Image: ShutterStock
Antibiotics are medicines that treat infections caused by bacteria. They act either by killing the bacteria (bactericidal) or making it difficult for the bacteria to grow and multiply (bacteriostatic) (1). Infection during pregnancy may harm both the mother’s and the growing fetus’s health. Therefore, doctors prescribe antibiotics when their benefits outweigh the combined maternal and fetal risks.
This post gives you an insight into the safe use of antibiotics while pregnant, the ones contraindicated, their side effects, and precautions.
Key Pointers
- Your doctor might prescribe antibiotics during pregnancy to treat respiratory tract or urinary tract infections, among others.
- Antibiotics such as Penicillin, Cephalosporins, Carbapenems, and Vancomycin are safe to use during pregnancy.
- However, you must not take antibiotics without your doctor’s consent as they pose the risk of side effects.
- Certain antibiotics such as Tetracyclines and Fluoroquinolones are considered unsafe during pregnancy.
Why Are Antibiotics Prescribed During Pregnancy?
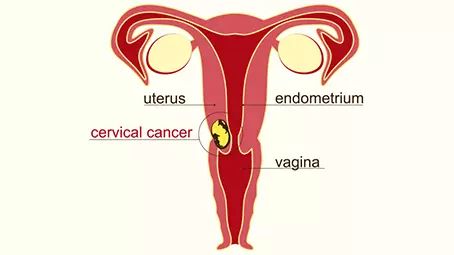
Antibiotics may be prescribed during pregnancy by doctors to treat:
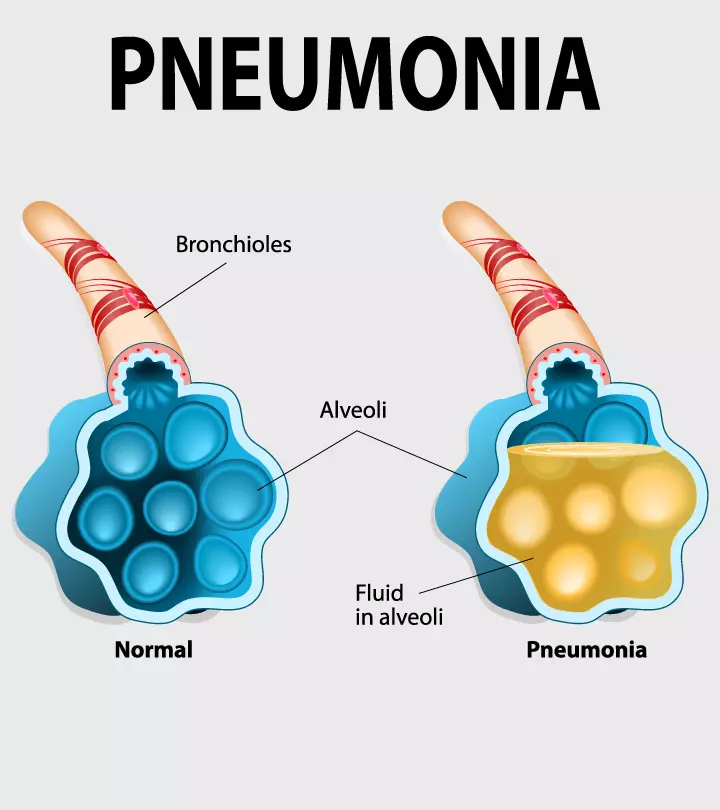
- Severe respiratory or sinus infection
- Urinary tract infection
- Kidney infections
- Bacterial vaginosisi A condition caused by the excess growth of the normal vaginal flora, characterized by increased vaginal discharge with a fishy odor
- Sexually transmitted infections
Antibiotics may also be prescribed for intrapartum fever (fever during childbirth or delivery)
and as preventive medication during cesarean sections (2). Many of these infections could be life-threatening during pregnancy if left untreated. They may also increase the risk of congenital malformationsiA structural or functional abnormality present from birth in the newborn.
