
Image: iStock
Ear infection in babies usually refers to middle ear infection. The middle ear is part of the ear that contains the vibrating bones of the ear. This air-filled space behind the eardrum is an optimal site for the growth of microorganisms, and ear infections in infants are quite common (1) (2).

An ear infection could make the baby irritable and cause irreversible effects if left untreated. Since babies cannot express their discomfort in words, knowing the symptoms is crucial to prevent the infection from worsening. Read on to know the signs, diagnosis, and treatment for ear infections in babies.
Key Pointers
- Ear infections are caused by fluid buildup in the middle ear and subsequent bacterial or viral infection.
- They are common in babies below two years of age due to the small size of their eustachian tube.
- Symptoms may include ear pain, fussiness, sleeping trouble, and pulling at the ear. Fever, loss of appetite, and fluid release from the ear may also occur.
- When left untreated, ear infections can lead to more serious complications such as hearing loss and meningitis in babies.
- Doctors may prescribe antibiotics and painkillers to treat ear infections in babies.
What Are The Types Of Ear Infection?
There are four types of ear infections.
- Acute otitis media: It occurs when the middle ear gets inflamed or infected. Acute otitis media could be very painful and is the most common pediatric infection type. It usually is a result of respiratory infections (3).
A study showed the association between hearing loss in adulthood and Acute Otitis Media (AOM) in early childhood. AOM or recurring AOM during childhood may lead to permanent hearing loss. The graph depicts the age at which the final episode of AOM infection occurred. It can be inferred from the graph that more than 50% of patients who have had at least one AOM infection have had their final case of AOM by the age of eight.

Count of patient ages during final acute otitis media (AOM) infection
Source: Association between otitis media infection and failed hearing screenings in children; PLOS ONEHence, close monitoring in a high-risk population for relapse or temporary hearing loss is necessary for timely diagnosis and to prevent permanent hearing loss.
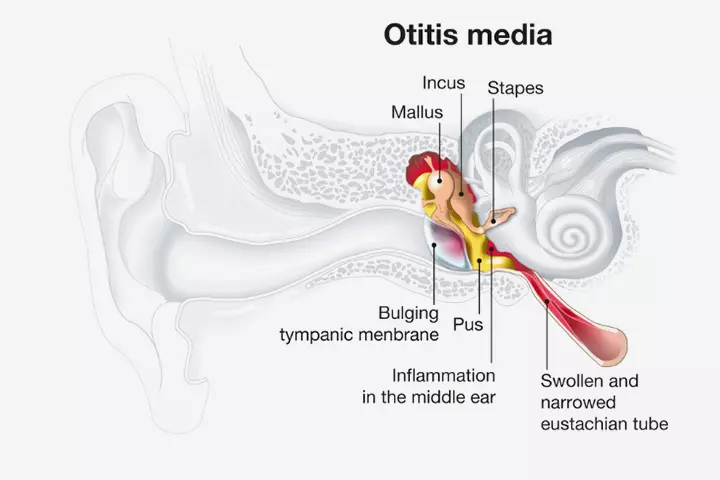
- Otitis media with effusion: In this type of ear infection, there is fluid accumulation in the ear canal. This fluid may not be infected and is usually accompanied by other symptoms such as distorted hearing, fever, or pus-buildup.
- Chronic otitis media with effusion: It occurs when the fluid in the middle ear stays for long and may become infected. The persistent presence of fluid in the middle ear may affect the baby’s hearing.
- Chronic suppurative otitis media: It is a persistent ear infection, which can lead to a ruptured eardrum and recurrent discharge from the ear. This infection may often occur due to advanced acute otitis media (4).
Why Are Babies More Prone To Ear Infections?
There are three primary reasons why ear infections are common among babies (5).
- Underdeveloped immunity: A baby’s immunity is still developing. Hence their body takes time to recognize and fight any infections.
- Smaller Eustachian tubes: An Eustachian tube connects the middle ear to the back of the throat. There is a tube each from each ear. In adults, the Eustachian tube is inclined and easily drains any excess fluid from the ears. However, in babies, the tube is smaller and leveled. As a result, there is a higher risk of fluid buildup, causing it to potentially harbor pathogens.
