Image: Shutterstock
Motherhood is an exciting experience, and if this is the first time, it is common that you will have many questions about it. The following post will discuss ‘how is breast milk made?’ During pregnancy, several changes happen inside your body to prepare the baby and nurture them after birth. One such change is the beginning of lactation after your baby is born. Learn how it happens, from when the milk is produced inside the body, how it is produced, and more. Read on to know more about the phenomenon of milk production inside the human body and some interesting facts related to it.
Key Pointers
- During pregnancy, progesterone and estrogen (ovarian hormones) regulate breast size and prepare the breasts for milk production.
- Each breast nipple contains small milk ducts and lobules that produce milk.
- Colostrum, also known as “first milk,” starts being produced in the 16th week of pregnancy.
- The release of milk into the ducts is triggered by oxytocin, which is produced in the brain and causes the milk let-down reflex.
- Milk production usually begins 3 to 5 days after delivery.
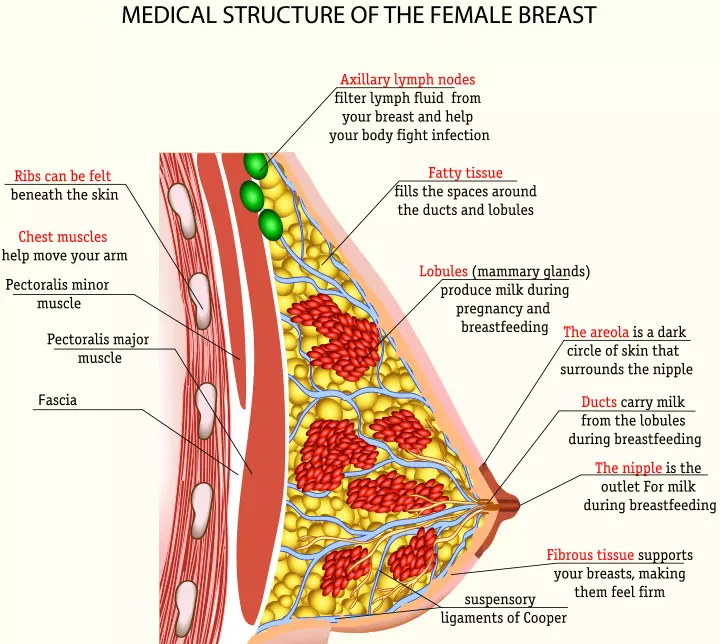
Anatomy Of The Breast
To understand the production of breast milk, you need to understand the anatomy of the mammary gland and how they function (1).
- Each nipple has 15-20 tiny outlets for the lactiferous ducts that carry milk from the lobules to the nipples.
- The milk lobules produce milk within the breasts. They form clusters that are called lobes, and a healthy breast can contain about 12 to 20 such lobes (2).
- The Montgomery glands or areolar glands are the sebaceous glands on the nipple that produce oil to lubricate it. The oil has anti-bacterial properties that keep the nipple clean and free of bacteria. It is also believed that the oil gives out a fragrance that helps the baby easily detect the nipple while breastfeeding.
- You may notice your nipple and areola getting larger during pregnancy and throughout your lactation state. The color of the areola and nipple also gets darker. It is mainly to make it easier for the baby to see the nipple. Hence, the breast anatomy tends to change with pregnancy and motherhood.
The Beginning Of Milk Production
The mammary glands start preparing for lactogenesis right from the moment you conceive. Keep reading to know how.
Ovarian hormones influence breast size and shape: Ovaries produce the hormones progesterone and estrogen. These nursing hormones have a significant influence on how your breasts appear and how the milk lobules within it function. Milk production occurs within the clusters of alveoli within the breast. When you ovulate, estrogen creates new branches of milk ducts, which will carry the milk from the lobes to the nipple.
Progesterone increases the size and number of milk lobules to prepare the breasts for the production of milk. The hormone also increases the supply of blood to the breasts. All this makes you experience fullness and tenderness of breasts during menses (3).
Your first milk production begins in the second trimester: The effects of progesterone and estrogen wear out if you do not get pregnant during the menstrual cycle. Otherwise, the effects of these hormones remain, and the body further prepares the breast for lactation. As your pregnancy progresses, the breasts continue to change.
The nipples, areola, and the areolar glands grow larger and become more prominent than ever. By the 16th week, the breasts begin the production of colostrum, otherwise known as the “first milk.” The yellow-colored colostrum is also referred to as liquid gold due to its yellow color, as it is rich in nutrients, antibodies, and fat globules. The body produces more than enough of it as you near full term, causing it to leak a little during late second trimester, although some mothers may never leak colostrum during pregnancy. This is also considered to be normal (4) (5).
Breasts are ready for lactation by the end of pregnancy: By the end of your pregnancy, the milk lobules inside the breasts are capable of handling round-the-clock milk production typically 50-73 hours or 3 to 5 days after delivery of the baby and placenta.
How Is Breast Milk Produced?
Once the baby has ingested the colostrum, the breasts will produce the first batch of milk. The following are the steps involved in the production of milk after the birth of your baby:
1. Prolactin takes over:
- After delivery, there is a drop of the hormones in the body since the uterus shrinks and the placenta is removed. Then, the hormone prolactin, which is produced by the pituitary gland inside the brain, takes over the milk production (5) (6).
- Breast milk composition is fundamentally water, proteins, fatty acids, sugars, lactose, micronutrients, and antibodies. Prolactin stimulates the milk lobules to source these building blocks of milk from blood vessels. Once the milk lobes obtain these building blocks, they combine it all through a complex biochemical process to create milk. Prolactin ensures that both the breasts produce milk.
- The effects of prolactin kick in about three to five days after the birth of the baby. By this time, your baby would have drunk all the colostrum, and prolactin would have stimulated the milk lobules to produce a fresh batch of milk.
 Quick fact
Quick fact2. The milk let down:
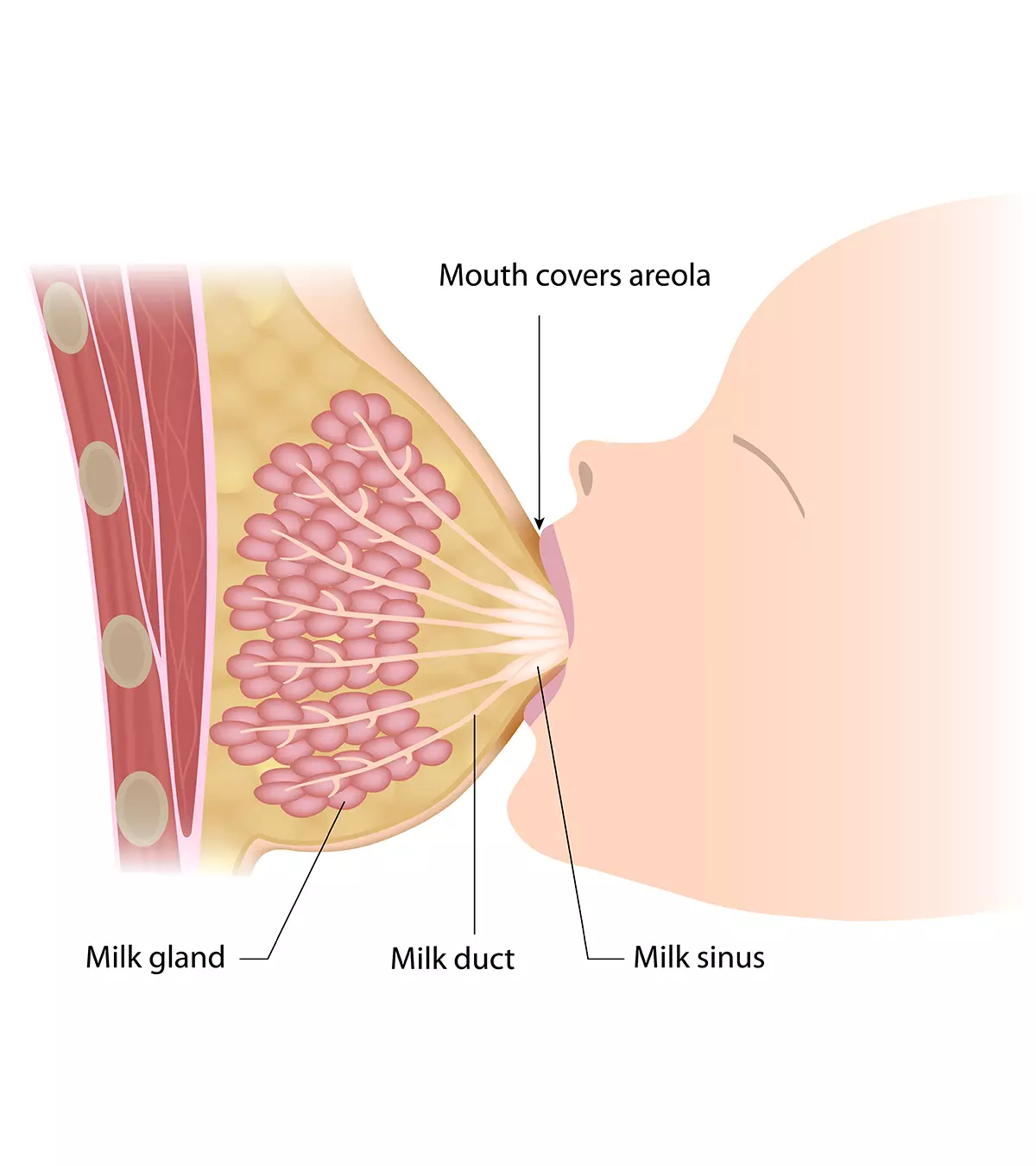
- While prolactin stimulates the milk lobules, the hormone oxytocin is responsible for letting out the milk from the lobes into the ducts from where they can flow out through the nipple.
- Oxytocin is produced in the hypothalamus region of the brain, which is close to the pituitary gland that produces prolactin (7).
- Oxytocin makes the milk lobes contract and releases the milk into the milk ducts, from where it passes through the nipple. It is the milk ejection or let-down reflex that causes your body to push the milk to the nipple when your baby suckles to feed. This nipple stimulation causes some mothers to feel a tingling sensation with their milk let-down. Others do not ever feel it, but hear their infant starting to swallow actively. There is more than one let-down in a breastfeeding session, although it may or may not be noticeable to the mother.
 Quick fact
Quick fact3. Suckling stimulates more milk production:
Image: Shutterstock
- Constant stimulus from your baby’s suckling and emptying of the breast enable prolactin and oxytocin to work towards production and let-down of milk respectively.
- Other factors such as the baby’s crying or cuddling the baby skin to skin – may help trigger the let-down reflex.
- Over a period, when the baby relies less and less on breast milk, the brain senses that the breasts are emptied less often than before. This brings down the production of breast milk and limits it to only as much as your baby drinks. In other words, “Supply=Demand.”
Breastfeeding gives infants the best nutrition and helps create a special bond between mother and child. When you are healthy, milk synthesis goes on smoothly. Sometimes, there could be trouble producing the necessary amount of milk for various reasons. This is when you should always seek the help of a Board Certified Lactation Consultant, if available.
Can There Be Problems In Milk Production?
Image: IStock
Yes, you may experience problems with the production or the let-down of the milk due to the below reasons:
- Fatigue: The days after childbirth are perhaps the most stressful for a mother. Fatigue and stress can interfere with the production of oxytocin and may slow down the let-down reflex. Sharing baby duties with your partner and taking some time to rest are the best ways to prevent the onset of fatigue.
- Painful distractions, such as uterus cramps: Oxytocin also causes the uterus to contract after childbirth. This is good, because it prevents the mother from bleeding too much after delivery. However, contractions can cause uterine cramps that could be distracting and may interfere with your ability to feed your baby in peace. The cramps will subside as the uterus gradually attains its regular shape and you will start feeling better.
- Rapid, unrelieved breast engorgement: Engorgement of breasts 3-5 days after delivery can make feeding painful. However, the breasts become less engorged as you feed the baby, creating an outlet for the milk to flow out.
- Poor latch and inability to feed: If the baby has difficulty latching to the nipple, then they may not get sufficient milk. It keeps the breast full, which in turn could signal the brain to reduce the production of prolactin, which eventually brings down the milk supply.
Listen to the suckling and swallowing sounds to know your baby is feeding. Look for a calm place to feed the baby. Stay relaxed while feeding for a better let-down reflex. Feel for a softer breast and look for your baby to be relaxed and satisfied when feeding is finished.
Amber, a mother of three, reflects on her breastfeeding journey with her twin baby girls, “I found that Parker and Jolie (her twins) needed a lot of practice nursing. They had small mouths and worked really hard at the breast for the first couple of weeks, but eventually, they figured it out, and they were ‘sucking’ pros! Once I became confident in my supply, my ability to nourish, and Parker and Jolie’s satiety, I was more confident in facing any issue (low supply, supplementing with formula, or a nursing strike) I would have had later on (i).”
Read on for tips on how to prepare for breastfeeding.
How To Prepare Breasts For Feeding?
Image: Shutterstock
Relaxing usually alleviates any problems caused during milk production and let-down. The following techniques may also help you achieve let-down (8):
- Take a warm shower: A warm shower allows you to relax, to stimulate the production of oxytocin that enables easier milk flow from the nipple.
- Wrap the breasts in a warm towel: Place a towel soaked in warm water on your breasts for a few minutes before feeding. It has the same effect as a warm shower.
- Massage the breasts: It will stimulate milk flow from the lobes towards the nipple.
- Relaxation through other methods: Listening to soothing music, going for a walk or taking a nap are some of the ways to feel calm and less stressed before the breastfeeding session.
 Quick tip
Quick tipFrequently Asked Questions
1. What foods boost the supply of breast milk?
Breastfeeding women should eat a well-balanced diet containing different foods from all the food groups. You should also take healthy beverages to stay hydrated. Also, limit alcohol and caffeine consumption (9). According to the Institute of Medicine of the National Academies, you should drink around 2.7 liters of fluid daily. If you’re concerned about your milk supply, consult a lactation specialist who can advise on foods that increase breast milk and other strategies to support lactation.
2. Why does breast milk look white?
Breast milk looks white because of its fat content. Therefore, foremilk produced at the beginning of the feed looks bluish-gray as it contains less fat, while the hindmilk produced toward the end looks creamy white because of its high-fat content (10).
3. How long can breast milk be stored?
Freshly expressed milk can be stored (11):
- At room temperature for around four hours
- In the refrigerator for around four days
- In the freezer for around six months (although using the milk for up to 12 months is acceptable)
Understanding “how breast milk is produced” could clarify the queries on the breast changes during lactation. In addition, while learning about breast milk production, you learn about the intervening factors that come into play. This is beneficial as it helps you differentiate the myths from the facts about breastfeeding. The knowledge of breast milk production could also help you understand how a baby latches themselves while feeding. Also, if you have other queries, you can always seek the help of a lactation consultant.
Infographic: Common Misconceptions About Breast Milk
Breast milk nourishes the baby and supports their growth and development. However, a lot is said and believed about breast milk and its production during and after pregnancy. Our infographic brings you a list of some common misconceptions associated with breast milk. Read through these myths that are prevalent in many parts of the globe. Illustration: Momjunction Design Team
Illustration: How Is Breast Milk Made During Pregnancy & Interesting Facts
Image: Dall·E/MomJunction Design Team
Discover the amazing journey of breast milk production, from pregnancy to feeding your baby from this informative video!
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Breast feeding, pumping, & being a working mom.https://themasseyspot.blogspot.com/2014/05/breast-feeding-pumping-being-working-mom.html
References
1. Breast Milk Production; Sutter Health Network
2. Breast Anatomy; National Breast Cancer Foundation
3. Breast Anatomy;Cleveland Clinic
4. Changes in the breasts; The Open University
5. Reviewed by L Adler, D Freeborn; How Breastmilk is Made; University of Rochester
6. Reviewed by D Zieve, I Ogilvie et al.; Prolactin blood test; US National Library of Medicine, Medline Plus
7. S K Fineberg, D A Ross; Oxytocin and the Social Brain; Biol Psychiatry (2017)
8. Ten Valuable Tips for Successful Breastfeeding; Government of Canada
9. Are There Breastfeeding Superfoods That Help Increase Milk Production?; Cleveland Clinic
10. Infant and Young Child Feeding: Model Chapter for Textbooks for Medical Students and Allied Health Professionals; National Library of Medicine
11. Breast Milk Storage and Preparation; Centers for Disease Control and Prevention
12. How Breast Milk Is Made; USDA WIC Breastfeeding Support
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Jill Lancaster
Read full bio of Swati Patwal
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny