
A gestation of 39 to 40 weeks is regarded as a full-term pregnancy. Therefore, your little bundle of joy may be due anytime as soon as you complete the 40th week of pregnancy. However, some women may experience the onset of labor before completing these nine months, while some may not experience any such signs even during the 40th week.
This post explains the symptoms and signs you may experience in the 40th week of pregnancy, the changes that occur in your body and that of your baby, and tips to help you cope with labor. Also, we address some of the frequently asked questions related to the 40th week of pregnancy.
Key Pointers
- Pregnant women at 40 weeks may experience aches, pelvic pressure, lightening, false contractions, and frequent urination.
- At this stage, the baby is full-term, measuring around 50cm in length, and weighing approximately 3.5kg.
- Mucus discharge, lower back pain, abdominal cramps, and amniotic sac rupture may indicate the onset of labor.
- Inducing labor may be considered by the doctor after examining the health status of the mother and baby during the last prenatal visit.
What Are The Pregnancy Symptoms At 40 Weeks?
In the 40th week of pregnancy, you might have the below symptoms (1) (2) (3) (4):
- Pelvic pain and discomfort: The baby goes down further, putting more pressure on the pelvis and thus causing pain and discomfort. Moreover, the head movements of the baby inside the womb will give you sharp pain in the pelvic area.
- Lightening: With the baby moving down, the pressure from your ribs is released. This helps you breathe easier and relieves heartburn.
- Braxton Hicks: The false contractions become more frequent, and you might mistake them to be real labor. If you are getting Braxton Hicks contractions regularly, your doctor may do a vaginal examination to look for signs of cervix dilation. This, in turn, helps you know if the contractions are real or false. The doctor may ask you to keep track of the time gap between contractions to know if they are false or true. True labor contractions differ from Braxton Hicks contractions by becoming more intense, more regular as time passes and they never disappear with rest.

- Vaginal discharge: A thick mucus plug is discharged through your vagina as the baby pushes down to the birthing canal. This vaginal discharge could be white and clear or tinged with blood appearing slightly pinkish. This is called the bloody show.
- Painful leg cramps: You might experience them, especially at night. To ease the pain, you can gently flex your ankle and toes back towards the shin.
- Backaches: The pressure exerted by the baby’s head further into the pelvis and your postural changes could result in backaches.
- Insomnia: The discomforts will be at their peak, and you may feel fatigued due to lack of sleep. Getting a relaxing head massage can help you get proper sleep. You may also feel exhausted, especially as a result of weight gain and elevated hormonal levels.
- Low blood pressure: Hormonal changes cause the blood vessels to expand during pregnancy. The pressure put by the growing uterus on these expanded blood vessels reduce the blood flow to heart from the lower part of the body, causing a drop in the blood pressure.
- Varicose veins and hemorrhoids: The restriction in blood flow to the heart can cause the blood to pool in the leg veins and near the rectum, leading to varicose veins and hemorrhoids.
- Slowdown in fetal activity: As the baby reaches full-term, there won’t be enough space for him/her to move freely, thereby decreasing the movements.
- Frequent urination: The enlarged uterus puts pressure on your bladder, thus making you pee frequently. Also, an increase in the blood flow to the kidneys, and the relaxed urinary tract muscles (due to the increase in the progesterone level) result in frequent urination.

- Swelling: Severe swelling of hands, face, and feet is a common symptom noticed towards the 40th week. The increasing estrogen level causes water retention. To avoid the swelling, keep your feet raised over a plank. Circle both the ankles clockwise and anti-clockwise to ease the discomfort. Stretch your toes upward and downward. Walking regularly is also recommended to decrease swelling.
- Hot flashes: It is the most common symptom you may notice towards your due date. Wearing breathable maternity clothes and keeping yourself hydrated will help you stay cool.
- Early signs of labor: You are most likely to have labor contractions and water breaks this week. In such cases, call your doctor or visit the hospital.