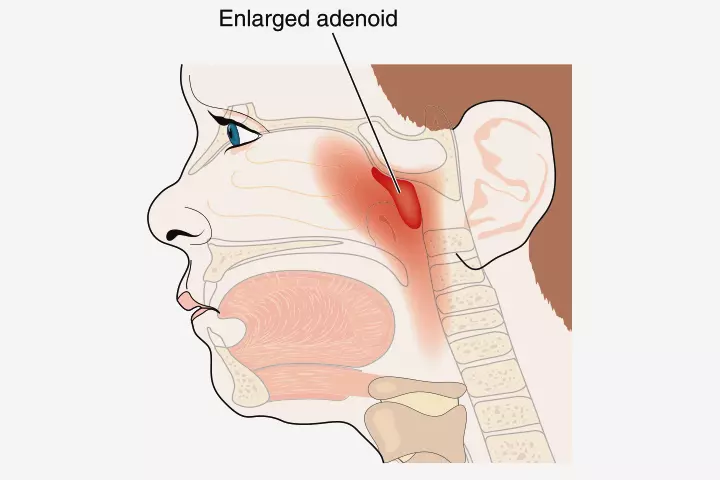
- Swollen adenoid: An adenoid is a type of tonsil tissue and part of the lymphatic system, which provides immunity. The tissue is located near the Eustachian tubes. The adenoid may trap viruses and bacteria. However, sometimes these pathogens may lead to infection, which may spread to the ear due to the proximity of Eustachian tubes to the adenoid.
How Long Do Ear Infections Last In Babies?
Most ear infections in babies are due to other respiratory illnesses. In such cases, usually, the infection recedes on its own within two or three days. However, if the ear infection persists for more than three days, it could be chronic. A chronic ear infection may take up to six weeks or more to subside (6).
What Causes An Ear Infection?
Ear infection in a baby could be due to the following factors (7).
- Common cold: Since the ear canal and the respiratory tract lie close to each other, a microorganism may reach the ears during a common cold. This infection may cause a fluid buildup, making the ears an optimal site for the growth of microorganisms.
 Be watchful
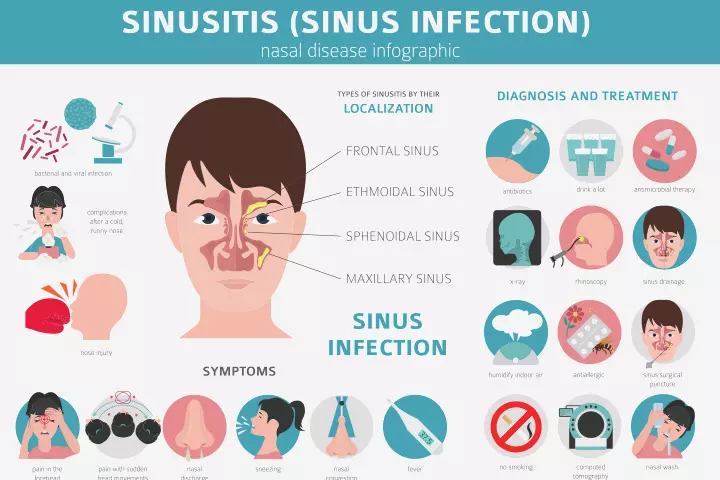
Be watchful- Sinus infection: This condition is due to the swelling of the lining of the sinuses and the nose. The swelling creates pressure on the ear and may lead to an ear infection.
- Bottle propping: It is a method of bottle-feeding where a baby lies on their back with the bottle in the mouth. This position may cause milk to accumulate in the mouth and then quickly flow to the back of the throat due to gravity from where it may reach the middle ear through the Eustachian tubes. Once in the middle ear, the milk may not drain quickly and become a breeding ground for pathogens that cause ear infections (8).
What Are The Associated Symptoms Of Ear Infection?
If your baby has an upper respiratory tract infection, you may expect an ear infection. Although your baby cannot express the reason, the following symptoms could help you interpret an ear infection in babies (9).
- Ear pain: If you notice your baby tugging or pulling their ears, it could be a sign of earache. They may also have trouble sleeping, seem fussy, and would be crying frequently.
- Fever: A fever may occur even before the ear infection becomes noticeable. Fever is a more common sign of ear infection among infants.
- Poor hearing: The accumulation of fluid in the middle ear could hinder the passage of sound and may decrease the baby’s hearing abilities. You may notice that they show delayed responses to your auditory cues.
- Decreased appetite: The baby may feel pain when they open their mouth due to the swollen Eustachian tubes. This may cause your baby to refuse milk or food (10).

- Fluid drainage: The release of yellowish fluid from the ear is a common sign of an ear infection. Unlike ear wax, this fluid may be cloudy, have a foul odor, and sometimes be blood-tinged. Fluid draining from the ear often indicates pus buildup within the ears. In about ten percent of cases, bloody pus drainage may indicate a ruptured eardrum caused by a bacterial ear infection, requiring medical attention (11) (12).
