Autoimmune diseases in children may be linked to genetic, environmental, and hormonal factors. An autoimmune condition might develop when our immune system misinterprets and attacks healthy cells or tissues in the body as antigen or foreign bodies. Around 80 autoimmune diseases are present; however, not all can affect children (1). There may not be specific signs and symptoms in autoimmune illnesses, and doctors may do some tests to exclude other possible conditions while diagnosing.
Read on to know more about the causes, symptoms, and management of autoimmune diseases in children.
Key Pointers
- Localized autoimmune diseases affect a specific organ, while systemic autoimmune diseases can impact multiple organs.
- Autoimmune diseases may result from hereditary, genetic, hormonal, or environmental factors.
- Children with autoimmune diseases may experience symptoms such as internal organ infection or inflammation, delayed growth and development, anemia, prolonged fever, and general discomfort.
- Diagnosis of autoimmune diseases can be complex, and it may involve physical examination, medical history, and tests such as antinuclear antibody tests.
- Although autoimmune diseases have no cure, supplements, blood transfusions, physical therapy, intravenous immunoglobulin, and surgery can assist in managing them.
15 Autoimmune Diseases In Children
These diseases fall into two categories, namely localized and systemic. Localized diseases affect a particular organ such as liver, thyroid, and adrenal glandsiSmall triangular-shaped glands on kidneys that help produce hormones. , while systemic autoimmune diseases spread to multiple organs from skin to kidneys and heart. The disorders can affect any part of your child’s body, including:
- Blood vessels
- Connective tissues
- Endocrine glands such as the thyroid or pancreas
- Joints
- Muscles
- Red blood cells
1. Addison’s disease
It is also called pediatric adrenal insufficiency, and it occurs when the adrenal glands do not produce sufficient cortisoliA steroidal stress hormone that helps regulate the body's response to stress. and aldosteroneiA steroid hormone responsible for the regulation of sodium, potassium, and high blood pressure. . These hormones regulate the child’s metabolism, immune system, and the levels of sodium and potassium in the body (2). Addison’s disease is rare.
2. Psoriasis

Image: IStock
Itchy, dry patches on skin could point towards psoriasisiAn autoimmune disorder that makes the skin itchy and scaly. . This could be due to an autoimmune condition or caused by a bacterial infection on the skin. Psoriasis in children can often be attributed to genetics or other autoimmune diseases such as Crohn’s Crohn’s diseaseiA chronic condition causing inflammation of the digestive tract. , type I diabetes, and Rheumatoid Arthritis. This disease causes inflammation and along with skin may involve joints as well (3).
3. Autoimmune liver disease
It is also known as autoimmune hepatitis. It is an inflammatory disorder that damages the liver and can lead to cirrhosisiA severe condition characterized by chronic or permanent liver damage that may occur due to scarring of the liver. , if it progresses. Type I is less common in children. Type II, too, is rare but more common than type I. It usually affects girls of two to 14 years of age (4).
4. Autoimmune thyroiditis (AT)
Autoimmune thyroiditis usually occurs in adolescents, but can present even in younger children. This is a common acquired cause of thyroid disease in children. AT can be either hypothyroidismiA condition in which the thyroid gland fails to produce sufficient thyroid hormone. or hyperthyroidismiA condition in which the thyroid gland produces excessive thyroid hormone. . Genes and environmental factors cause the disease in children (5).
5. Celiac disease
This digestive disorder affects the small intestine and is triggered in genetically predisposed children if they eat foods such as wheat, barley, rye, and cooked food containing the protein gluten. One in 141 people in the US have this disorder, but most remain oblivious to it (6). According to a study that the Pediatric Gastroenterology-Hepatology and Nutrition conducted, it was estimated that approximately 95% of Celiac patients remain undiagnosed. Girls are more vulnerable than boys, and it can also be hereditary.
6. Henoch-Schonlein purpura (HSP)
In an HSP affected child, the inflamed skin leaks red blood cells causing rashes in the legs, buttocks, and arms. The condition can also target the internal organs. In the US, HSP occurs in 20 per every 100,000 children, and boys are more vulnerable than girls. This kind of autoimmune rashes in children can develop between two and 11 years of age (7).
