Altitude sickness in babies can present itself as the baby seeming visibly uncomfortable and beginning to throw up when traveling to the mountains or higher altitudes (1). It might be stressful for the parents to see their baby in distress or discomfort. Read this post to know more about the causes, types, signs, diagnosis, treatment, and prevention of altitude sickness in babies.
Key Pointers
- Altitude sickness is discomfort experienced by babies at high altitudes.
- Babies should be at least six weeks old to travel to higher altitudes.
- Symptoms of altitude sickness in babies include crying, lethargy, and irritability.
- To keep your baby hydrated at higher altitudes, feed them milk and formula at regular intervals. Frequent meals rich in carbohydrates can help alleviate altitude sickness.
- However, consult a doctor if symptoms persist or become severe.
What Causes Altitude Sickness In Babies?
Altitude sickness is an umbrella term for a group of symptoms that might occur when you travel to a place at a high altitude. It is also known as ‘mountain sickness.’
The air in the atmosphere exerts pressure on Earth. It is known as barometric pressure. As we go higher in altitude, this pressure begins to drop. Along with the pressure, the oxygen level in the surrounding atmosphere also falls.
Multiple changes in the atmosphere affect the body, thus causing altitude sickness and making the baby feel uncomfortable.
Pediatrician Dr. Kishor Tewary says, “Infants under six weeks of age, and those having congenital cardiopulmonary disorders, pulmonary hypertension, systemic diseases that compromise respiratory function, and a history of respiratory distress are at a higher risk of having altitude sickness.”
Is It Safe For A Baby To Visit High-altitude Areas?

Dr. Maria Carmela Villania-Mamauag, board-certified diplomate of the Philippine Pediatric Society, advises, “For babies less than six weeks old, traveling to a higher altitude would not be a good move. The baby’s immature immune system, along with the sudden altitude change, could have harmful effects.”
It could be safe to travel to high-altitude places once the baby is more than six weeks old (1). You may follow some precautions during the trip.
- Seek your pediatrician’s consent before traveling to places of high altitude. The doctor’s approval is vital if your baby was premature, unwell recently or has a medical condition. They may prescribe any emergency medications for altitude sickness.
- If your baby has a frequent need for supplemental oxygen, that is, requires oxygen inhalation through a machine or cylinder, then it is advised against visiting a place at high altitude.
- Babies with pulmonary hypertension, a form of high pressure in the lungs causing low oxygen levels in the blood, should be avoided from being taken to such places.
Keep your baby hydrated with breast milk and water, once you have observed all the precautions and reached a high altitude region. Feed your baby small but multiple meals a day if they are on solids. Babies younger than six months should be given only breast milk.
How To Take Care Of A Baby Having Altitude Sickness?

You can observe the following simple non-pharmacological methods to help the baby with altitude sickness feel better.
- Hydrate your baby through breast milk or formula. If your baby is older than six months, then you can provide them with frequent sips of water.
- Feed your baby small yet frequent meals that are high in carbohydrates. It is noted that craving for carbohydrates tends to increase at high altitudes (2). Carbohydrates may help provide sufficient energy to the body to overcome altitude sickness
- Regions at a high altitude are often cold. Dress your baby in insulated clothing. Staying warm may help the baby feel better.
- Monitor your baby’s oxygen levels, particularly if symptoms continue. A pulse oximeter can help ensure adequate oxygen saturation.
A baby can be prone to altitude sickness even when they are healthy. It is thus essential to know the variations of altitude sickness.
Types Of Altitude Sickness
Altitude sickness occurs in various levels of severity. It is broadly classified into three different syndromes.
1. Acute mountain sickness (AMS)
This is the most common form of altitude sickness but is less severe (3). Healthy babies may also have AMS.
2. High altitude pulmonary edema (HAPE)
HAPE occurs when fluid accumulates in the tissues and air spaces within the lungs (4). This leads to the impaired exchange of gasses and may cause respiratory failure. HAPE has the symptoms of AMS (listed later) accompanied by breathlessness, coughing, and weakness. Oxygen support or descent might be life-saving.
HAPE is significantly less common than AMS. The combined statistics derived from several studies indicated that the incidence of HAPE in children under two is 0.9 percent (17). Babies with the following conditions tend to be more susceptible to HAPE (1) (5).
