Image: Shutterstock
Amoxicillin, also spelled as Amoxycillin, is an antibiotic made from penicillin. It is either used alone or in combination with clavulanic acid and is taken in various forms, including tablets, powder, and syrup. The World Health Organization has categorized it as an important medicine.
Amoxicillin is mainly prescribed for treating infections, such as strep throat, pharyngitisiAn inflammation in the pharynx (back of the throat) characterized by pain and swallowing problem , and tonsillitisiAn inflammation of the tonsils, oval-shaped tissue pads on either side of the back of the throat , caused by the streptococcus bacteria and other bacterial infections such as pneumonia and UTI. However, it can also be used to relieve symptoms of various maternal health conditions, ranging from skin infections to urinary tract infections.
In breastfeeding mothers, amoxicillin is also prescribed for mastitisiInflammation of the breast tissue, which can be pain-inducing (1). But since the medicine passes through the bloodstream into the milk, the baby might also feed on it. Therefore, it is important to understand how amoxicillin affects the baby if the mother consumes the medicine.
This leaves us with one question: can you take amoxicillin while breastfeeding? Read this post to understand the safety of amoxicillin during breastfeeding, its side effects, and things you can do to reduce the risk of the medicine.
Key Pointers
- Amoxicillin is a penicillin-based antibiotic commonly used for treating infections such as tonsillitis and strep throat.
- It is generally considered safe for lactating women to use, but it does pass into breast milk and remains there for 4-6 hours.
- Breastfed babies may experience adverse effects such as drowsiness, hives, stomach ache, and colic from the medication.
- To prevent side effects, it may be helpful to feed the baby before taking the medication with a proper dose or consider using formula milk instead.
Is Amoxicillin Safe While Breastfeeding?
Amoxicillin is considered safe for breastfeeding mothers by the American Academy of Pediatrics, and research shows no change in the health of the nursing infant when the mother is on a dosage
(2). The medicine is among the safest antibiotics when breastfeeding (3). However, it is not entirely free of potential side effects, just like other medications.
Does Amoxicillin Pass Through Breast Milk?

Image: IStock
While the drug may not hinder milk production, amoxicillin passes into the breast milk just like any other chemical compound present in the mother’s bloodstream. The peak level of amoxicillin in breast milk is found between four and six hours after a single dose of 1g consumed by the mother. The amount of drug present in breast milk can vary depending on the woman’s body. The average levels of amoxicillin usually found in breast milk are 0.5 mg/ml at four hours, 0.81mg/ml at five hours, and 1.64 mg/ml at six hours (4).
 Quick fact
Quick factSide Effects Of Amoxicillin In Breastfed Babies
, a board-certified allergist and immunologist from St. Louis, Missouri, says, “Since some amoxicillin gets into the blood supply, it can cause minor symptoms in breastfed babies. These include mild rash, diarrhea, or drowsiness.
“A true allergic reaction can consist of hives, swelling, cough, wheeze, nausea, vomiting, diarrhea, and throat swelling. It usually occurs within an hour of taking the dose and requires urgent treatment. Delayed rashes can also happen. These usually come on several days to a week after starting the medication and can take up to one to two weeks to resolve after stopping the medication.”
Though the side effects of amoxicillin are not widespread and have a low probability of occurrence, it is useful to know how a baby could be affected by the drug:
- Diarrhea
- Bloody stools
- Skin hives
- Constant sleepiness or drowsiness
- Excessive coliciFrequent, prolonged, and intense periods of crying in a healthy baby without any apparent reason due to stomach pain with general irritability
Diarrhea, vomiting, nausea, and other side effects are similar to what a mother or any other individual could have on consuming amoxicillin (5). Infants can show other subtle side effects such as a change in feeding and sleeping schedule. When taking amoxicillin, it’s important to monitor your baby for any unusual symptoms.

Image: IStock
If you observe these side effects in the baby or sense something is wrong, then take him to the doctor. Also, find out from your doctor if you should stop taking amoxicillin. However, it is important to ascertain that these symptoms have appeared only after the mother’s use of amoxicillin.
 Be watchful
Be watchfulWhy Does Amoxicillin Cause Side Effects In Breastfeeding Babies?
The side effects are caused due to the active compound penicillin, which is derived from the Penicillium fungus, a living organic matter. The baby’s immune system may mistake penicillin to be a pathogen and mount an attack, which is manifested through symptoms like diarrhea and rashes. The immune system develops an antibody for penicillin to attack it effectively the next time, thus resulting in an allergy. (6).
Amoxicillin is often combined with a compound called clavulanic acid when made into an oral liquid or a solid tablet. One study has found higher instances of side effects in babies whose mothers consumed a mixture of amoxicillin and clavulanic acid than in those whose mothers were given amoxicillin alone (5). However, there is no conclusive research on the effects of clavulanic acid, and it cannot be said for sure that it is the real reason behind the side effects (6).
 Quick fact
Quick factIs Amoxicillin Still Safe For A Breastfeeding Baby?