7. Immune (or idiopathic) thrombocytopenia purpura (ITP)
In this condition, the immune system destroys the platelets (blood cells that help in clotting of blood) in the child’s body, mostly in the spleen (8). Therefore, when their count is low, bleeding could become uncontrollable. Medical practitioners are yet to know the cause of the condition, sometimes, it could also be the result of a non-contagious virus. Also, ITP could occur if the child has any other autoimmune disorders.
8. Juvenile arthritis (JA)

Image: IStock
Also called pediatric rheumatic disease, JA can affect children aged below 16 years. Nearly 300,000 children in the US are affected with this condition (9). JA is a collective name given to various rheumatic diseases in children, affecting different body parts from the musculoskeletal system to eyes, skin, muscles, and gastrointestinal tract.
9. Juvenile dermatomyositis
Juvenile dermatomyositis is an inflammation of muscles (myositis), as the faulty immune system attacks blood cells throughout the child’s body. The condition is very rare as three in one million children are affected in the US every year (10). It mostly occurs in children of five to ten years of age.
 Point to consider
Point to consider10. Juvenile scleroderma
This autoimmune disease is characterized by the formation of thick skin patches due to the excess production of collagen. There are two types, localized scleroderma which affects only the skin, and systemic scleroderma where, in addition to the skin, internal organs such as kidneys, heart and gastrointestinal tract are affected.
Girls are more vulnerable than boys. The US has just about 5,000 to 7,000 children suffering from this rare disease. Among those affected, 1.5% get it before 10 years of age while 7% develop it between 10 and 19 years (11).
11. Kawasaki’s disease
The rare disease occurs due to inflammation of the muscles in the body, and when left untreated, it might affect the coronary vessels in the heart. It starts with a fever, a skin rash and swollen lymph nodes in the neck, which continues for around five days. Children aged below five years are susceptible, and one in 10,000 children are affected (12).
12. Pediatric lupus (SLE)
Systemic lupus erythematosus or lupus happens in many forms and damages joints, skin, kidneys, heart, lungs, blood vessels, and brain among other organs. The disease is uncommon in children below five years, but 15% of those affected by the disorder are younger than 18 years (13).
13. Type 1 diabetes (juvenile)

Image: IStock
Type 1 diabetes is an autoimmune disease where the pancreas stops producing insulin hormone. The disease can develop at any age but is more common in people aged below 20 years. Over 304,000 youth below 20 years are estimated to be suffering from this disease in the US (14).
Betsy Boehm Bland, a mom, shares her experience of her five-year-old daughter suffering from Type 1 diabetes, “We’ve dealt with the complex emotions that accompany a life-long battle to keep a child alive. We even set alarms to wake up one to two times a night to check blood levels in case she was going dangerously low. We learned how to draw up and give injections for the first time in our lives. Reminded me of changing diapers — scary and awkward in the beginning, then feels like no big deal in a short amount of time (ⅰ).’’
14. Multiple autoimmune syndrome (MAS)
MAS is the combination of three or more autoimmune diseases in a person. One of the disorders pertains to skin – either scleroderma or psoriasis. Around 25% of the people suffering from an autoimmune disease are likely to get more autoimmune disorders (15).
Multiple Sclerosis (MS) and Ulcerative Colitis (UC) are two other autoimmune diseases that can affect children (16) (17).
15. PANDAS Autoimmune Disorder
Pediatric Autoimmune Neuropsychiatric Disorders Associated with Streptococcal Infections or PANDAS is a condition thought to be triggered by a streptococcal (strep) infection, such as scarlet fever or strep throat. Around 1 in 200 children in the United States alone are thought to be affected by PANDAS, according to a conservative estimate (18). In PANDAS, the body’s immune system, which normally fights off infections, mistakenly targets and attacks certain cells in the brain, leading to neuropsychiatric symptoms. These symptoms often emerge suddenly and dramatically, appearing out of nowhere. These can include either motor or vocal tics, or both, and may also exhibit compulsions, obsessions, or both. Alongside these symptoms, children may experience changes in mood or become irritable. Anxiety attacks could also occur, and they might express concerns about being away from their family. The exact mechanisms behind this process are not fully understood, but it is believed that molecular mimicry might play a role (19)(20).
Autoimmune disorders can target any part of our body. And why do they do so? Unfortunately, the medical fraternity is yet to understand the exact cause for these immunological diseases and conditions.