- Recent viral infections
- Recent upper respiratory tract infections
- Pulmonary hypertension (high blood pressure)
- Problems with pulmonary artery and pulmonary vein
- Atrial and ventricular defects (heart defects)
- Obstructive sleep apneaiA sleep disorder in which there are recurrent episodes of breathing pauses.
- Babies with Down’s syndromeiA chromosomal disorder caused by the presence of an extra copy of chromosome 21, resulting in intellectual impairment and short stature. might be more prone to HAPE.
3. High altitude cerebral edema (HACE)
High altitude cerebral edema is considered the most severe form of altitude sickness but is also the rarest (6). The condition occurs when there is an influx of fluid and swelling of the brain due to low oxygen in ambient air (7). Along with all the symptoms of AMS, HACE has profound lethargy, drowsiness, dizziness, confusion, and poor muscle control.
HAPE and HACE can be fatal, and usually, a prompt descent to a low altitude is suggested. Since AMS can aggravate HAPE or HACE, it is essential to know the symptoms of altitude sickness in babies.
 Did you know?
Did you know?What Are The Signs Of Altitude Sickness In Babies?

Unlike adults, infants may not show typical altitude sickness symptoms, so parents should monitor them closely. Board-certified pediatrician Dr. Edward Kulich observes, “Infants with altitude illness or acute mountain sickness can display symptoms such as headache, irritability, fussiness, poor feeding. This is commonly seen when there is a rapid ascent to a significant altitude.” If you just traveled with your baby to a high-altitude location, be alert to the following general indicators of altitude sickness (15).
- Fussiness
- Food refusal
- Crying
- Irritability
- ClinginessiA tendency to seek attention, physical contact, and proximity to parents for protection
- LethargiciHaving very little energy to do anything
Some symptoms, such as severe crying and irritability, may also happen due to tiredness from the trip. So let your baby rest well. If the symptoms persist even after resting, then it could be acute mountain sickness.
There are a few severe symptoms of altitude sickness that could point towards HAPE and HACE.
- Breathlessness
- Cyanosis, a bluish discoloration of the skin
- Confusion
- AtaxiaiA term that refers to a lack of muscle control, coordination, and body balance. , poor muscle control and inability to move
- Coughing
- Repeated vomiting
When Should You Call The Doctor?
See a doctor during the following situations:
- The baby shows severe symptoms of altitude sickness
- General symptoms of AMS persist for more than three days.
- There is labored breathing with constant shortness of breath.
- Repeated vomiting and dehydration
- Refusal to eat or drink
These problems require prompt medical attention.
The symptoms of altitude sickness could overlap with other conditions. Also, a baby cannot verbally express discomfort. Therefore, a score-based diagnostic tool could be used to determine if the baby has altitude sickness.
How To Diagnose The Severity Of AMS In Your Baby?
The severity of altitude sickness may be determined through the use of Children’s Lake Louise Score (CLLS) for the diagnosis of acute mountain sickness (AMS) in preverbal children (8).
