Image: Shutterstock
Arthritis is a condition characterized by stiffening and swelling of joints resulting in decreased range of motion. Although this is a common geriatric problem, arthritis after pregnancy may occur in a few women. This condition could be due to physical changes after pregnancy and childbirth. It may be present for a few weeks or a few months after pregnancy. Postpartum arthritis may cause a lot of discomfort to the mother and may also impact her mental health and overall well-being. Hence knowing the right treatment and caring measures could be helpful. Continue reading the post for more information.
Key Pointers
- Pregnancy and childbirth can cause arthritis, which makes joints stiff and swollen.
- Arthritis can improve during pregnancy, but worsen after birth due to changes in the immune system.
- After giving birth, arthritis can also develop due to various factors such as aging, genetics, obesity, lack of physical activity, smoking, infections, occupation, and poor nutrition.
- Breastfeeding may not worsen rheumatoid arthritis after pregnancy, but some mothers with rheumatoid arthritis may experience severe pain while breastfeeding.
Is Arthritis Common After Pregnancy?
Arthritis is common in people of all ages. It may aggravate after pregnancy and a few women are likely to experience arthritis flare-ups or joint inflammation, after childbirth (1). They may have postpartum joint disorders that may cause pain in their wrists, hands, ankles, and feet.
According to gynecologist & obstetrician Dr. Nisarg Patel, “Pregnancy arthritis usually goes away after delivery, but some women may continue to have symptoms for a few months or longer. If your joint pain and stiffness persist beyond six weeks of delivery or interfere with your daily activities, you should see your doctor for a proper diagnosis and treatment.”
 Quick fact
Quick factCauses Of Arthritis After Delivery
New mothers may have postnatal joint discomfort or arthritis for the following reasons.
- During pregnancy, most autoimmune diseasesiRelated to conditions where the immune system attacks the body’s healthy cells due to a malfunction , such as rheumatoid arthritisiA condition where the immune system attacks the tissues lining the joints on either side of the body or psoriatic arthritisiType of arthritis seen in people with psoriasis, which is also an autoimmune condition causing itchy, red patches on the skin , go into remission because of the vigorous antibody and cell-mediated immune responses. The symptoms may again flare up after pregnancy (2).
Sharing her experience, Stephanie Kay, a mother of four and homeschool teacher, talks about how she always wanted to be a mother but feared how her rheumatoid arthritis would affect the pregnancy. After being on the medication Enbrel and therapy, she decided to have a baby and describes how her rheumatoid arthritis went into remission, allowing her to have a comfortable pregnancy. She says, “I jokingly tell my husband I would always feel great if I could stay 2nd trimester pregnant all the time (puking is over but I’m not as big as a barn). That may sound odd until you learn that for most women RA goes into remission (inactive) during pregnancy! The funny thing is that after the baby’s born RA usually rears it’s ugly head again. I’m no exception. 6 weeks after delivery I start feeling the old aches and pains and inflammation again (i).” - The immune system usually becomes stronger after pregnancy. The overactive immune system may lead to pre-existing allergies or autoimmune diseases such as rheumatoid arthritis (RA), lupusiA condition in which the immune system attacks its tissues, causing inflammation , or psoriatic arthritis (3).

- Age, genetics, obesity, physical inactivity, smoking, infections, occupation, and diet deficiencies may also lead to arthritis flare-ups during the postpartum period (4).
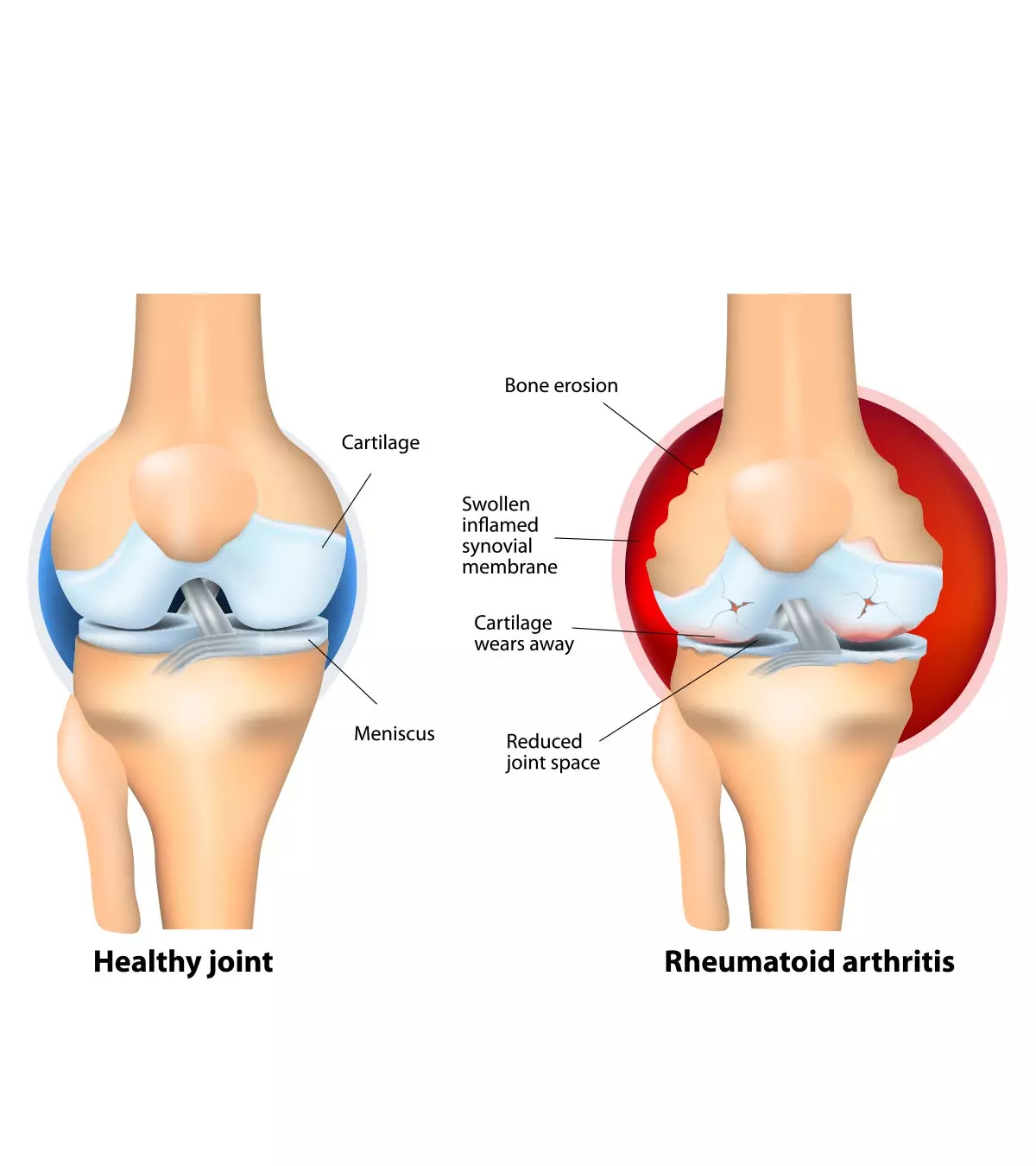
- Cartilage is a firm tissue that protects your bones and joints and an eventual cartilage damage can lead to osteoarthritisiA condition in which tissues in the join gradually break down and degrade over time where bones rub against bones.
- Hematogenous seedingiAn infection that spreads to other parts of the body through blood. of bacteria contacted during birth or from nipple trauma during breastfeeding may result in postpartum septic arthritis.
- The physiological effects of pregnancy, such as weight gain, water retention, and bearing an unbalanced load on loose joints, may cause wear and tear in the knees, triggering inherent genetic traits for arthritis postpartum (18).
Although postpartum musculoskeletal pain often results from injuries to bones or ligaments, it can also be associated with osteoarthritis and rheumatoid arthritis.
What Should You Do If You Have Postpartum Joint Pain or Arthritis?
Some measures that might help in managing and treating postpartum joint stiffness or arthritis are:
- See a doctor: Seek medical help if you already have arthritis. The doctor may give treatment to minimize pain, reduce joint damage, and improve the quality of life. You could only achieve them through regular follow-ups and by following the recommended treatment.
 Quick tip
Quick tip- Have a balanced diet: Plan a healthy post pregnancy diet with your nutritionist. Include low-calorie, low-fat foods, and plan your meals and snacks in a way that you are having a balanced diet. Your doctor may advise you to include omega-3-rich foods and supplements such as fish oil to help with inflammation and improve the health of joints and muscles (20).
- Manage your weight: Losing the excess weight and maintaining a healthy weight could be helpful if you have arthritis. It can lower the stress on joints, especially the hips and knees. Being overweight may also increase the risk of having arthritis. According to the US CDC’s Prevalence of Arthritis and Arthritis-Attributable Activity Limitation Report 2016–2018, about 28.8% of obese adults experience arthritis (19).
- Stay active: Being physically active by engaging in exercises could relieve pain and improve your mood. You may do a combination of different exercises, from aerobic workouts to strength training. Range of motion exercises, stretching, swimming, cycling, and walking can help maintain the flexibility and functionality of joints while increasing endurance. Strength training exercises, yoga, and pilates may help build muscles, stabilize joint supporting tendons, and improve overall physical strength (14). Exercising also decreases your chances of developing chronic conditions such as diabetes, hypertension, and heart disease. Speak to your doctor to know the safest postnatal exercises you can do to manage arthritis.

- Improve your self-management skills: You may join a self-management education program to learn skills to manage arthritis. It could help you gain control over your health, manage pain and its symptoms, reduce stress levels, improve mood, and communicate better with your doctor (5).
- Wear correct size comfortable footwear: Avoid high heels. Ensure the sole is soft and gives adequate cushioning.
- Get adequate rest: It is important to ensure that you rest while your joints feel stiff and painful to assist your body in remedying muscle fatigue and reducing inflammation. The period of rest will allow you to regain some lost energy and help you resume your exercise routine(14)(20).
- Avoid tobacco and alcohol: Studies indicate smoking as a risk factor for the development and worsening of rheumatoid arthritis(21). Similarly, consumption of alcohol may cause some interactions with medications prescribed for the management of arthritis, worsening the symptoms. Thus, lifestyle changes such as quitting smoking and reducing or avoiding the intake of alcohol are necessary to manage arthritis(14).
- Focus on your mental health: Pregnancy and postpartum are an intense period where the mother may constantly battle symptoms of stress and depression. Studies exploring the link between poor mental health conditions and arthritis indicate depression as a likely causal trigger for rheumatoid arthritis (22). Stress has also been linked with worsening the symptoms of arthritis. Thus, you must opt for suitable ways to relax postpartum including having regular massages or acupuncture, meditation, deep breathing, and visualization to cope with the symptoms (20).
However, despite making these lifestyle changes to manage arthritis, if you continue to experience uncontrollable symptoms due to recurring flare-ups after pregnancy, speak with your doctor.
Can You Get Rheumatoid Arthritis After Pregnancy?
There is a risk of developing autoimmune diseases such as rheumatoid arthritis after pregnancy. Although there is no substantial evidence to support this claim, there is a belief that complex hormonal changes and immune-related shifts occur during and after pregnancy. This could be a plausible reason for an increase in the rate of postpartum rheumatism (6). However, pregnancy alone need not be a reason for getting RA, as other factors such as genetics play a more important role.
Does Breastfeeding Make Rheumatoid Arthritis Worse?

Breastfeeding may not worsen rheumatoid arthritis. But some mothers with RA may have chronic pain while holding the baby for breastfeeding. It can also affect arthritis treatment since some medications aren’t safe during breastfeeding. Therefore, it is important to consult your healthcare provider to find pain relief options that are safe during breastfeeding.
Does Postpartum Arthritis Go Away?
Unfortunately, there is no cure for arthritis. However, early treatment and a healthy lifestyle could help you manage the condition and improve your quality of life (7).
Frequently Asked Questions
1. How do you diagnose rheumatoid arthritis?
For rheumatoid arthritis, doctors can suggest the following tests (8) (9):
- Physical examination to assess the swelling and joint mobility
- Blood tests
- Erythrocyte sedimentation rateiA blood test used to check for inflammation in the body to detect inflammation in the body
- C-reactive proteiniA liver protein, the presence of which indicates an inflammation to detect inflammation
- Complete blood count to know about general health
- Rheumatoid factor to check the antibody present in people with this condition
- Anti-cyclic citrullinated peptideiType of antibodies used as biomarkers for the detection of rheumatoid arthritis
- Joint scans
- X-rays
- MRI
- Ultrasound
- Arthroscopy, where a thin tube with light and camera is inserted in the joint to detect bone disease and tumors
2. Can pregnancy cause arthritis flare-ups?
In some women, the pain and swelling associated with rheumatoid arthritis seem to reduce during pregnancy. However, some women do not notice any changes, while a few others notice worsening symptoms. Therefore, discussing your symptoms with your doctor and creating a precise treatment plan is important. Also, since pregnancy is generally associated with backaches and swelling, the symptoms should not be confused with rheumatoid arthritis (10).
3. Can breastfeeding impact the likelihood of developing arthritis after pregnancy?
Studies suggest that the influence of postpartum hormones such as an elevated level of prolactin, a proinflammatory hormone during breastfeeding, may significantly increase the risk of developing rheumatoid arthritis (13). However, more research is needed to validate this finding.
4. Can arthritis after pregnancy affect future pregnancies?
The usage of certain medications for the treatment of rheumatoid arthritis has been shown to result in impaired fertility. Furthermore, the treatment options are limited during pregnancy, making flare-ups common after pregnancy (15). Therefore, it is better to consult with your doctor if you wish to conceive before any future pregnancies.
5. How long does it take for arthritis after pregnancy to resolve?
Arthritis, before or after pregnancy, has no cure; hence, limiting pain and managing symptoms is the only treatment plan available (16). Consult with your rheumatologist to undertake a specific symptom management plan for your case.
6. Can stress during pregnancy increase the risk of developing arthritis after pregnancy?
No medical evidence indicates a relationship between stress and the development of arthritis in mothers after pregnancy. However, first-time mothers may feel generally stressed or the post-partum blues after a few weeks of delivery (17). Therefore, feel free to contact your family to help you during this time.
Arthritis after pregnancy can get aggravated if you have a history of arthritis or if it is genetic. You must talk to a rheumatologist about its management during and after pregnancy to ensure it is under control. While postpartum joint inflammation and pain or arthritis cannot be cured, you can still take specific measures to manage it. It includes following a healthy lifestyle and taking a balanced diet. It is of great help to avoid inflammatory foods and be regular with any form of physical activity that you enjoy. Also, keep in mind not to cause excessive strain on your body.
Infographic: What You Should Know About Postpartum Arthritis?
Arthritis can be suppressed during pregnancy due to biochemical changes in the body. However, postpartum comes with an exacerbation of the condition. Timely management could help to deal with flares better. Go through the infographic to learn about postpartum arthritis. Illustration: Momjunction Design Team
Illustration: Postpartum Joint Pain (Arthritis) Causes And Tips To Manage

Image: Dall·E/MomJunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Rheumatoid Arthritis (RA), Pregnancy and Enbrel. https://stephaniesmommybrain.blogspot.com/2010/02/rheumatoid-arthritis-ra-pregnancy-and.htmlReferences
1. Pregnancy and Arthritis; Department of Orthopaedics and Sports Medicine – University of Washington
2. Beagley KW and Gockle CM; Regulation of innate and adaptive immunity by the female sex hormones oestradiol and progesterone; FEMS Immunol Med Microbiol (2003).
3. Immune System; healthdirect – Australian Government – Department of Health
4. What Are Common Symptoms of Autoimmune Disease; Johns Hopkins Medicine
5.Self-Care for Arthritis: Five Ways to Manage Your Symptoms; Centers for Disease Control and Prevention
6. Brittany Buening, Hendrickson S, and Smith C; Relationship between Pregnancy and Development of Autoimmune Diseases; Journal of Womens Health, Issues and Care (2017)
7. Treatment – Rheumatoid arthritis; NHS
8. Diagnosis-Rheumatoid arthritis; NHS
9. Arthritis Diagnosis; Johns Hopkins
10. Rheumatoid arthritis & pregnancy; National Rheumatoid Arthritis Society
11. Sana Qureshi, et al; New diagnosis of rheumatoid arthritis during the third trimester of pregnancy; NCBI (2016)
12. Pregnancy And Arthritis; UW Medicine
13. Breast-feeding and the onset of rheumatoid arthritis; NCBI
14. Lifestyle Changes for Rheumatoid Arthritis; NYU Langone
15. Current perspectives on fertility, pregnancy and childbirth in patients with Rheumatoid Arthritis; Science Direct
16. Arthritis; Johns Hopkins
17. Baby Blues and Postpartum Depression: Mood Disorders and Pregnancy; Johns Hopkins Medicine
18. Pregnancy and Arthritis; University of Washington
19. Prevalence of Arthritis and Arthritis-Attributable Activity Limitation — United States, 2016–2018; CDC
20. Rheumatoid Arthritis: Causes, Symptoms, Treatments and More; Arthritis foundation
21. Yuki Ishikawa and Chikashi Terao; The Impact of Cigarette Smoking on Risk of Rheumatoid Arthritis: A Narrative Review; NCBI (2020)
22. Isabelle A Vallerand, Scott B Patten, and Cheryl Barnabe; Depression and the risk of rheumatoid arthritis; NCBI (2019)
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sangeeta Agrawal
- Dr. Nisarg Patel is a gynecologist, obstetrician, and laparoscopic surgeon from Ahmedabad, India, with over 13 years of experience in the field. He did his post graduation in Obstetrics and Gynecology from Pravara Institute of Medical Sciences, Ahmednagar, and holds a fellowship of Reproductive Medicine.
 Dr. Nisarg Patel is a gynecologist, obstetrician, and laparoscopic surgeon from Ahmedabad, India, with over 13 years of experience in the field. He did his post graduation in Obstetrics and Gynecology from Pravara Institute of Medical Sciences, Ahmednagar, and holds a fellowship of Reproductive Medicine.
Dr. Nisarg Patel is a gynecologist, obstetrician, and laparoscopic surgeon from Ahmedabad, India, with over 13 years of experience in the field. He did his post graduation in Obstetrics and Gynecology from Pravara Institute of Medical Sciences, Ahmednagar, and holds a fellowship of Reproductive Medicine.
Read full bio of Rebecca Malachi
Read full bio of Swati Patwal
Read full bio of Dr. Joyani Das

