Why Do Some Children Have Autoimmune Diseases?
Autoimmune diseases are ‘idiopathic’ meaning that their cause is unknown. However, based on some common traits, scientists believe that a combination of multiple factors causes the diseases:
- Heredity: The autoimmune problems could pass on to a child from parents. Also, if a woman is carrying an autoimmune disorder when she is pregnant, she could pass on the antibodies to the child in the womb. In such cases, the symptoms may disappear in a few months (21).
- Genetic: According to the US National Institutes of Health (NIH), genetic studies show that people with autoimmune diseases possess unique gene variations (22), which means defects in genes could also be a cause of autoimmune diseases.
 Quick fact
Quick factSo while genes make an individual susceptible, environmental factors may act as triggers for various autoimmune diseases.
- Hormonal effects: Medical experts assume that hormones in our body influence disorders because several autoimmune problems occur in women than men. The female immune system has a stronger response to infections and vaccinations which comes with a side-effect of higher susceptibility to autoimmune diseases (23).
- Environmental factors: The disorders generally remain dormant until some external elements, such as sunlight, virus, a drug, radiation, diet high in fat, sugar might trigger them. For instance, a virus can enter the body and alter the cells, which could make the immune system attack the body (24).
Note: Studies are still ongoing to identify the genes that cause pediatric immune disorders, environmental and hormonal factors influencing them.
Symptoms Of Autoimmune Diseases In Children
There are no specific symptoms that can be associated with these disorders. Most of the time, symptoms depend on the organs involved. However, the most prevalent symptoms and signs are:
- Infection and inflammation of internal organs
- Cramps, loss of appetite, diarrhea, nausea and other digestive problems
- Delayed growth and development
- Prolonged fever
- Anemia or low platelet counts
- Frequent sinus infection, pneumonia, bronchitis
- Joint pain and swelling
- Ear infections
- MeningitisiInflammation of the fluid and protective membranes around the brain and spinal cord.
- Skin infections
- General ill-feeling (malaise)
- Rashes
- Dry eyes and mouth
- Hair loss
- Weight loss
- Tiredness
All the above symptoms are non-specific in the sense that they need not necessarily point at an autoimmune disorder but could be a simple, temporary health problem.
Note: Most of the symptoms like fatigue, swelling, and rashes come occasionally and go away. However, if your child is suffering from these symptoms frequently, it could be indicative of a health problem. In such cases, take them to a pediatrician for further analysis and diagnosis.
Diagnosis Of Degenerative Autoimmune Diseases
Diagnosis is a challenge for doctors as the symptoms are not unique to autoimmune disorders.
However, an early diagnosis can significantly impact the management and progression of the autoimmune condition in children, thus resulting in a better prognosis. The doctor would initially do a physical examination and understand the child’s medical history. Later, they may recommend various tests based on the affected organs:
Antinuclear antibody tests: Antinuclear antibody (ANA) test is the primary test done to diagnose autoimmune disorders. ANA are the autoantibodies that attack the matter present in the nucleus of a cell.
ANA test is done using two methods, indirect fluorescent antibody (IFA) and immunoassay. In IFA, the affected child’s blood sample is combined with cells. If antibodies are present in blood, they react with the cells. Immunoassays are less accurate than IFA (25).
The doctor may recommend other autoantibody tests along (26) with ANA, to observe specific substances within cell nuclei.
- CBC: The complete blood count (CBC) test gives details about three components, red blood cells, white blood cells, and platelets.
- Comprehensive metabolic panel: CMP is a blood test done to check for anomalies in the kidney, liver, and diabetes.
- C-reactive protein: The CRP test is done to screen inflammatory bowel disease, rheumatoid arthritis, and lupus.
- Erythrocyte sedimentation rate (ESR): This is a non-specific test because it identifies inflammation in the body but does not specify the organ in which the anomaly exists.
- Urinalysis: Urinalysis involves several tests to examine the physical, microscopic, and chemical appearance of the child’s urine.
 Things to know
Things to knowOnce the doctor diagnoses the cause and understands the severity of the problem, he will recommend certain changes in the child’s diet and routine if the disorder is minor or temporary.
So, would those minor changes be enough to address the problem? No, serious diseases need medical intervention.