Image: IStock
Yes, amoxicillin is safe, even in combination with clavulanic acid, since its side effects on breastfeeding babies are infrequent and not long-lasting. Research has found that the notable side effects in breastfeeding infants are drowsiness and diarrhea, which resolve without medical intervention and do not harm the infant (7). A study, which found isolated incidents of side effects, has concluded that amoxicillin is safe for lactating mothers (8).
Therefore, we conclude that amoxicillin is safe for breastfeeding babies. Amoxicillin is considered a safe option for infants with upper respiratory tract infections, with or without Clavulanic acid. No matter how safe a medicine is, you should never take it without a doctor’s prescription.
And when you are taking the drug, you can take some measures to mitigate the risk of side effects on the breastfeeding infant.
How To Mitigate The Risk Of Amoxicillin Side Effects In Babies?
Make sure that the chances of side effects are zero. Follow these measures:
- Tell your doctor that you are breastfeeding: It should be the first thing you tell the doctor when he writes any medicines. The doctor may ask about the age of the baby, frequency of breastfeeding, and if the baby has any history of antibiotic or food allergies. He can then prescribe you a formulation and dosage of amoxicillin, which is least likely to cause side effects in the baby.

Image: Shutterstock
- Do not overdose: Stick to the dose recommended by the doctor and do not overdose, especially the liquid form of amoxicillin (generally prescribed for infants) as you may accidentally pour out extra. Always use the measuring cap provided with the bottle of the medicine to measure the dosage and never use teaspoon/tablespoon for measurement.
- Feed the baby before the dose: Amoxicillin is safe, but you can be extra cautious by breastfeeding the baby before you take the dose. This arrangement is suitable when you have a single dose of amoxicillin a day. Discuss the management of dosage intervals and feeding schedule with your doctor to minimize the risk of side effects on the baby.
- Switch to formula milk: If allergies in your baby make you nervous, then go for formula milk during your treatment. But note that formula milk can also cause severe allergies in some infants. If the baby is older than 12 months, then cow milk can be a good substitute in combination with other nutritious solid food.

Image: Shutterstock
Frequently Asked Questions
1. Should I stop breastfeeding while taking amoxicillin?
You need not stop breastfeeding unless directed by a doctor or unless the baby shows any allergic reactions specific to the drug intake (11).
2. What is the recommended dosage of amoxicillin while breastfeeding?
According to the US Food and Drug Administration, it is safe to consume up to 1000mg of amoxicillin while pregnant or breastfeeding. You may take it at eight-hour intervals (12).
3. Are there any alternative antibiotics I can take while breastfeeding?
Several alternative antibiotics are considered safe for consumption by breastfeeding mothers, such as Azithromycin, Clarithromycin, and Penicillin. However, you should consult a doctor to get an antibiotic prescription rather than self-medicate to avoid complications and allergic reactions (11).
4. Are there any long-term effects of taking amoxicillin while breastfeeding?
Amoxicillin is considered safe for use while breastfeeding, and there are generally no long-term effects for the breastfed infant. Research shows that only small amounts of amoxicillin pass into breast milk, which does not pose a risk to the infant (4). However, you should still talk to your healthcare provider to confirm that amoxicillin is the best treatment option for them.
Amoxicillin while breastfeeding is a medicine commonly prescribed for different types of infections and breast inflammation. Hence, as long as you do not exceed the recommended dosage, amoxicillin is safe during breastfeeding and does not pose any threat to the baby’s health. However, since there is a rare possibility of mild side effects and in order to keep your baby healthy and safe, do not take the drug without consulting your doctor. Remember to check for any adverse reactions in your baby and talk to your healthcare provider for appropriate advice and treatment.
Infographic: More Points To Remember About Amoxicillin
Amoxicillin is a Penicillin group antibiotic that may be used by lactating mothers while following certain precautions. Knowing the drug interactions and contraindications of this medication will help you be cautious when taking it. The infographic below elaborates on the same. Illustration: Momjunction Design Team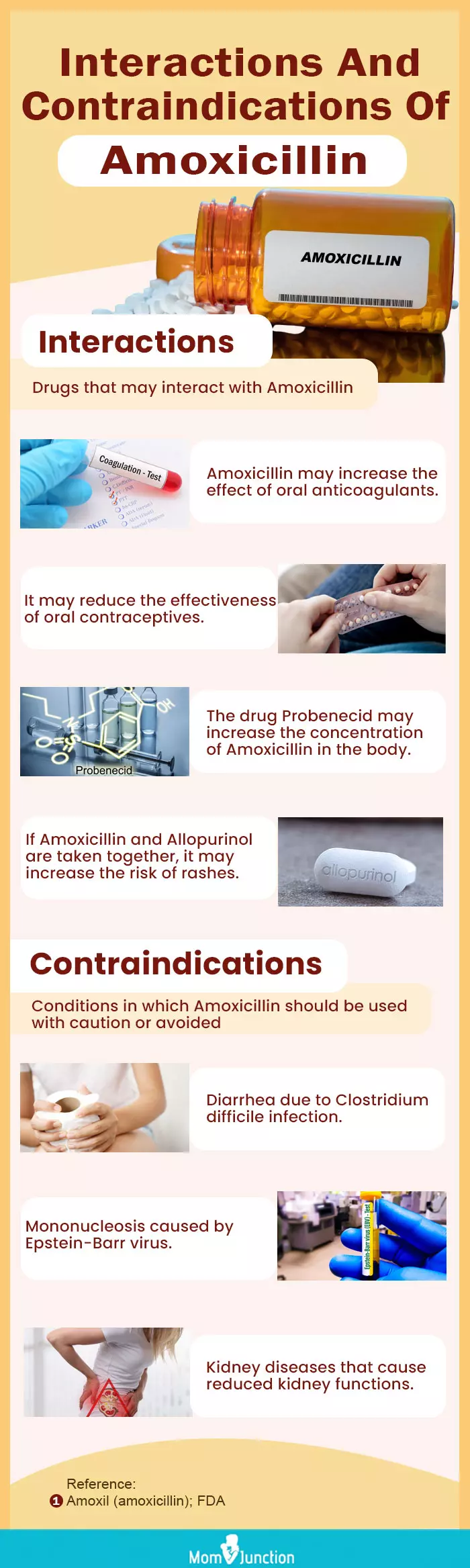
Learn from this video when and how to use amoxicillin. Absorb guidance on timing, duration, and further details to make well-informed health choices.
References
- Management of Mastitis in Breastfeeding Women.
https://www.aafp.org/pubs/afp/issues/2008/0915/p727.html - The Transfer of Drugs and Other Chemicals Into Human Milk.
https://publications.aap.org/pediatrics/article-abstract/108/3/776/66674/The-Transfer-of-Drugs-and-Other-Chemicals-Into?redirectedFrom=fulltext - Effect of maternal antibiotics on breast feeding infants.
https://pmj.bmj.com/content/80/942/196.full - D A Kafetzis et al.; (1981); Passage of cephalosporins and amoxicillin into the breast milk.
https://pubmed.ncbi.nlm.nih.gov/7246123/ - Lilach Benyamini et al.; (2005); The safety of amoxicillin/clavulanic acid and cefuroxime during lactation.
https://pubmed.ncbi.nlm.nih.gov/16044108/ - Drug Safety in Lactation.
https://www.medsafe.govt.nz/Profs/PUarticles/lactation.htm - How best to treat UTIs in women who breastfeed?
https://mospace.umsystem.edu/xmlui/bitstream/handle/10355/41379/UTIsWomenBreastfeed.pdf?sequence=1 - Amoxicillin.
https://www.ncbi.nlm.nih.gov/books/NBK500887/ - Amoxicillin.
https://medlineplus.gov/druginfo/meds/a685001.html - Amoxicillin and Clavulanic Acid.
https://www.ncbi.nlm.nih.gov/books/NBK500776/ - Antibiotics and Breastfeeding.
https://www.breastfeedingnetwork.org.uk/factsheet/antibiotics/ - Amoxicillin Use by Pregnant and Lactating Women Exposed to Anthrax.
https://www.fda.gov/drugs/bioterrorism-and-drug-preparedness/amoxicillin-use-pregnant-and-lactating-women-exposed-anthrax
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Priya Shashank
- Dr. Sonia Cajigal is a board-certified allergist/ immunologist, practicing for seven years. She attended medical school at the University of Missouri-Kansas City School of Medicine and trained around the midwest (Kansas City, Cleveland, Detroit) before settling down back in her hometown of St. Louis, Missouri where she started her own practice.
 Dr. Sonia Cajigal is a board-certified allergist/ immunologist, practicing for seven years. She attended medical school at the University of Missouri-Kansas City School of Medicine and trained around the midwest (Kansas City, Cleveland, Detroit) before settling down back in her hometown of St. Louis, Missouri where she started her own practice.
Dr. Sonia Cajigal is a board-certified allergist/ immunologist, practicing for seven years. She attended medical school at the University of Missouri-Kansas City School of Medicine and trained around the midwest (Kansas City, Cleveland, Detroit) before settling down back in her hometown of St. Louis, Missouri where she started her own practice.
Read full bio of shreeja pillai
Read full bio of Rohit Garoo
Read full bio of Vidya Tadapatri