Is It Safe to Take Antibiotics When Pregnant?
Studies have shown some antibiotics to be safe during pregnancy, while some may have potential adverse effects on the mother or fetus. The safety may also depend on the dose, duration of antibiotic treatment, and gestational agei A term used to measure the length of the pregnancy from the first day of the last period until childbirth . Additionally, metabolic and immunological changes during pregnancy may change the behavior of drugs inside the body and impact antibiotic therapy (3). Therefore, you should take antibiotics only when prescribed by the doctor.
 Research finds
Research finds
Which Antibiotics Are Safe To Take During Pregnancy?
The United States Food and Drug Administration (FDA) established a pregnancy risk categorization (A, B, C, D, and X) system in 1979. Drugs that may be used during pregnancy belong to category A (No risk in human studies) and category B (Animal reproduction studies have failed to demonstrate a fetal risk and adequate and well-controlled studies in pregnant women are not available).
According to these classifications, the following classes of antibiotics are considered safe during pregnancy (3).
- Penicillins and their newer derivatives are most widely prescribed during pregnancy. A few common ones include Ampicillin, Amoxicillin, and their combinations with Clavulanate and Sulbactam. They are grouped under FDA pregnancy category B.
- Cephalosporins (Ceftriaxone and Ceftaroline) are category B drugs and are considered a first-line option in pregnant women. They may be used in patients allergic or intolerant to penicillin therapy. Cephalosporin combinations (Ceftolozane-Tazobactam, and Ceftazidime-Avibactam) may be used with caution as published data about safety during pregnancy is inadequate.
- Carbapenems (Ertapenem, Meropenem, and Doripenem) are category B drugs. They are generally reserved for pregnant women with penicillin- and cephalosporin-resistant infections with limited alternatives.

- Macrolide antibiotics are category B drugs, and the common ones are Azithromycin and Erythromycin. Erythromycin may be used during pregnancy for preventing Group B streptococcal infection in the newborn. However, some forms, such as erythromycin estolate, should be avoided (4).
- Other antibiotics considered pregnancy-safe (category B) are Vancomycin, Daptomycin, Fidaxomicin, Fosfomycin, and Nitrofurantoin.
 Research finds
Research findsWhich Antibiotics Are Not Safe During Pregnancy?
Some antibiotics have shown an increased risk of birth defects in studies. They were assigned category C (Animal reproduction studies have shown fetal adverse effects and well-controlled human studies are inadequate), category D (there is positive evidence of risk), and category X (contraindicated in pregnancy due to established fetal risks).
Below are the classes of antibiotics associated with safety concerns related to use in pregnancy (3) (5).
- Aminoglycosides: Streptomycin (category D) in the first trimester has been related to congenital deafness in infants and should be avoided. Other aminoglycosides (Gentamicin) have not shown many adverse effects and may be used for the short-term under strict medical surveillance.
- Tetracyclines: These category D antibiotics (Doxycycline, Minocycline, and Tigecycline) have proven teratogenicity (harmful for the fetus). They can bind to calcium in the developing fetus, causing permanent discoloration of bones and teeth. Large doses may also lead to maternal liver toxicity.

- Fluoroquinolones: These consist ofOfloxacin, Ciprofloxacin, and Levofloxacin. Although they are classified as pregnancy category C, they are generally contraindicated in pregnancy. Studies have associated Fluoroquinolones with renal toxicity, cardiac defects, and central nervous system toxicity in the fetus. They may be recommended when there is no alternative.
- Other antibiotics under category B should be used with caution in pregnant women due to the lack of adequate human data confirming their safety. A few examples are below.
- Monobactams: An example is Aztreonam. It may be used only in patients with a severe penicillin allergy or for whom beta-lactam therapy is contraindicated.
- Clindamycin: Vaginal Clindamycin is not recommended as it may increase the risk of neonatal infection and low birth weight.
- Daptomycin: It should be used in pregnancy only if the benefits outweigh the risks.
- Metronidazole: It is contraindicated in the first trimester of pregnancy. Vaginal use may cause congenital hydrocephalus in babies (fluid build-up in the brain). The drug is recommended for use in bacterial vaginosis and Trichomonas infections in pregnancy, but it may cause preterm birth, although this is not clearly established.
Avoid these antibiotics unless prescribed by a healthcare professional, and discuss alternatives with your doctor to ensure the safest options are taken during pregnancy.
What Are The Possible Side Effects Of Antibiotics?

The common side effects of antibiotics include (6):
- Rash
- Dizziness
- Nausea
- Diarrhea
- Yeast infections
A serious allergic reaction may occur due to hypersensitivity, usually to Penicillins and Cephalosporins. The symptoms may include wheezing, hives, shortness of breath, and anaphylaxis (it may feel like your throat is closing or choking, or your voice is changing). Long-term use of antibiotics may also lead to increased susceptibility to infections and disturbances in gut microbiota, which can affect your child and your overall health postpartum (16).
What Precautions To Take When Having Antibiotics In Pregnancy?
Antibiotics account for 80% of all prescribed medication in pregnant women (3). Therefore, it is important to be aware of precautions to minimize fetal and maternal toxicity from antibiotics.
- Inform your doctor that you are pregnant before getting treated for any infection. Discuss with your healthcare provider all medications that you are on, including dietary supplements and herbal products. Also, consider discussing any previous allergic reactions to medications to ensure safety.
- Use antibiotics only when prescribed by an obstetrician or medical doctor. The dosage of antibiotics varies for pregnant women. Therefore, self-medication with the usual dose may cause fetal harm and also increase the risk of antibiotic resistance.
- Consult a doctor whenever you suspect that you have an infection. Antibiotics cannot treat viral infections, such as cold and flu. Get a proper diagnosis before taking any antibiotics.

- Take antibiotics as per the prescribed dosage and course. Do not stop the medication when symptoms subside. Not completing an antibiotic course may cause the recurrence of infection with more severity. It may also lead to drug resistance, compromising your immunity and rendering the antibiotic no longer effective against the bacteria.
 Experts say
Experts sayWhat Is The Safest Antibiotic For UTI During Pregnancy?
According to a global survey published in the journal Antibiotics, urinary tract infections (UTIs) were found to be the most common infections requiring antibiotic treatment, accounting for a significant 67.9% of cases. When treating UTI during pregnancy, the choice of antibiotic may vary depending on the specific organism identified in the urine culture. Commonly prescribed include Amoxicillin, Ampicillin, Cephalosporins, Nitrofurantoin, and Trimethoprim-Sulfamethoxazole. Some recent findings suggest a link between the use of sulfa derivatives and Nitrofurantoin and congenital disabilities if prescribed in the first trimester. The most commonly used sulfonamide during pregnancy, Trimethoprim-Sulfamethoxazole, should be avoided in late pregnancy due to the potential risk of the newborn developing kernicterus (brain damage due to high bilirubin in the baby’s blood) (7).
Frequently Asked Questions
1. Which antibiotics can cause miscarriage?
Researchers have found that taking azithromycin during pregnancy may increase the risk of miscarriage by 65%. Antibiotics such as tetracyclines and quinolones also increase the risk of spontaneous miscarriage two to three times (8).
2. Do antibiotics pass through the placenta?
Yes. Some antibiotics, for example, ampicillin and methicillin, cross the placenta quickly and are found in equal concentrations in the maternal and cord plasma.
Other antibiotics, such as azlocillin and dicloxacillin, show incomplete transfer where the concentration of antibiotics is lower in cord plasma than in maternal plasma.
Ceftizoxime is the only antibiotic that shows a higher concentration in the cord plasma than in maternal plasma (9).
3. Can antibiotics cause preeclampsia?
A study conducted in 2013 showed that when antibiotics were given to women with urinary tract infections, they experienced an increased risk of preeclampsia. However, this was not the case when women with respiratory tract infections were treated with antibiotics. Therefore, the association of antibiotics with preeclampsia is still not clear. Further research is required to confirm it (10).
Infections during pregnancy may be prevented by maintaining good hygiene (washing hands regularly), eating well-cooked food, and avoiding unpasteurized food milk or milk products. Avoid coming in contact with cat litter or contaminated soil that may cause toxoplasmosis. Get vaccinations on time to prevent certain infections (8). This would reduce severe infections and help you avoid antibiotics during pregnancy.
Infographic: Pregnancy-Safe And Unsafe Antibiotics
During pregnancy, it’s crucial to ensure your safety while having medications, including antibiotics. In this infographic, we’ve provided a list of safe and unsafe antibiotics to take during pregnancy. Knowing about these medicines can help you avoid anything harmful; however, it is best to ask your doctor before taking any medicine.

Illustration: Momjunction Design Team
Pregnant and wondering if taking antibiotics is safe? Find out if antibiotics can harm you or your baby and some precautions you should take in this informative video.
References
- Silvie Bernatová et al; (2013); Following the Mechanisms of Bacteriostatic versus Bactericidal Action Using Raman Spectroscopy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6270526/ - Antibiotic Use during Pregnancy: Too Much of a Good Thing?
https://sph.umich.edu/pursuit/2020posts/antibiotic-use-during-pregnancy-too-much-of-a-good-thing.html - P. Brandon Bookstaver et al, (2015); A Review of Antibiotic Use in Pregnancy.
https://accpjournals.onlinelibrary.wiley.com/doi/full/10.1002/phar.1649 - Khashayar Farzam et al, (2021); Erythromycin.
https://www.ncbi.nlm.nih.gov/books/NBK532249/ - Antibiotic Use During Pregnancy and Lactation.
https://www.aafp.org/pubs/afp/issues/2006/0915/p1035.html - Antibiotics.
https://my.clevelandclinic.org/health/treatments/16386-antibiotics - Patricia J. Habak and Robert P. Griggs Jr.; (2021); Urinary Tract Infection In Pregnancy.
https://www.ncbi.nlm.nih.gov/books/NBK537047/ - 10 Simple Steps to Prevent Infections During Pregnancy.
https://www.healthychildren.org/English/ages-stages/prenatal/Pages/Simple-Steps-to-Prevent-Infections-During-Pregnancy.aspx - Part two: Can taking antibiotics during pregnancy increase risk of miscarriage?
https://utswmed.org/medblog/antibiotics-miscarriage/ - G M Pacifici; (2006); Placental transfer of antibiotics administered to the mother: a review.
https://pubmed.ncbi.nlm.nih.gov/16502764/ - Caroline Minassian; (2013); Acute Maternal Infection and Risk of Pre-Eclampsia: A Population-Based Case-Control Study.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3760871 - 10 Simple Steps to Prevent Infections During Pregnancy.
https://www.healthychildren.org/English/ages-stages/prenatal/Pages/Simple-Steps-to-Prevent-Infections-During-Pregnancy.aspx - Amir A. Kuperman and Omry Koren; (2016); Antibiotic use during pregnancy: how bad is it?
https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-016-0636-0 - Elizabeth C. Ailes et al., (2016); Antibiotic Use among Women with Urinary Tract Infections in the First Trimester of Pregnancy and Birth Defects.
https://stacks.cdc.gov/view/cdc/43819 - Medicine and Pregnancy.
https://www.fda.gov/consumers/free-publications-women/medicine-and-pregnancy - Sheng Zhang and De-Chang Chen; (2019); Facing a new challenge: the adverse effects of antibiotics on gut microbiota and host immunity.
https://pmc.ncbi.nlm.nih.gov/articles/PMC6511407/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Pamela Adhiambo Muga
Read full bio of Dr. Joyani Das
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das