- Morning sickness: Morning sickness is a common pregnancy symptom that can persist throughout the entirety of the pregnancy, including the 40th week
In addition to the pain and discomfort, you may witness some changes in your body this week.
In addition to the pains and discomfort, you witness some changes in your body this week.
Did you know?
- Only 5% of babies are born on their due date.
- The placenta triggers the hormones for milk production.
- Babies born at term can regulate their temperature better, effectively suck and swallow compared to babies born earlier.
- The first labor takes around 14 to 17 hours with the subsequent ones lasting for 6 to 8 hours (5) (6).
Changes In Your Body In Week 40
Here are some of the physical and emotional changes you may notice in the 40th week:
- Enlarged belly: The belly will be enormously large with the belly button sticking out. With this big belly, an expectant mother faces difficulty in walking and performing other regular activities.
- Stretch marks: The stretch marks become more prominent during this period. The US Office of Women’s Health (OASH) estimates that about twenty percent of pregnant women experience itchiness throughout pregnancy, primarily due to pregnancy hormones and skin stretching. Applying a moisturizing cream can help relieve the itchiness while pregnant.

- Nesting instinct: Colostrum (the first milk that breasts produce, usually yellow) begins to leak from the nipples.
- Cervix dilation: Your cervix starts dilating towards the later stage of pregnancy (7).
- Emotional changes: You might go through anxiety and impatience as you are worried about coping with delivery, infant care, and parenthood. Due to the hormonal changes, you may experience mood swings too.
Narrating her feelings on the 40th week of her pregnancy just before her induction day, a mother of four, Julia says, “Today started off really rough. I woke up at 12:30 a.m. to pee and again at 3:30 a.m. and could not get my brain to shut off— horrible thoughts swirling in my head, negativity, and anxiety in the wee hours of the morning. I know it’s awful to think this way, but I lost the mental battle of staying positive this morning.
“I worked on some belly picture montages, blog posts, etc. I was fine when I was distracted. And when the kids came down with Nate (her husband) later, he asked if I was alright, and I lost it. You know that feeling when you are in a funk but holding it together, and as soon as someone says, ‘Are you okay?’ you immediately start bawling? That was me. ‘Just frustrated and over it and tired?’ he asked. He tried to comfort me, saying he was proud of me for hanging in there and doing a great job carrying his son, which only made me roll my eyes because I don’t feel like I’ve done anything (such as birth the baby) other than ride an emotional roller coaster this past week (i).”
The physical changes mainly occur because your body is getting ready for the delivery, and your baby has grown big.
How Big Is Your Baby At 40 Weeks?
At 40 weeks, your baby reaches full-term and is about the size of a watermelon. The baby measures 19.68 inches (50 cm) from head to toe and weighs about 7.7 pounds (3.5 kg) (8).
Baby’s Development At 40 Weeks
Let’s see how fetal development has progressed over the past few months (2) (8) (9) (10) (11):
| Baby Organs | Development |
|---|---|
| Hair | Gets thicker and coarser |
| Nails | Grow longer |
| Lungs | Matured |
| Lanugo (thin bodily hair) | Disappears |
| Skull | Babies develop fontanelles (two soft spots) on the skull. It helps the skull bones to shift one over the other while the baby comes out of the birth canal. It also helps the brain grow further after the baby is born |
| Digestive system | The baby’s gut contains a green colored sticky substance called meconium. It forms the first fecal matter of the baby after birth. |
| Skills and reflexes | By this time, the baby develops 70 natural skills and reflexes that help them respond and react |
| Protective layer on skin | The baby’s body is covered with creamy coating called vernix caseosa |
The changes in your body and the baby are closely monitored during your regular visit to the doctor.
Your OB/GYN Visit

In addition to the regular check-ups, your final prenatal care visit might include the following tests:
- The physical test includes a pelvic examination to determine the cervical dilation (also called ripening), thinning, and softening. It helps the doctor to ascertain the expected time of labor.
- Amniotic fluidiThe fluid surrounding the fetus to aid in its protection and healthy growth. index (AFI) will be checked to measure the volume of amniotic fluid. The normal AFI value ranges from 5-25cm and for the third trimester the AFI value is around 7cm on average (12).
- The non-stress test (NST) measures the fetal heart rate and movements (13).
- A contraction stress test is done when the NST results are not normal. It helps in determining the response of fetal heartbeat during contractions.
- Biophysical profile test (BPP) is a kind of fetal well being test using an ultrasound. It detects the baby’s movements, breathing pattern, level of amniotic fluid and the body tone. This test is performed when NST produces unsatisfactory results or when there are conditions when fetal well being must be monitored.
Note: NST, CST, and BPP can be done at any time during the pregnancy. They will be done if you have health problems or your pregnancy is overdue (longer than 40 weeks).
During your last prenatal visit, your doctor will also discuss the possibility of your pregnancy getting over due to induction of labor or C-section. Most importantly, your OB/GYN will advise you to look out for the signs of labor.
Signs Of Labor In The 40th Week
Keep an eye on these signs, and contact your doctor accordingly (7):
Contractions get frequent and stronger with time.
- Light brown or pinkish mucus discharge (also referred to as bloody show)
- Period-like abdominal cramps
- Throbbing or dull pain in the lower back
- Diarrhea
- Amniotic saciThe thin-walled fluid-filled sac in the uterus where the embryo grows and eventually forms the fetus. rupture – you might experience frequent contractions if the labor is imminent. Water leak
If the leaking water is colorless, odorless and is gushing or leaking slowly, then it indicates the rupture of the amniotic sac.
It means your labor will start soon. But even if labor does not start, just let your doctor know.
What Happens After The Water Breaks?
Most women have a water break before the onset of labor. However, some may have it after the contractions begin.
The rupture of the amniotic sac exposes your baby to various infections (14). The bacteria can travel from the vagina to the uterus, causing infection to both the mother and the baby. To prevent infections, wear a sanitary pad that will keep you dry and clean. Contact your hospital and see the doctor.
When To Call The Doctor?
You must call a doctor if you (15):
- Notice a decreased fetal movement (fewer kick counts)
- Have pain while passing urine as this can indicate urinary infection
- Experience continuous abdominal pain
- Have bright red vaginal bleeding
- Have fever and chills
- Have no contractions even after the water breaks
- Leak yellowish or greenish fluid when the amniotic sac ruptures
Note: If the amniotic fluid appears brown or green, then notify your doctor immediately. It happens when your baby passes meconium in the sac and is an indication that your baby is stressed and needs to be delivered as soon as possible (16).
Once you reach the hospital, the doctor may wait for the contractions to begin. If the contraction does not start by itself, then the doctor may induce labor. In some women, the amniotic sac will not rupture until they are into active labor.
Labor At 40 Weeks Pregnancy
As you enter labor, the pain grows intense and stronger till the cervix opens completely. You may also have cramps. Your doctor will check if you need epidural anesthesia when the pain becomes unbearable.
The average labor time is six hours (17).
In some cases, labor begins naturally but in some other cases, the doctor may induce it.
Inducing Labor At 40 Weeks Pregnancy
Labor induction helps start the birthing process through medical intervention.
Labor is induced in the following cases (18):
- You have a water break, and the contractions are delayed. Inducing labor will help prevent infections to you and the baby.
- You have high blood pressure at full-term.
- Prolonging the pregnancy poses risks to you or your baby.
- The amniotic fluid is insufficient.
You have long crossed your due date. However, at 40 weeks, you would be advised to wait for a few more days.
 Point to consider
Point to considerHow is labor induced?
Labor can be induced through traditional methods such as:
- Sexual intercourse
- Nipple stimulation
- Walking
- Acupuncture
However, there is little scientific evidence to prove their effectiveness (19).
Medical techniques for inducing labor include include (20):
- Membrane stripping or sweeping
- Oral or vaginal medication
- OxytociniA hormone secreted by the pituitary gland to stimulate contractions during childbirth and lactation. administered through IV
- Rupturing the amniotic sac
Discuss with your doctor about the benefits and risks before you agree to induced labor.
Your delivery will be smooth if your baby is in the right position that is head-down. But if the baby is in a breech position, a normal delivery could become a problem.
 Point to consider
Point to considerWhat If The Baby Is In A Breech Position?
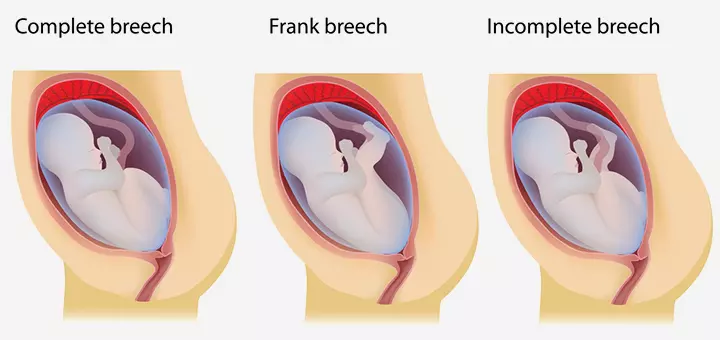
By the time you enter labor, the baby moves down into the pelvis with its head down for easy passage through the vagina. But if the baby has its buttocks or legs down, it is called a breech presentation.
Such a situation arises in some cases of twin pregnancies, in the absence of sufficient amniotic fluid, the presence of uterine fibroidsiAbnormal benign growths in or on the uterine wall. , and also due to physical abnormalities in the baby (22).
In the case of breech presentation, your OB/GYN will do a pelvic examination or an ultrasound scan to confirm the breech. Once it is confirmed, they might suggest a cesarean section or external cephalic version (ECV), where the doctor would change the baby’s position manually.
The ECV method helps in getting the baby to head-down position (23). However, in the 40th week, this method is not encouraged by the doctors as there is no room for the baby to move inside.
The breech position will definitely increase your anxiety levels, and anxiety is exactly what you should not have during labor.
Tips To Help You Cope With Labor
Whether it is a breech position or a head-down, you need to know how to face the situation without getting tensed. Here are some tips you can follow:
- Stay calm: Find ways to keep yourself occupied, while the help is on the way. Engage in packing clothes and other things needed for your stay in the hospital. Stay calm as you wait for the onset of labor. You may practice breathing exercises that will help you during delivery.
- Do light exercises: Engage in light exercise to keep yourself active. This will also help in inducing labor. But you can do this only in the presence of a professional and with the permission from your doctor.
- Get good sleep: Try to take a nap before your labor begins. It helps you stay active and push the baby with all your energy.
- Spend time with your partner: Talk to your partner. Ask him to massage your back or just keep talking so that you are distracted from the pain and anxiety. His presence will boost your confidence.
Not just presence, the dad-to-be should also participate in the event with all the contribution he can make.
Tips For Dads-To-Be
Dads, let’s tell you that you will have your moments of fear and anxiety. So, here are some tips you can follow to ease your emotions:
Know your stuff: Understand what your partner is going through. Make a note of the instructions given by your doctor. Prepare yourself for the D-day so that you can act wisely rather than be terrified when your partner’s water breaks.
- Understand what she wants: Once your partner goes into labor, try to understand her preferred method of delivery – whether she wants to get induced, opt for a C-section, or opt for natural birth.
- Do your homework on hospitals: Enquire about the various hospitals in your locality. Weigh the facilities they are offering, their hospital policies, and their track record. This will make it easy for you to contact your preferred hospital when the time comes.
- Know when to take charge: While in labor, your partner might not be able to make the right decision. If she is unable to understand what is happening, and what she needs to do, hold her hand and explain the situation patiently.
As you help your partner to deliver, you both will realize that it is not too long before you become parents to a lovely little baby.
What Happens Immediately After The Baby Is Born?
This information will prepare you for a series of events that will happen after the birth of your baby.
In babies:
- Soon after the baby is out, he/she may cry out loudly or stay unconscious due to the medicinal effect.
- The umbilical cord is cut and clamped.
- The doctor uses an aspirator to suction the baby’s mouth and throat to remove any traces of fluid. The newborn will be wiped dry and covered in a blanket to provide warmth. The blood sample taken from the umbilical cord will be tested for identifying your baby’s blood group and several other factors.
- The infant will be administered the necessary vaccinations. Your baby will be given an Apgar score based on their physical and health conditions. The doctor will check for the heartbeat, muscle tone, response to stimuli, breathing rate and color of skin for the score.
In mothers:
- The doctor will first try to stop excess bleeding.
- She will check the placenta to ensure that no fragments are left inside the uterus because it can cause bleeding or infections.
- The internal and external stitches, if any, are left to heal on their own.
Ensure you have a strong support system for your postpartum needs and childcare. This can aid in your physical recovery and support your emotional well-being.
Frequently Asked Questions
1. What if I get unpleasant discharges at 40 weeks?
As the cervix opens, a thick mucus plug with a tint of blood is discharged. It indicates that your labor is closer. However, if the discharge has a foul smell, then it might indicate a vaginal infection that can affect your baby inside. Inform the doctor in such a case.
2. What is a post-term pregnancy?
If a pregnancy lasts beyond 42 weeks, it is termed as post-term pregnancy. It increases the complications of stillbirth, large babies, and fetal mortality. In such cases, a C-section is usually recommended over vaginal delivery to avoid any risks of infections and postpartum hemorrhage (24).
3. Is the 40th week of pregnancy good for delivery?
At 40 weeks, a pregnancy is considered full-term, and the baby is fully developed and ready for birth. Therefore, delivering in the 40th week is usually safe. However, medical intervention may be necessary if there are concerns regarding the health of the mother or the baby. Speak to your healthcare provider to know if delivering at the 40th week is safe and healthy for you and your baby (25).
4. How common is labor at 40 weeks?
Research suggests that approximately 60 out of 100 expectant mothers give birth on or before their calculated due date (25). The length of a pregnancy is always considered 40 weeks, and the due date is calculated based on the last date of period (LOP).
5. How long does a fetus sleep in the womb at 40 weeks?
According to a study, fetuses spend 90-95% of their time in deep sleep between 38 and 40 weeks of pregnancy (26).
6. Why is my cervix closed at 40 weeks?
It is not uncommon for the cervix to remain closed as you near your due date, but typically, cervical changes begin several weeks before birth. Your healthcare provider will monitor cervical changes during your third trimester prenatal appointments and update you (27).
7. Why is my stomach so hard at 40 weeks?
At 40 weeks, the baby may drop down into the pelvis, and their head presses on the cervix, making your belly feel firm or hard. Braxton Hicks contractions are the other possible cause for belly hardening during this time. These contractions occur throughout the pregnancy but may become more frequent and strong as you near your due date.
8. How many movements should I feel at 40 weeks?
According to experts, pregnant women should feel at least ten fetal movements within two hours starting from 28 weeks of pregnancy (28). At 40 weeks, your baby should be moving frequently, though the number of movements may vary.
9. How should I sleep at 40 weeks pregnant?
Expecting women are advised to sleep on their side, particularly the left side. This position promotes better blood flow to the baby and improves kidney function. Additionally, spending most of your time in bed, particularly on your back or sitting up, can impede the progress of labor (29).
Now that you have reached the last week of pregnancy, your joy and anxiety might be at their peak. However, note that it is common for pregnant women not to experience any labor pains during the 40th pregnancy week. While a few have early deliveries, others may experience it later. Therefore, while the labor may not be within your control, being vigilant about its symptoms and staying calm is the best you can do. If you notice any discomfort or are worried about delayed childbirth, it is also advisable to consult your physician for any queries.
Infographic: Signs Of Labor At 40th Week Of Pregnancy
Being 40 weeks pregnant means you’ve already reached your full term and can go into labor at any time. Therefore, knowing the signs of labor can help determine when to go to the hospital. Check out the infographic below to learn about the signs of labor in the 40th week of pregnancy and what to do next.

Illustration: Momjunction Design Team
Illustration: 40th Week Pregnancy: Symptoms Baby Development And Tips

Image: Dall·E/MomJunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Baby #3: 40 weeks + 2 days | final pregnancy post!https://julia-transition.blogspot.com/2014/07/baby-3-40-weeks-2-days-final-pregnancy.html
References
- When Does Labor Usually Start?
https://www.nichd.nih.gov/health/topics/labor-delivery/topicinfo/start-of-labor - Third Trimester.
https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-third-trimester - Pregnancy.
https://www.nhs.uk/start-for-life/pregnancy/week-by-week-guide-to-pregnancy/3rd-trimester/week-40/ - Your Pregnancy Guide.
https://www.fhs.gov.hk/english/health_info/woman/30005.pdf - 40 Reasons To Go The Full 40 Weeks Of Pregnancy.
https://www.health4mom.org/go-the-full-40/ - Pregnancy Planning.
https://www.womenandinfants.org/services/pregnancy/pregnancy-planner - Pregnancy – Labour.
https://www.betterhealth.vic.gov.au/health/healthyliving/pregnancy-labour - Pregnancy At Week 40.
https://www.pregnancybirthbaby.org.au/pregnancy-at-week-40 - Fetal development.
https://medlineplus.gov/ency/article/002398.htm - A woman’s right to know.
https://firstcareclinic.org/wp-content/uploads/2018/08/p40074.pdf - Meconium
https://my.clevelandclinic.org/health/body/24102-meconium - Amniotic Fluid Index.
https://radiopaedia.org/articles/amniotic-fluid-index - Monitoring Your Baby Before Labor.
https://medlineplus.gov/ency/patientinstructions/000485.htm - Amniotic Fluid.
https://www.sutterhealth.org/health/labor-delivery/amniotic-fluid - CPMC Pregnancy and Childbirth Services.
https://www.sutterhealth.org/cpmc/services/pregnancy-childbirth - Meconium Aspiration Syndrome (MAS).
https://kidshealth.org/en/parents/meconium.html - ‘active Labor’ Duration And Dilation Rates Among Low-Risk Nulliparous Women With Spontaneous Labor Onset: A Systematic Review.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2904982/ - Quick Facts About Labor Induction.
https://nationalpartnership.org/our-work/resources/health-care/maternity/quick-facts-about-labor-induction.pdf - Marit L. B. et al. (2014); What Started Your Labor? Responses From Mothers in the Third Pregnancy Infection and Nutrition Study.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4210668/ - Induced Labor – What Are The Options?
https://www.pregnancybirthbaby.org.au/induced-labour - Labor Induction.
https://www.acog.org/womens-health/faqs/labor-induction - Breech Baby.
https://my.clevelandclinic.org/health/diseases/21848-breech-baby - External Cephalic Version.
https://www.pregnancybirthbaby.org.au/external-cephalic-version-ecv - Post-term Pregnancy.
https://www.stanfordchildrens.org/en/topic/default?id=post-term-pregnancy-90-P02487 - Pregnancy and birth: When your baby’s due date has passed.
https://www.ncbi.nlm.nih.gov/books/NBK279571/ - Neurophysiologic Measurement of Continuity in the Sleep of Fetuses during the Last Week of Pregnancy and in Newborns.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2140151/ - Mid-Pregnancy Ultrasonographic Cervical Length Measurement (A Predictor of Mode and Timing of Delivery): An Observational Study.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6329997/ - Quickening in Pregnancy.
https://my.clevelandclinic.org/health/symptoms/22829-quickening-in-pregnancy - Sleep During Pregnancy.
https://www.pregnancybirthbaby.org.au/sleep-during-pregnancy
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Burcu Saygan Karamürsel
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Aneesha Amonz





