The process begins by rating the amount and intensity of baby’s fussiness measured on the following scales.
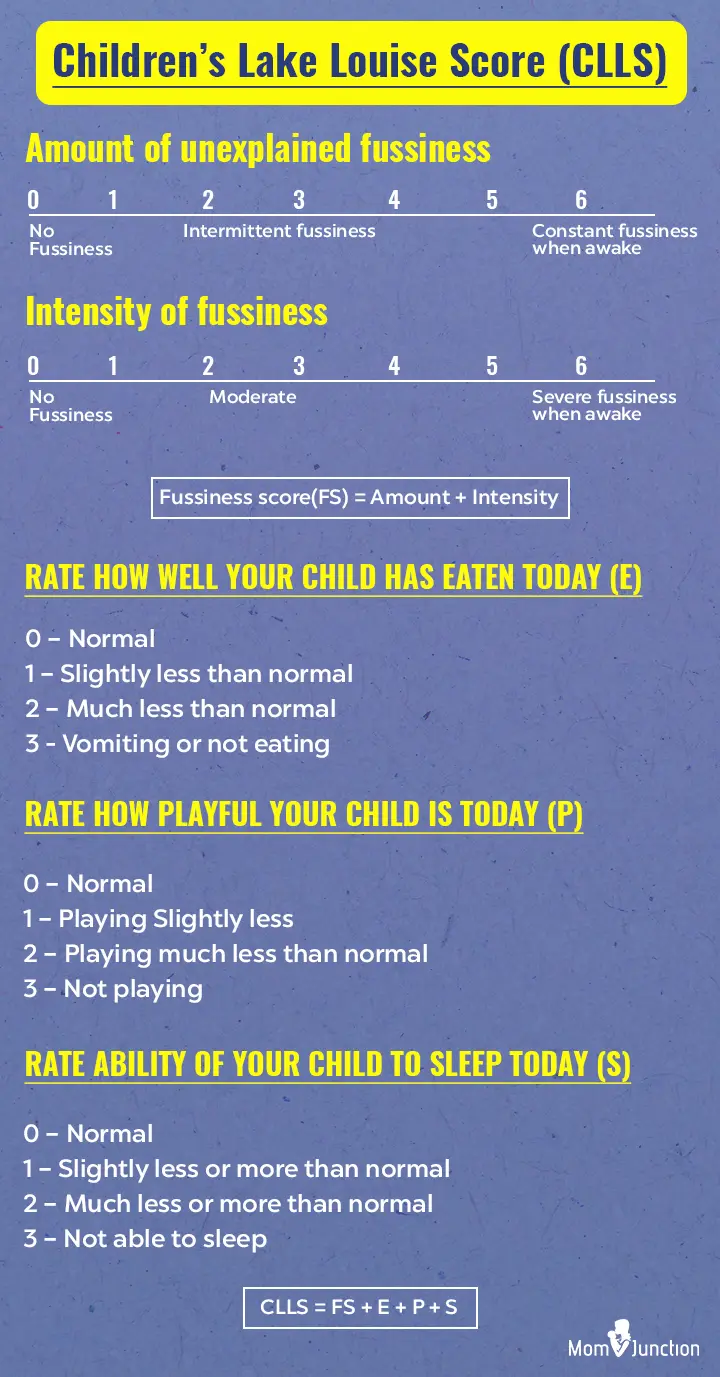
Meeting all of the following score conditions determines the presence of acute mountain sickness:
- Fussiness score (FS) should be greater than or equal to 4
- Eating, playfulness, and sleep score (E+P+S) should be greater than or equal to 3
- The total Children’s Lake Louise Score (CLLS) should be greater than or equal to 7
CLLS is useful in providing an approximate idea to the parents about the severity of altitude sickness in their baby. It is best to consult a doctor if you have any concerns or when the baby displays severe symptoms of altitude sickness.
How Is Altitude Sickness In Babies Treated?

The doctor may suggest the following treatment methods to help the baby feel better.
- Medications: If the baby is feeling excessively fussy and restless, then the doctor may prescribe ibuprofen or acetaminophen. Do not self-medicate even with over-the-counter medicines.
- Electrolyte supplement: If the baby is dehydrated due to vomiting and is feeling dizzy, then the doctor may suggest an electrolyte solution such as an oral rehydration salt (ORS) (18). It may help subdue nausea and constant discomfort caused by altitude sickness.
- Descent to low altitude: If the condition of the baby does not seem to improve, then the last resort will be moving to a place with a low altitude.
Do not give acetazolamide, nifedipine, and dexamethasone to the baby
. These medicines are conventionally administered to teens and adults for altitude sickness. But their effect on infants is not well known, and it may cause side effects. Consult your doctor before giving any medicine to the baby.
How To Prevent Altitude Sickness In Babies?

A few simple steps can help you avoid altitude sickness in babies (9).
- Avoid flying directly to an altitude above 2,750 meters (9,000 feet). The baby’s body will have no time for acclimatization.
- Ascend 1,000 feet (305 meters) at a time. Spend a day at that altitude before moving any further. It will help your baby’s body to get used to the increasing altitude gradually.
- Let your baby rest. Make sure they are not fussy, cranky, and tired before your trip to the high-altitude location.
- Hydrate the baby as you reach a high-altitude location.
 Quick fact
Quick factDoes High Altitude Make A Baby Have Ear Infections?
There is no direct link between living at high altitudes and ear infections in babies. Changes in altitude may increase the risk of infection (10). However, the risk might be due to related changes in climate since places at a higher elevation tend to be colder. If your baby has enough time to acclimatize to the altitude and weather, then they may be less prone to ear infections. In addition, exposure to a hypobaric environmentiAn environment with low atmospheric pressure like that at a high altitude can lead to oxygen deprivation and potentially increase the risks for conditions such as respiratory distressiA condition marked by difficulty in breathing and increased oxygen demand , headaches, and fatigue (7).