- Loss of balance: An infection in the semi-circular canals of the inner ear can cause fluid buildup and pressure within this part of the ear. These canals are vital for detecting and transmitting signals related to physical movements to the brain. Pressure in the inner year can disrupt this sensory transmission and cause the baby to display signs of dizziness, unsteadiness, clumsiness, nausea, and involuntary eye movements (13) (14).
 Caution
CautionWhat Are The Risk Factors For An Ear Infection?
There are a few factors that put a baby at risk of ear infections (1):
- Age: Babies between the ages of six months and two years are more prone to ear infections due to shorter Eustachian tubes.
- Bottle-fed babies: If bottle-feeding babies are made to consume milk while lying on their backs, they are more likely to develop an ear infection.
- Cleft palate: Babies with cleft palate have a few differences in bone structure. This may make the drainage of fluid from the Eustachian tubes difficult.
- Pollution: Air with pollutants, including tobacco smoke, may make a baby more prone to upper respiratory infections and ear infections.
- Seasonal allergies: Ear infections could be common during the pollen seasons as these environmental agents could trigger an allergic reaction. Fall and winter are the common seasons when these reactions are triggered. Allergies may increase the chances of fluid accumulation in the middle ear.
- Nursery: Childcare centers could have many babies and children staying in close proximity. That increases the risk of contracting viral or bacterial infections in babies compared to staying home.
- Genetics: As per a study, genetics play a moderate but significant role in both recurrent acute otitis media and chronic otitis media with effusion (15).
How Is An Ear Infection Diagnosed?

The following methods may help diagnose an ear infection (5).
- Baby’s medical history: The medical professional may ask if the baby experienced any infection, especially respiratory infection, recently. The doctor may also ask if the baby had ear infections in the past and for how long the symptoms have been present.
- Physical examination: A device called a pneumatic otoscope would be used to study the inside of an ear canal. The doctor would blow air using the otoscope into the baby’s ear. In healthy conditions, the eardrum would move. However, if the ear is infected, the eardrum would show little to no movement, indicating there is fluid in the middle ear behind the eardrum.
- Tympanometry: This device helps detect an ear infection by studying the movements of the eardrum. The device has a speaker and microphone. One can alter the air pressure and the sound tones of the device. The movement of the eardrums in accordance with the varying tones and pressures is measured. An impaired movement could indicate an ear infection.
How Is An Ear Infection Treated?
If the ear infection is not severe, the doctor may prescribe you an analgesic for pain relief and adopt a watchful waiting period of two to three days. No further treatment may be suggested if the ear infection recedes within these observation times. Otherwise, one of the following treatment plans may be considered (6) (16).
- Antibiotics: Antibiotics should not be prescribed as a primary treatment for a baby. Recurring antibiotic treatment could make a baby antibiotic-resistant and impact future medical care. Antibiotics could be prescribed if the infection continues after the observation period. They may be administered through an oral form or as ear drops. If the medical professional prescribes an antibiotic, follow the prescribed course. Do not discontinue the usage if the pain or infection subsides unless directed by the doctor.
- Pain medications: The doctor may prescribe regular over-the-counter medications, such as acetaminophen, to relieve ear pain in babies. Any pain medication must be used after consulting a doctor. Never give aspirin to a child as it may cause Reye’s syndrome (17).
- Ear tubes: These are also known as tympanostomy tubes and help treat chronic ear infections. The procedure may be considered if antibiotics fail. These tubes would be placed within the baby’s ear and left there for a few weeks or months. This tube helps drain the trapped fluid from the infected middle ears. The installation is harmless and is a ten-minute procedure. The tube usually stays for six to twelve months and falls out on its own. If the tube does not fall out, it can be removed by the doctor.
Amber, a mother, shares her daughter Baker’s experience with ear tubes. Baker had a severe and persistent ear infection, which antibiotics failed to treat. So, she got tubes. Amber says, “Since her (Baker) surgery, many things are startling her, things that would have never bothered her before. We have a train that passes the house about 17 times/day, and she got freaked out by the horn the first time she heard it. Tears were falling, and I couldn’t help but think that she was hearing it truly for the first time.
“After the hearing test and seeing how she’s improved since the tubes were placed, it is evident that she had a hearing level as we do if we were underwater.. lots of muffled sounds! With everything coming through as it should, she is surprised multiple times daily by how clear she can hear now (i).”
- Surgery: Surgical treatment for chronic otitis media may usually be suggested for babies with other conditions such as cleft palate or Down syndrome.
 Quick tip
Quick tipWhat Happens If A Baby’s Ear Infection Goes Untreated?
A few complications may arise out of untreated and recurring ear infections (18).
- Cholesteatoma: It is an abnormal tissue growth on or behind the eardrum. This growth may pose a problem by preventing the drainage of fluids from the ear. It may also cause mild hearing loss and changes in the structures of the ears’ bones (19).
- Hearing loss: Fluid accumulation in the ears could cause temporary or permanent hearing loss. Chronic fluid buildup may also affect the inner ear in the long run.
- Rupture of the eardrum: Chronic fluid accumulation and infection of the middle ear may create pressure on the eardrum. It may result in a small tear in the eardrum and may heal within two weeks after treatment.
- Mastoiditis: A bone called mastoid protects the delicate parts of the ear. Middle ear infections could cause mastoiditis, an inflammation of the inner lining of the bone (20).
- Meningitis: The inflammation of the protective membranes around the brain is called meningitis. It may occur when the pathogens from the ear infection enter the cerebral spinal fluid. This condition may lead to severe complications, including brain damage, if left untreated (21).
Hence, early diagnosis is important to prevent complications like hearing loss and the need for more aggressive treatments.
How To Prevent Ear Infections In A Baby?
Certain measures of prevention may help minimize the risks for ear infections in babies (9).
- Vaccinate: The 13-valent pneumococcal conjugate vaccine (PCV13) protects against the attack of 13 types of bacterial infections. The less prone they are to such infections, the less their chances of having a secondary ear infection.
- Avoid allergens: Keep the baby away from allergens and irritants, such as pollen, pet dander, tobacco smoke, and automobile exhaust. Avoid taking your baby to public places where smoking is a common activity.
- Breastfeed: Breast milk contains antibodies that strengthen a baby’s immunity. Hence if you can nurse, prefer breast milk over formulas.
- Avoid ill people: Keep the baby away from family members and other individuals with symptoms of illness. If there is a disease spread in your area, request your family members to maintain distance and take the necessary precautions when around the baby.
- Change the feeding position: Bottle-feed your baby in an upright or semi-inclined position instead of placing them on their back and giving the bottle. It can prevent milk from reaching the middle ear through the Eustachian tubes.
- Wash hands frequently: Maintaining personal hygiene can protect the baby from communicable infections. Wash your hands with soap and warm water for 20 seconds frequently.
When To Call The Doctor For A Baby’s Ear Infection?
Consult your doctor if you notice the following signs in your baby (22).
- Symptoms persist beyond three days.
- Infection occurs frequently; neither the antibiotics nor the OTC medications seem to treat the infection.
- The baby is fussy and is expressing signs of severe pain.
- The ear infection is in a baby below six months of age.
- Pus discharge or bloody fluid secretion from the ears.
- A foul odor emanating from the baby’s ears.
- You notice symptoms such as loss of balance, impaired response, stiff neck, or fever.
Frequently Asked Questions
1. Can a baby have an ear infection without a fever?
An ear infection may or may not be accompanied by fever. Since fever is a common symptom of many childhood illnesses, it cannot be a dependable sign of an ear infection. Hence, look for other symptoms to distinguish an ear infection.
2. Can I put breast milk in my baby’s ear?
It is not safe to put breast milk into a baby’s ears. The accumulation of milk in the Eustachian tubes may increase the risk of an ear infection.
3. Can I smell an ear infection in a baby?
An ear infection leads to the release of pus, which may often have a foul odor due to the presence of microorganisms in it.
4. Can teething cause an ear infection?
Usually, teething may not cause ear infections in babies. To support this fact, a group study on breastfeeding mothers revealed that teething should not be deemed a causative factor of ear infections in babies. Further, babies who experience ear pain or infection should be evaluated promptly (23).
5. Can baths cause ear infections in babies?
Although you may be concerned about water accidently entering your baby’s ear while bathing, it usually comes out as a clear discharge and does not cause ear infections. Nevertheless, the NHS recommends preventing the entry of water or shampoo into your baby’s ear while bathing to reduce the risks of outer ear infections (24).
6. Can sippy cups cause ear infections?
Reports suggest that prolonged use of bottles or drinking of water or milk from sippy cups and using pacifiers may pose a risk of ear infection in babies and children (25) (27).
7. What are some alternative treatments for ear infections?
Using a cool-mist humidifier can help reduce congestion and promote comfort. Over-the-counter saline nasal drops can help clear nasal passages, potentially alleviating pressure and supporting drainage. For young children, gentle sinus rinses or nasal suction devices can help remove mucus and reduce infection-related discomfort. Parents of children over one year old might consider giving honey mixed in warm water to soothe associated symptoms, and positioning older children with an extra pillow can improve sleep comfort (28).
Ear infections in babies are common, but their signs may often go unnoticed. Since this condition resolves on its own, a wait-and-see approach is suggested for three days. If the symptoms persist even after that, it is safe to go to a doctor. However, if you’ve noticed severe signs like pus discharge, fever, distorted hearing, or altered behavior, take them to a doctor for further evaluation.
Infographic: Factors That Increase Chances Of Baby’s Ear Infections
Ear infections often tend to be common among babies and toddlers. Certain conditions and lifestyle choices tend to increase the chances of ear infections in infants. Staying aware of these factors can help you mitigate the risk of ear infections in babies, helping avoid other potential complications.
Some thing wrong with infographic shortcode. please verify shortcode syntax Some thing wrong with illustration image shortcode. please verify shortcode syntax
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Baker Bree | 19 + 20 months.https://themasseyspot.blogspot.com/2017/03/baker-bree-19-20-months.html
References
- Ear Infection (middle ear).
https://www.mayoclinic.org/diseases-conditions/ear-infections/symptoms-causes/syc-20351616 - Ear Infection Basics.
https://www.cdc.gov/ear-infection/about/?CDC_AAref_Val=https://www.cdc.gov/antibiotic-use/ear-infection.html - Acute Otitis Media.
https://www.ncbi.nlm.nih.gov/books/NBK470332/ - Chronic Suppurative Otitis Media.
https://www.aafp.org/pubs/afp/issues/2013/1115/p694.html - Ear Infections In Children.
https://www.nidcd.nih.gov/health/ear-infections-children#5 - Ear Infection.
https://familydoctor.org/condition/ear-infection/ - Sinusitis.
https://intermountainhealthcare.org/services/ear-nose-throat - Bottle Propping.
https://intermountainhealthcare.org/ckr-ext/Dcmnt?ncid=520407540 - Ear Infection In Babies And Toddlers.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/ear-infections-in-babies-and-toddlers - Cause Of Eustachian Tube Constriction During Swallowing In Patients With Otitis Media With Effusion.
https://pubmed.ncbi.nlm.nih.gov/8800060/ - Ear Infection Symptoms.
https://www.healthychildren.org/English/health-issues/conditions/ear-nose-throat/Pages/Ear-Infection-Symptoms.aspx - Ear – Discharge.
https://www.seattlechildrens.org/conditions/a-z/ear-discharge/ - How to Spot the Signs of an Ear Infection in Baby.
https://entandallergyspecialists.org/balance-testing/pediatric-balance-disorders/ - Pediatric Balance Disorders.
https://www.unitypoint.org/news-and-articles/how-to-spot-the-signs-of-an-ear-infection-in-baby - Lena Hafrén et.al; (2012); Genetic background and the risk of otitis media.
https://www.sciencedirect.com/science/article/abs/pii/S0165587611004769 - Ear Infection (Otitis Media).
https://my.clevelandclinic.org/health/diseases/8613-ear-infection-otitis-media#diagnosis-and-tests - Aspirin And Baby’s.
https://www.nationwidechildrens.org/family-resources-education/health-wellness-and-safety-resources/helping-hands/aspirin - Complications Of Ear Infections.
https://www.mottchildren.org/health-library/hw182912 - Cholesteatoma.
https://www.enthealth.org/conditions/cholesteatoma/ - Mastoiditis In Children.
https://www.stanfordchildrens.org/en/topic/default?id=mastoiditis-in-children-90-P02048 - Meningitis In Children.
https://www.stanfordchildrens.org/en/topic/default?id=meningitis-in-children-90-P02528 - Ear Infections: When To Treat At Home And When To Call A Doctor.
https://www.osfhealthcare.org/blog/ear-infections-when-to-treat-at-home-and-when-to-call-a-doctor/ - Opeodu Olanrewaju Ige and Popoola Bamidele Olubukola; (2013); Teething myths among nursing mothers in a Nigerian community.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3687861/ - Ear infections.
https://www.nhs.uk/conditions/ear-infections/ - Ear infection – acute
https://medlineplus.gov/ency/article/000638.htm - Ear Infection Questions.
https://www.seattlechildrens.org/conditions/a-z/ear-infection-questions/ - Hadara L. Norowitz et al.; (2019); Association between otitis media infection and failed hearing screenings in children
https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0212777#pone-0212777-g004 - Ear Infections: Treatment Without Antibiotics.
https://giving.massgeneral.org/stories/treating-ear-infections-without-antibiotics
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Anuradha Bansal
Read full bio of Sindusha MS
Read full bio of Dr. Ritika Shah
Read full bio of Ghazia Shah
