Ways To Manage Autoimmune Diseases In Children
These methods cannot cure autoimmune diseases, as there is no cure for them. The available options aim at reducing the symptoms, controlling the damage done by autoimmunity, and maintaining the body’s ability to fight the disease.
Each childhood autoimmune disease has unique management steps but commonly include (26) (27):
- Supplements: Your physician may prescribe supplements to replenish the vitamins, hormones (such as thyroid), or insulin in the child’s body.

Image: Shutterstock
- Blood transfusion: In the case of disorders such as ITP, very rarely your child may need a blood transfusion as the body produces less blood or fewer platelets, among other things.
- Physical therapy: Diseases related to bones, joints, or muscles need physical therapy to make the body parts move easily and strengthen the muscles.

Image: Shutterstock
- Nonsteroidal anti-inflammatory drugs: The NSAIDs or painkillers, such as ibuprofen and naproxen, give relief from swelling, pain, and stiffness. They suppress the inflammatory pain caused due to some diseases such as rheumatoid arthritis.
- Disease-modifying anti-rheumatic drugs (DMARDs): These drugs slow down the rate at which the disease is progressing. These are commonly used for rheumatoid arthritis, to alleviate pain and inflammation, and control joint damage.
- Biologics: Biologics are a new class of drugs that are genetically engineered proteins. They target the specific organs attacked by the immune system. They are DMARDs used for patients with persistent disease activity.
- Corticosteroids: Corticosteroids are hormones produced by the adrenal glands. They are available in various forms, including tablets, injections, inhalers, and lotions. The drugs used to fight inflammation and control the immune system are so powerful that doctors prescribe them only in small doses. High doses are likely to have long-term side effects. Prednisone is one such corticosteroid.
- IVIg (intravenous immunoglobulin): IVIg is an immunoglobulin G antibody pooled from multiple plasmas collected from multiple donors. They help in controlling idiotypic antibodies and mitigating inflammatory mediators, among others (28).
Depending on your child’s autoimmune disease, they may need other kinds of medical treatment, such as:
- Plasmapheresis: It is a physical process to remove plasma. Plasma carries antibodies in the blood. The doctor would recommend the procedure only in extreme cases as plasmapheresis flushes good antibodies as well.
- Surgery: In certain complicated cases of juvenile idiopathic arthritis or bowel obstruction in Crohn’s disease, doctors may recommend surgery.
- Stem cell transplantation: Autologous hematopoiesis stem cell transplantation (AHSCT) has been found to be effective in treating refractory autoimmune diseases in children (35).
- Biologic therapies: New biologic therapies may be used to target specific pathways. For instance, the doctor may suggest CAR-MSCs therapy, an immunotherapy strategy that combines chimeric antigen receptors (CAR) with mesenchymal stromal cells (MSC) to develop engineered stem cells called CAR-MSCs (36).
The pain, inflammation, and the trouble associated with the conditions could be traumatic for the child. Along with medication and physical therapy, he might need psychotherapy or counseling to be strong during these testing times.
In addition to taking the child to the doctor, what can you do? Support the child by taking precautions such as giving an allergen-free diet, nutritional supplements like vitamin B and C, and healthy lifestyle changes.
Autoimmune diseases in childhood occur as the immune system fails to differentiate between an individual’s body and foreign antibodies. They can attack any one or multiple organs. While a few could be long-term disorders, some might disappear in a few days. As a parent, you need to be strong and make your child feel as normal as possible lest it affects her psyche. Take care of her routine, and food consumption to make the problem less worrisome.
Frequently Asked Questions
1. What is leaky gut syndrome?
Inflammation creates large spaces in between the cells bordering the intestines. They become leaky and allow toxins, bacteria, bad fats, and other unhealthy materials to seep into the bloodstream through the gut membrane. In short, a leaking gut wall invites the toxic substances into our body, triggering the immune system to become hyper-defensive. The symptoms of many autoimmune diseases might get agitated with leaky gut syndrome (29).
2. Is cancer an autoimmune disease?
According to Cancer Research UK, there is no direct connection between autoimmune diseases and cancer. A person with autoimmune disorders is as likely as a normal person to get cancer. However, certain types of cancer are more likely to happen in people with particular autoimmune diseases.
For instance, researchers at the Medical College of Wisconsin have found that systemic sclerosisiAbnormal thickening of the tissues and organs of the body. increased the risks for lung cancer by five times, liver cancer by three times, and nonmelanoma skin canceriSkin cancer that starts in the skin cells other than melanocytes (melanin-producing cells). by four times (30).
According to a study in Shanghai, the risk of esophageal cancer increased 2.4 fold in patients with autoimmune diseases.
3. Which specialist doctor treats autoimmune diseases?
Take your child to a pediatrician. He will be the main doctor, who would suggest the specialist or specialists you need to visit. For example, if your child has an autoimmune problem with
- Digestive system: gastroenterologist;
- Kidneys: Nephrologist
- Joints and connective tissue disorders: Rheumatologists
4. Can a child outgrow autoimmune disease?
Autoimmune diseases are considered to last long, if not a lifetime. Some children may outgrow the condition, and for other diseases, the symptoms may cease to recur after treatment. Even then, the status must be continuously monitored as recurrence is possible (26).
5. What happens if autoimmune disease is left untreated?
Leaving an autoimmune disease untreated can pose a severe health risk. They are chronic illnesses and are the leading cause of mortality and morbidity (31). Symptoms can aggravate rapidly, and hence timely medical attention is recommended.
6. What foods help autoimmune diseases?
Following an anti-allergenic and anti-inflammatory diet has proven beneficial in people with autoimmune diseases. Foods rich in antioxidants, phytochemicals, nutrients, and fiber, like whole fruits and vegetables, legumes, nuts and seeds, and some seafood, combat inflammation by inhibiting signaling pathways (32). Modify your diet under the guidance of a registered nutrition professional or your healthcare provider.
Autoimmune diseases in children may be caused by hormonal changes or hereditary, genetic, and environmental factors. They may affect different body parts. For example, psoriasis affects the skin, while celiac disease affects the small intestines. The symptoms depend on the organ affected; however, some common symptoms are skin infections, joint pain, and hair loss. Presently, there is no cure for autoimmune diseases, but they can be managed with supplements, corticosteroids, physical therapy, blood transfusion, and other methods. If you are dealing with an autoimmune disease, consult a doctor to devise an effective treatment plan to help you manage the disease well and lead a comfortable life.
Infographic: What Can Cause Autoimmune Diseases In Children
Autoimmune disorders lack a definitive cause and cure; however, several factors may contribute to their development. Explore the infographic below to learn the various notable causes and factors behind autoimmune diseases in children.
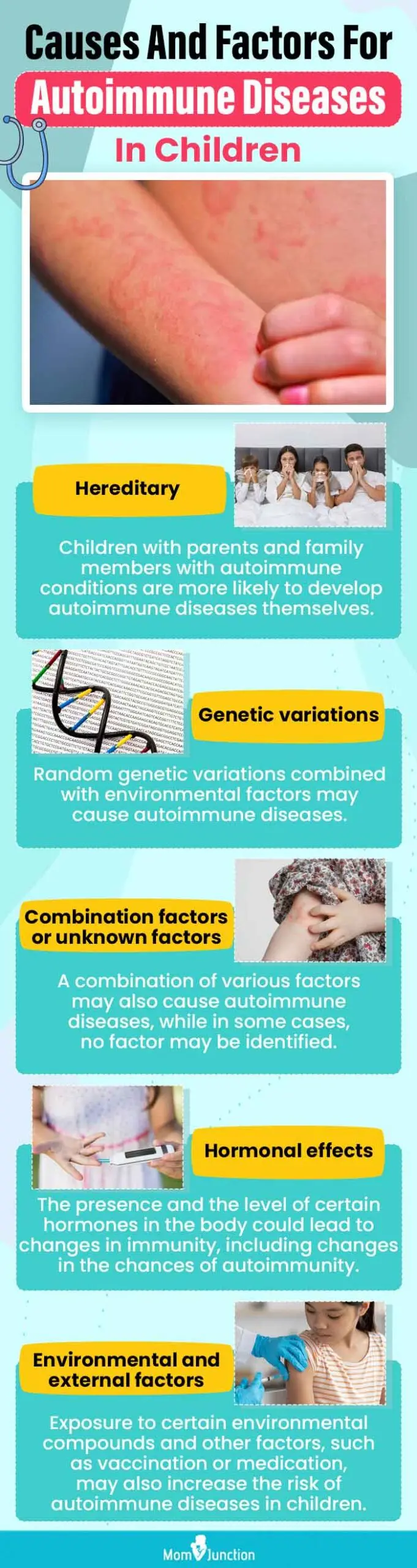
Illustration: Momjunction Design Team
Illustration: Autoimmune Diseases In Children: Causes Symptoms & Treatment

Image: Stable Diffusion/MomJunction Design Team
Learn how to help your child manage autoimmune diseases. Explore the multiple benefits of adopting a plant-based diet and its potential to improve your child’s overall health and well-being.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
ⅰ. Happy diaversary! Surviving the first year with Type 1 diabetes.https://betsyboehmbland.medium.com/happy-diaversary-surviving-the-first-year-with-type-1-diabetes-5c261f5d2e13
References:
[editor_policy_text]
1. Autoimmune disorders; Medline Plus; US National Library of Medicine
2. Addison Disease in Children; University of Rochester Medical Center
3. Adriana Rendon and Knut Schäkel; Psoriasis Pathogenesis and Treatment; NCBI(2019)
4. Autoimmune Hepatistis; Cincinnati Children’s Hospital
5. Rosalind S. Brown; Autoimmune Thyroiditis in Childhood; NCBI(2013)
6. Definition & Facts for Celiac Disease; National Institute of Diabetes and Digestive and Kidney Disease
7. IgA Vasculitis (Henoch-Schönlein Purpura); Cleveland Clinic
8. Immune thrombocytopenic purpura (ITP); Medline Plus; US National Library of Medicine
9. Juvenile Arthritis; Arthritis Foundation
10. Juvenile Dermatomyositis; American College of Rheumatology
11. Pediatric Systemic Scleroderma; Cleveland Clinic
12. Kawasaki disease; National Institute of Health
13. Lupus | Symptoms & Causes; Boston Children’s Hospital
14. National Diabetes Statistics Report; CDC
15. M Cojocaru, et al.; Multiple autoimmune syndrome; NCBI(2010)
16. Pediatric Multiple Sclerosis; Cleveland Clinic
17. Pediatric Ulcerative Colitis; Yale Medicine
18. PANDAS/PANS Prevalence; PANDAS Network
19. PANDAS & PANS – Autoimmune Disorders in Children; South Carolina Department of Health and Environmental Control
20. PANDAS—Questions and Answers; NIH
21 Kristina M. Adams Waldorf, and J. Lee Nelson; Autoimmune Disease During Pregnancy and the Microchimerism Legacy of Pregnancy; NCBI(2008)
22. NIH researchers reveal link between powerful gene regulatory elements and autoimmune diseases; National Institute of Health
23. Vaishali R. Moulton; Sex Hormones in Acquired Immunity and Autoimmune Disease; NCBI(2018)
24. Environmental Contributors to Autoimmune Disease: Mechanisms, Impacts, and Chemicals of Concern; Collaborative on Health and Environment
25. Antinuclear Antibody (ANA); labtestsonline
26. Autoimmune Diseases | Diagnosis & Treatment; Boston Children’s Hospital
27. Autoimmune Diseases; Better Health Channel
28. Bayry J, et al.; Mechanisms of action of intravenous immunoglobulin in autoimmune and inflammatory diseases; NCBI(2003)
29. Qinghui Mu; Leaky Gut As a Danger Signal for Autoimmune Diseases; NCBI(2017)
30. Nancy Volkers; Do Autoimmune Diseases Raise The Risk of Cancer?; Journal of the National Cancer Institute
31. Michael D. Rosenblum, et al.; Treating Human Autoimmunity: Current Practice and Future Prospects; NCBI(2014)
32. Diet Review: Anti-Inflammatory Diet; The Nutrition Source; Harvard T.H. Chan School of Public Health
33. Juvenile Dermatomyositis; Cleveland Clinic
34. What Are Common Symptoms Of Autoimmune Disease? Johns Hopkins Medicine
35. Özlem Satirer et al.;Autologous haematopoiesis stem cell transplantation (AHSCT) for treatment-refractory autoimmune diseases in children; RMD Open (2024)
36. Scientists pioneer immunotherapy technique for autoimmune diseases; ScienceDaily
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Garima Garg Seth
Read full bio of Dr Bisny T. Joseph
Read full bio of Swati Patwal
Read full bio of Anindita Ghatak