Frequently Asked Questions
1. Does aspirin help with altitude sickness?
Adults use aspirin to manage altitude sickness. But, it is not advisable to use aspirin for altitude sickness in babies as some studies have found aspirin linked to developing Reye’s syndromeiA serious but rare condition that leads to swelling in the liver and brain and may be fatal if left untreated. (11).
2. Does Benadryl help with altitude sickness in babies?
Some adults use Benadryl to sleep better at higher altitudes (12). However, avoid using Benadryl for babies because it is not safe for children under two (13).
3. How does altitude sickness in babies differ from that in adults?
Lethargy, food refusal, increased irritability, and more than usual crying are the major signs of altitude sickness in babies. In adults, headache, nausea, exhaustion, anorexiaiA psychological condition characterized by unhealthy weight loss and distorted body image or loss of appetite, dizziness, and sleep disturbances are the major signs. These symptoms can be due to changes in the diet because of remote travel. Children are no more likely to experience acute mountain sickness than older people (15).
4. Is any research being conducted on treating altitude sickness in babies?
Research on treating altitude sickness in babies is limited, primarily due to the rarity of this condition in infants. However, research is ongoing to better understand the prevalence, risk factors, and clinical manifestations of altitude sickness in infants and children. Researchers and scientists are also investigating pharmacological interventions to treat the condition in children.
5. Is there a genetic component associated with altitude sickness in babies?
Researchers have identified various genes that may underlie the adaptation or maladaptation of people to high altitudes. Differences in adaptation patterns between the high-altitude groups show that some unique genetic mechanisms affect the adaptations. Some researchers also say that harsh environmental stress at high altitudes may modify DNA methylationiA chemical process where methyl groups are added to DNA to regulate gene expression or histone modificationiChemical changes to histone proteins that regulate gene expression and chromatin structure . It is observed that even a short period of hypoxia triggers changes in DNA (16).
6. How can I prepare my baby for high-altitude travel?
Before planning high-altitude travel, consult your doctor, especially if your baby has any health conditions that might worsen by altitude. Plan for a gradual ascent to help your baby adjust more comfortably. Be alert to any symptoms that may require medical attention, and carry baby essentials, such as a water bottle and blanket, to keep your baby hydrated and rested.
If your baby is fussy, refuses food, cries, or seems uncomfortable at higher altitudes, they may be experiencing altitude sickness. Altitude sickness in babies occurs because of the low pressure and oxygen level at higher altitudes. To stay safe from this condition, discuss the precautions with your doctor before visiting a mountainous region. Follow simple tips for traveling with a baby, such as keeping your baby hydrated, offering frequent carbohydrate-rich meals, and dressing them warmly to keep them comfortable and safe. Although severe symptoms such as breathlessness, repeated vomiting, or cyanosis are rare, keep an eye on your baby. If you notice anything worrying, contact your doctor promptly. Do not panic if your baby is uncomfortable on a mountain trip. Acclimatization and precautions will help you enjoy a comfortable vacation with your little one.
Infographic: Tips On Managing A Baby Experiencing Altitude Sickness
While adults may be able to manage their altitude sickness symptoms with self-care and different techniques, it may be much more difficult for babies to cope with. So, follow the tips in the infographic below to prevent your little one from throwing up and constantly crying when traveling to high-altitude areas. Illustration: Momjunction Design Team
Illustration: Altitude Sickness In Babies: Everything You Need To Know

Image: Stable Diffusion/MomJunction Design Team
References
1. Michael Yaron and Susan Niermeyer, Travel to High Altitude with Young Children: An Approach for Clinicians; High Altitude Medicine & Biology
2. Askew EW, Food for high-altitude expeditions; National Center for Biotechnology Information
3.Acute morning sickness; U.S. National Library of Medicine
4. Peter H. Hackett and David R. Shlim, High-Altitude Travel & Altitude Illness; Centers for Disease Control and Prevention
5. Durmowicz AG, Pulmonary edema in 6 children with Down syndrome during travel to moderate altitudes; National Center for Biotechnology Information
6. SR Mehta et al., Acute Mountain Sickness, High Altitude Cerebral Oedema, High Altitude Pulmonary Oedema: The Current Concepts; National Center for Biotechnology Information
7. Altitude sickness; NHS UK
8. Michael Yaron et al., Evaluation of Diagnostic Criteria and Incidence of Acute Mountain Sickness in Preverbal Children; Wilderness & Environmental Medicine Journal
9. Altitude Sickness; Harvard Medical School
10. Ear infection – acute; U.S. National Library of Medicine
11. Reye Syndrome in Children; Stanford Children’s Health
12. Altitude Illness; Himalayan Rescue Association Nepal
13. Diphenhydramine Dosing Table; American Academy of Pediatrics
14. Inder S Anand and Tianyi Wu; Syndromes of subacute mountain sickness; High altitude medicine & biology
15. Andrew J Pollard et al.; Children in the mountains; BMJ
16. Roy RonenThe genetic basis of chronic mountain sickness; NCBI
17. Santiago Ucrós et al.; (2023);High altitude pulmonary edema in children: A systematic review;NCBI
18. Dehydration: Giving Liquids at Home; JNationwide Children’s Hospital
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Shashidhar A
- Dr. Kishor Tewary is a senior consultant pediatrician with a special interest in pediatric urology and nephrology. He worked as a consultant pediatrician and nephrologist in India before moving to the UK for advanced training in 1997. Dr. Tewary has been practicing in the UK since 2007 and has served national regulatory and educational bodies in various positions, including as an associate professor at the St George's University of Medicine Grenada, senior lecturer at Birmingham University Medical School, and MIMS assessor at Aston University Medical School.
 Dr. Kishor Tewary is a senior consultant pediatrician with a special interest in pediatric urology and nephrology. He worked as a consultant pediatrician and nephrologist in India before moving to the UK for advanced training in 1997. Dr. Tewary has been practicing in the UK since 2007 and has served national regulatory and educational bodies in various positions, including as an associate professor at the St George's University of Medicine Grenada, senior lecturer at Birmingham University Medical School, and MIMS assessor at Aston University Medical School.
Dr. Kishor Tewary is a senior consultant pediatrician with a special interest in pediatric urology and nephrology. He worked as a consultant pediatrician and nephrologist in India before moving to the UK for advanced training in 1997. Dr. Tewary has been practicing in the UK since 2007 and has served national regulatory and educational bodies in various positions, including as an associate professor at the St George's University of Medicine Grenada, senior lecturer at Birmingham University Medical School, and MIMS assessor at Aston University Medical School. - Dr. Edward Kulich is a board-certified pediatrician, a fellow of the American Academy of Pediatrics, and the American Academy of Home Care Physicians. He obtained his Doctor of Medicine from St. George's University School of Medicine, completed a residency in Pediatrics at Maimonides Medical Center, Infants and Children’s Hospital of Brooklyn, and maintains privileges at Cornell, Lenox Hill, Mt. Sinai, and NYU hospitals. He has over 15 years of experience and is the current president of the American Academy of Concierge Pediatricians. Dr. Kulich is the author of The Best Baby Sleep Book and The Best OLSAT Book.
 Dr. Edward Kulich is a board-certified pediatrician, a fellow of the American Academy of Pediatrics, and the American Academy of Home Care Physicians. He obtained his Doctor of Medicine from St. George's University School of Medicine, completed a residency in Pediatrics at Maimonides Medical Center, Infants and Children’s Hospital of Brooklyn, and maintains privileges at Cornell, Lenox Hill, Mt. Sinai, and NYU hospitals. He has over 15 years of experience and is the current president of the American Academy of Concierge Pediatricians. Dr. Kulich is the author of The Best Baby Sleep Book and The Best OLSAT Book.
Dr. Edward Kulich is a board-certified pediatrician, a fellow of the American Academy of Pediatrics, and the American Academy of Home Care Physicians. He obtained his Doctor of Medicine from St. George's University School of Medicine, completed a residency in Pediatrics at Maimonides Medical Center, Infants and Children’s Hospital of Brooklyn, and maintains privileges at Cornell, Lenox Hill, Mt. Sinai, and NYU hospitals. He has over 15 years of experience and is the current president of the American Academy of Concierge Pediatricians. Dr. Kulich is the author of The Best Baby Sleep Book and The Best OLSAT Book.
Read full bio of Dr. Ritika Shah
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny