Breathing is a natural process the baby learns inside the womb itself. Newborns often have irregular breathing patterns, so counting their breaths for a full minute is vital to ensure everything is normal (1). Usually, there is little to worry about, but sometimes, there could be a problem with the baby’s breathing patterns.
Therefore, it is good for parents to know about normal infant breathing and how to spot anomalies in the pattern.
MomJunction tells you about the signs of breathing problems and how to help babies breathe properly. But first, let’s understand what ‘normal breathing’ means.
Key Pointers
- Pauses or gasps while breathing are normal for newborns.
- Breathing patterns may vary based on sleeping or feeding patterns.
- Periodic breathing is when a newborn stops breathing for up to 10 seconds before resuming normal breathing.
- If there are any unusual or persistent changes in breathing, parents should seek medical consultation.
What Is Normal Breathing In Babies?

Here are a few things you should know to understand what ‘normal breathing’ is in babies.
- Babies breathe faster: Infants breathe faster than older children and adults. An average infant, especially a newborn, has about 40 to 60 breaths in a minute while awake. The respiratory rate in infants slows down to only 30 to 40 breaths in a minute when asleep (2).
 Did you know?
Did you know?- More than 60 breaths per minute is possible: A baby may sometimes take more than 60 breaths per minute, especially when they are excited or crying. The breathing will return to the usual frequency when they calm down. However, if it continues to be more than 60, then it might be a concern (3).
- Belly breathing is normal: Babies usually indulge in diaphragmatic breathing, which causes the belly to move as the baby breathes in and out (4). We all are born with the ability to breathe this way but move on to chest breathing as adults, while babies practice belly breathing, which is the ideal way to breathe (5).
According to Po-Chang Hsu, MD, MS, Greater Boston-based medical expert, “Babies breathe with their stomachs because their intercostal musclesiThe muscles between the ribs are not developed enough yet. Instead, they use the abdominal muscles to encourage diaphragmatic breathing.”
- Babies could pause while breathing: A baby could breathe rapidly and pause for a maximum of ten seconds before resuming normal breathing (6). Parents who constantly watch their baby breathing while asleep could worry about it, but it is completely normal. Such a breathing pattern is called periodic breathing.
- Breathing accompanied by sound: Babies can breathe only through their nose. The small nasal passages and the presence of mucus can make the baby’s breathing a bit noisy. Some noise while breathing even without a cold is a normal occurrence (7). If the blockage due to mucus is severe, then the baby will sneeze as a natural reflex to clear the nose.
Dr. Steven Goudy, a pediatric ENT specialist in Atlanta, says, “Noises while breathing continue through life, and you likely don’t notice them when your child is older as you are not continually monitoring their breathing.”
Spotting abnormal breathing patterns becomes easier when you know what normal breathing is in babies.
What Are The Signs Of Breathing Problems In A Baby?

A deviation from the usual breathing pattern could indicate a breathing problem. Here are the signs you should check for to know if the baby has problem breathing (3):
- Rapid breathing: Rapid breathing of more than 60 breaths per minute. A baby may breathe rapidly when excited or crying, but not when sleeping or calm. If the baby always breathes rapidly, check for symptoms of illness such as fever, fussiness, and coliciA unique pattern of fussiness, frequent, or prolonged crying in infants for no known reason . Check if the baby also shows signs of distress, such as difficulty feeding or increased fussiness.
- Irregular breathing with extended pause: If the baby pauses more than ten seconds, it is a cause for concern. If the break goes beyond 20 seconds, it could be a sign of apnea, obstructed breathing due to constricted airways, or apnea of prematurity, a condition in premature babies (8). A study found that preterm infants rely more on holding their breath after exhaling to maintain their lung volume (9).
- Breath-holding attacks: These are common and can occur when the baby is crying. While crying, the baby may suddenly hold their breath for a few seconds. When the baby does this, the mother may give a few light thumbs at the back. This recovers the breath even if the crying continues. Rarely, it can cause circumoral cyanosisiAbluish discoloration of the skin around the mouth caused by low oxygen levels in the blood. , a harmless condition. If the baby tends to hold their breath often, consult a doctor to confirm that it is a breath-holding attack and nothing pathological.
Brooke Benoit, who documents her eight-month-old baby’s breath-holding incident, says, “My first daughter was a few months old when she sneakily held her breath on me for the first time. She was crying, but I didn’t realize that she was also holding her breath.
“When her little body went limp in my arms—I think that was the worst feeling I have ever had in my life. I nearly passed out, too, but she did come around fairly quickly. She was slightly dazed for a few minutes. If I hadn’t known about breath holders, I’m sure we would have been en route to the emergency room instead of reassuringly cuddling each other (i).”
- Flared nostrils: According to the National Heart, Lung, and Blood Institute, flared nostrils can be a warning sign of a breathing problem in newborns (10). If the baby has trouble getting sufficient air into the airways, the nostrils will flare or widen during each inhalation.
- Mouth breathing: If the baby prefers breathing through the mouth, then it could be an indicator of an inflamed tonsil or adenoidiRectangular lymph tissues found in the upper airway, between the nose and the back of the throat. due to infection (11). Such a condition can cause obstructive sleep apnea, which leads to problems while breathing.
- Strained breathing with a retraction: Did you notice the baby straining his/her chest inwards during each breath? The infant is quite probably straining to get enough air into the lungs, which is a sign of a breathing problem. In breathing problems, a depression generally develops between the rib cage and abdomen, and the muscles between the ribs (12). Increased respiratory rate, together with the above signs, might need an immediate doctor consultation.
- Constant coughing and wheezing: A cough once in a while is okay, but if persistent, then it indicates a problem. However, a wheeze indicates constriction of the air passages. Coughing and wheezing could be more common if the baby suffers from an allergic condition or bronchospasmiTightening of the muscles that line the bronchi (13). Assessment by a doctor is necessary.
 Quick fact
Quick factWhen To Take The Baby To A Doctor?

Take the baby to the doctor in the case of:
- Extremely rapid breathing: If the infant’s respiration rate is more than 60 per minute or the above signs of depression between the thoracic cage as well as intercostal recession is present, then the baby could be breathing at least 80 times per minute. Such rapid breathing is medically called tachypnea in infants (15). On the other hand, if your baby is having an extremely slow breathing rate, it could be indicative of bradypneaiAbnormally slow breathing rate. in infants requiring medical attention.
- Grunting: A grunt is a loud breathing sound which is audible. If the baby grunts with every breath, then it could indicate pediatric respiratory distress (6).
- Stridor: It is the sound you hear when the baby inhales and is audible when you stand close to a baby. This is the effort made by the baby while inhaling and indicates upper respiratory tract inflammation and is known as stridor. One of the treatment options is to use a humidifier. This viral condition is very common in winter. The raspy breath could be due to congenital anomalies in the pediatric respiratory system (15). In rare cases, it can be due to a congenital condition called laryngomalaciaiA condition where the soft tissues of the larynx or voice box collapse inward during breathing. (7).
- Blue coloration of skin: The color of the skin turns blue around the fingertips, cheeks, and the lips, indicating a severe respiratory problem called cyanosis. A baby with the condition could have low blood oxygen levels and even cardiac complications that need immediate medical care (3).
- Wheezing and whistling Sounds: Wheezing or whistling noises during breathing might signal an underlying respiratory issue, warranting prompt medical attention (16).
Timely diagnosis and treatment are necessary to correct any breathing problem that the baby has.
How Are Breathing Problems In A Baby Treated?

The correction of a breathing problem entirely depends on the diagnosis of the fundamental cause of the problem. The doctor will make a diagnosis based on the symptoms and check the breathing pattern using a stethoscope or by performing a pediatric pulmonary function test.
The following treatment steps could be used for the correction of breathing problems:
- Medication: In some cases, the illness can be treated with oral medication. Steam inhalation and nebulizationiA method of administering medications by turning liquid medicine into a fine inhalable mist through a facemask are important. Simple nebulization with normal saline is helpful. In other cases, nebulization with bronchodilatorsiA drug that helps open up the small airways by relaxing the muscles in the lungs. is needed under medical guidance.
- It is important to treat the underlying condition. Treat the infection, inflammation or bronchospasm.
- Breathing apparatus: Some respiratory ailments can be corrected using a breathing apparatus. An example is sleep apnea, which can be treated using a continuous positive airway pressure (CPAP) face mask attached to an electronic device, which allows the child to breathe normally (17).
 Quick tip
Quick tipTo ensure timely treatment of a baby’s breathing problem, parents should be observant of the baby’s breathing patterns and check if they are okay from time to time.
How Often Should Parents Check The Baby’s Breathing?
Ideally, you can check on the baby’s breathing once or twice a day. Perhaps the best time to do it is when the baby is having a nap or has just fallen asleep for the night. Here is how you can check your baby’s breathing:
- Check for abnormal sounds: Stand close and listen for any unusual sounds like baby grunting, whistling, etc. You can also hear the baby’s breath to check if it is okay.
Dr. Goudy adds, “Noises that occur when babies are breathing can be stertor (sound of a bad cold or congestion), stridor (high-pitched noise of difficulty breathing when breathing in with conditions, including croupiAn infection of the upper airways that leads to narrow airways, breathing difficulty, and a bark-like cough ), wheezing (noisy breathing or whistling when exhaling that can occur with asthma, RSV, or narrowing of the lower airway), snoring (choking/gasping sound that can occur when the airway is obstructed).“
- Observe movements of distress: See for any indicators of abnormal chest movements. Check if the baby’s chest seems to retract or move faster than it should.
- Look for other symptoms: A baby could have abnormal breathing in case he or she has a fever or other flu symptoms. You can check for temperature by touching the baby’s forehead and heart rate by holding the baby’s wrist. Assessing the fingertips for blue coloration is another way to check for a respiratory problem.
- Observe changes in the baby’s behavior and routine: Is your baby fussy more often? Is the baby lethargic? Does he or she feel lethargic and show no interest in playing? All these symptoms, along with the presence of abnormal breathing, could indicate a problem.
How Can You Ensure The Baby Gets To Breathe Properly?
The following tips can help (19):
- Let the baby sleep on his or her back: Sleeping on the back is the best sleep position for a baby. It ensures that the esophagusiThe pipe that carries food and liquid from the mouth to the stomach stays lower than the tracheaiThe pipe that helps air travel from the voice box to the airways of the lungs. and does not allow regurgitated food from accumulating at the opening of the trachea. Putting the baby to sleep on the tummy or side can cause regurgitated food to gather near the opening of the trachea, thus leading to breathing problems and even choking.
- Keep the baby’s crib empty: Do not stuff the infant’s crib with soft toys and other bedding. Your baby’s sleeping area should be bare. Placing objects around increases the risk of obstructing the baby’s breathing and can even lead to SIDS (sudden infant death syndrome). According to the US CDC’s National Vital Statistics Data 2020, 41% of unexpected infant deaths were due to SIDS.
- Reduce exposure to allergens and irritants: Keep the baby away from pollution, dust, etc., and avoid using perfumes or sprays if the baby has allergies.
- Sleep with the baby in the same room: Pediatric experts recommend parents and babies to sleep in the same room, with the baby in his or her crib, till the age of six months and preferably till one year. It helps you detect any complications or problems with breathing.
- Keep baby away from smoke: Smoke, especially tobacco smoke, can cause inflammation of the infant’s airways and may increase the risk of infant sleep apnea (20). For this reason, make sure the baby’s room is free of smoke and even dust. Never smoke or let others smoke around the baby.
Frequently Asked Questions
1. What happens when a baby is born with breathing problems?
Respiratory distress syndrome and transient tachypnea are commonly diagnosed conditions among newborns. Both conditions have similar symptoms of rapid and noisy breathing, retractions, cyanosis, and flaring nostrils. However, infant respiratory distress syndrome individuals have inadequate surfactant (a fatty substance in the lungs that makes the alveoli open and close easily), resulting in insufficient oxygenation or hypoxia in infants. Doctors use lung imaging tests, heart tests, and blood tests to diagnose this condition (21). In either case, children require oxygen, medication, and continuous positive airway pressure (CPAP) to keep their lungs from collapsing while expelling the carbon dioxide and lung fluids from the body (14) (22). Children with either condition may start recovering within three to four days.
2. How should I check my child’s breathing rate?
Parents can measure the number of respirations per minute in a resting child by setting a timer for one minute and counting the number of times the child’s abdomen rises. Please note that one respiration cycle includes both the rise and fall of the abdomen. Parents can also place their fingertips on the belly (without pressure) to get an accurate number.
3. How does a baby’s breathing pattern change as they grow?
A baby’s breathing pattern changes as they grow. According to the Centers for Disease Control and Prevention, the respiratory rate is 40–60 breaths per minute during the first month. By six months, it decreases to 25–40 breaths per minute (23). Then, it’s 24-40 breaths between one and three years. From three to six years, it decreases to 22-34 breaths, and from six to 12 years, it further reduces to 18-30 breaths. Finally, from 12 to 18 years, the rate is 12-16 breaths per minute (24).
4. Can environmental factors such as pollution or cigarette smoke affect a baby’s breathing pattern?
Yes, environmental factors like pollution or cigarette smoke can impact a baby’s breathing pattern. Several studies have established a connection between parental smoking and respiratory diseases, causing detrimental health effects in children. These include acute respiratory illnesses, coughing, phlegm, middle ear disease, and hindered lung development (25)
Parents often find it a lovely sight to watch their babies breathe while asleep. You may be worried about hearing some abnormal sounds or patterns while looking at the baby. However, do note that babies make several different noises while breathing and not all of them are abnormal. If you have any doubts, do not hesitate to ask your healthcare professional about them. If the baby looks distressed, shows signs such as bluish discoloration of the lips and skin, or retraction between the ribs, you should seek immediate medical attention.
Infographic: What Causes Abnormal Breathing Patterns In Babies?
Abnormal breathing patterns in babies can occur during various respiratory conditions. Associated signs and symptoms may help to identify the cause. It is recommended to seek pediatric consultation to diagnose and treat breathing issues in babies. Go through the infographic to learn more about the causes of abnormal breathing patterns in babies. Illustration: Momjunction Design Team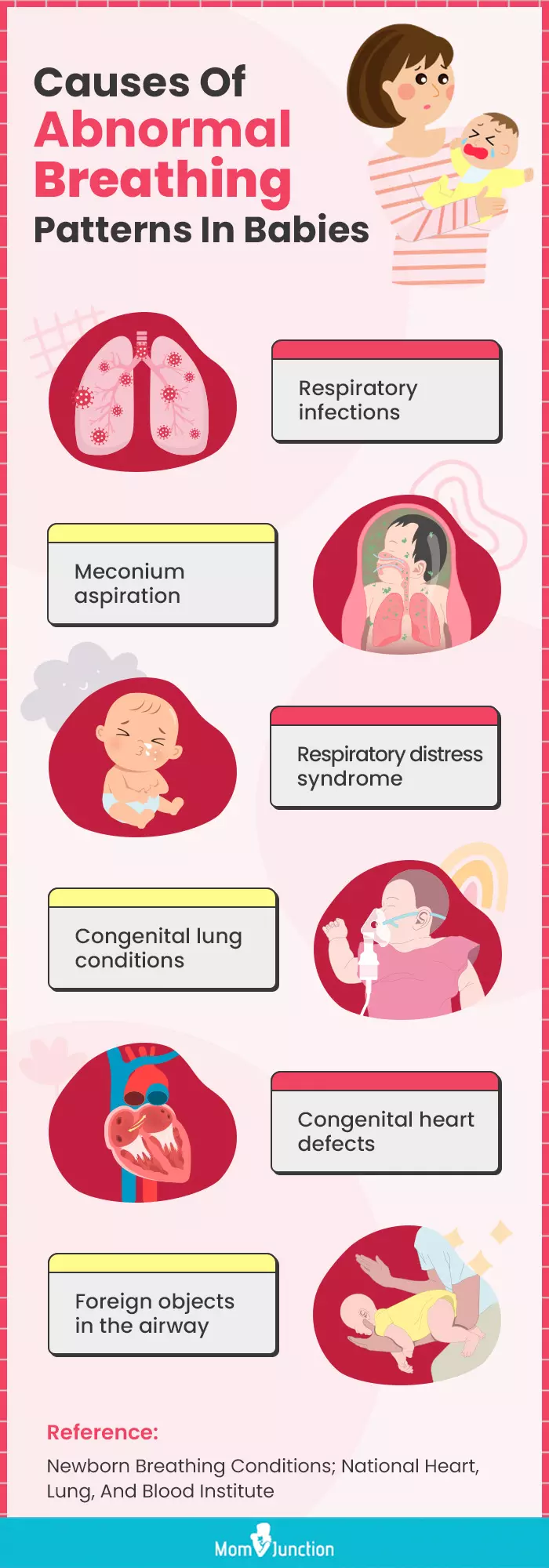
Illustration: Baby Breathing Patterns: What Is Normal And When To Worry

Image: Stable Diffusion/MomJunction Design Team
Take a look at this informative video that might answer a few of your common concerns about your little one’s breathing patterns.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. PSA: Breath-Holding, Parent-Terrifying Babies.https://sheerfluency.wordpress.com/2009/12/27/psa-breath-holding-parent-terrifying-babies/
References
- Newborn Warning Signs.
https://www.nationwidechildrens.org/conditions/health-library/newborn-warning-signs - Breathing Problems In Newborn; University of Utah
https://healthcare.utah.edu/the-scope/kids-zone/all/2017/12/breathing-problems-newborn - Breathing Problems; Stanford Children’s Health
https://www.stanfordchildrens.org/en/topic/default?id=breathing-problems-90-P02666 - Learning diaphragmatic breathing; Harvard Health Publishing
https://www.health.harvard.edu/healthbeat/learning-diaphragmatic-breathing - Breathing differences between children and adults; Christopher & Dana Reeve foundation
https://blog.christopherreeve.org/en/life-after-paralysis/breathing-differences-between-children-and-adults - What might breathing problems indicate in a newborn?; University of Rochester Medical Center
https://www.urmc.rochester.edu/encyclopedia/content.aspx?contenttypeid=90&contentid=p02666 - Stridor Versus Wheezing: When Noisy Breathing Is Something More; Johns Hopkins Medicine
https://www.hopkinsmedicine.org/health/conditions-and-diseases/stridor-versus-wheezing - What Is Apnea?; Nationwide Children’s Hospital
https://www.nationwidechildrens.org/conditions/apnea - Arjan B te Pas et.al; Breathing Patterns in Preterm and Term Infants Immediately After Birth; Pediatric Research (2009)
https://idp.nature.com/authorize?response_type=cookie&client_id=grover&redirect_uri=https%3A%2F%2Fwww.nature.com%2Farticles%2Fpr200967 - Newborn Breathing Conditions- Symptoms; National Heart, Lung, and Blood Institute
https://www.nhlbi.nih.gov/health/newborn-breathing-conditions/symptoms - Tonsils and Adenoids; American Academy of Otolaryngology–Head and Neck Surgery Foundation
https://www.enthealth.org/conditions/tonsils-and-adenoids/ - Intercostal retractions; National Library of Medicine
https://medlineplus.gov/ency/article/003322.htm - Yehia M El-Gamal and Shereen S El-Sayed; Wheezing in infancy; National Library of Medicine (2011)
https://pmc.ncbi.nlm.nih.gov/articles/PMC3651148/ - Respiratory Distress Syndrome.
https://kidshealth.org/en/parents/rds.html - Lungs/chest – Tachypnea; Stanford University
https://med.stanford.edu/newborns/professional-education/photo-gallery/lungs-chest.html#tachypnea - Newborn Breathing: What is Normal & What Is Not; St. Louis Children’s Hospital
https://www.stlouischildrens.org/health-resources/pulse/newborn-breathing-what-is-normal-and-what-is-not - Obstructive Sleep Apnea; Children’s Hospital of Philadelphia
https://www.chop.edu/conditions-diseases/obstructive-sleep-apnea - Newborn Breathing Conditions-Treatment.
https://www.nhlbi.nih.gov/health/newborn-breathing-conditions/treatment - Frequently Asked Questions (FAQs) About SIDS and Safe Infant Sleep; NIH
https://safetosleep.nichd.nih.gov/reduce-risk/FAQ - V. Krishnan S. D. Williams J. D. Thornton; Where There Is Smoke…There Is Sleep Apnea; NCBI (2014)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4251622/ - Respiratory Distress Syndrome (RDS); National Heart, Lung, and Blood Institute
https://www.nhlbi.nih.gov/health/respiratory-distress-syndrome - Transient Tachypnea of the Newborn (TTN); Nemours.
https://kidshealth.org/en/parents/ttn.html - Respiratory Rate; CDC
https://www.cdc.gov/dengue/training/cme/ccm/page57286.html - Pediatric Respiratory Rates (breaths per minute)
https://www.health.ny.gov/professionals/ems/pdf/assmttools.pdf - Respiratory Effects in Children from Exposure to Secondhand Smoke
https://www.ncbi.nlm.nih.gov/books/NBK44318/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Mubina Agboatwalla
- Dr. Steven Goudy is a pediatric ENT, the director of pediatric otolaryngology, vice-chairman of research at Emory and Children’s Hospital of Atlanta. An alumni of University of Louisville School of Medicine, Dr. Goudy holds around 18 years of experience in pediatric otolaryngology. He is the founder of Dr. Noze Best, a battery-powered nasal suction device for infants.
 Dr. Steven Goudy is a pediatric ENT, the director of pediatric otolaryngology, vice-chairman of research at Emory and Children’s Hospital of Atlanta. An alumni of University of Louisville School of Medicine, Dr. Goudy holds around 18 years of experience in pediatric otolaryngology. He is the founder of Dr. Noze Best, a battery-powered nasal suction device for infants.
Dr. Steven Goudy is a pediatric ENT, the director of pediatric otolaryngology, vice-chairman of research at Emory and Children’s Hospital of Atlanta. An alumni of University of Louisville School of Medicine, Dr. Goudy holds around 18 years of experience in pediatric otolaryngology. He is the founder of Dr. Noze Best, a battery-powered nasal suction device for infants. - Dr. Po-Chang Hsu is a medical doctor and medical content expert. He received his medical doctor's degree from Tufts University School of Medicine in Boston in 2016. Before that, he did a master’s degree at Harvard University and wrote a thesis on neuroimaging in schizophrenia patients at Brigham and Women’s Hospital.
 Dr. Po-Chang Hsu is a medical doctor and medical content expert. He received his medical doctor's degree from Tufts University School of Medicine in Boston in 2016. Before that, he did a master’s degree at Harvard University and wrote a thesis on neuroimaging in schizophrenia patients at Brigham and Women’s Hospital.
Dr. Po-Chang Hsu is a medical doctor and medical content expert. He received his medical doctor's degree from Tufts University School of Medicine in Boston in 2016. Before that, he did a master’s degree at Harvard University and wrote a thesis on neuroimaging in schizophrenia patients at Brigham and Women’s Hospital.
Read full bio of Rohit Garoo
Read full bio of Dr. Ritika Shah
Read full bio of Ghazia Shah