Image: ShutterStock
Pregnancy brings a lot of changes to your life. While some changes are immediately noticeable, others aren’t. On the other hand, some changes, such as blood in stool during pregnancy, may alarm you. While the condition may cause severe concern, it is usually not a serious problem unless the amount is significant or it occurs frequently.

Blood spots in the stool may often be normal for many pregnant women as the pregnancy advances. Nevertheless, do not hesitate to take your doctor’s opinion about the condition to ensure proper and timely prenatal care.
Understanding why blood might appear in stool during pregnancy is important, as it can affect both their health and their baby’s well-being. Read this post to learn more about blood in the stool in pregnant women, what it signifies, and why it happens.
Key Pointers
- Bloody stool in pregnant women can be due to constipation, hemorrhoids, anal fissures, Crohn’s disease, polyps, and cancer.
- Symptoms associated with bloody stool are pain during passing stool, along with dark, black, and sticky stool.
- Treatment options include increasing fiber intake, drinking more water and fluids, using stool bulking agents, topical creams, and prescription medications.
- Prenatal vitamins containing iron in the form of ferrous gluconate can help prevent constipation and the risk of bloody stools.
- Although the condition is not always serious, medical attention is needed when women experience diarrhea, intense pain or bleeding during pregnancy.
Causes Of Blood In Stool During Pregnancy
Here are some causes for blood in your stool during pregnancy:
1. Constipation

The movement of food and then stool through the intestines slows in response to pregnancy hormones. As a result, many women experience constipation while they are pregnant. It could either be mild constipation or a very severe case where passing stool becomes a painful experience.
To make sure that your bowel movements are regular and smooth, try to have a minimum of eight to ten glasses of water in a day, include ample fiber from fruit and veggies, and ensure the iron in your prenatal vitamin is “non-constipating.” Prenatal vitamins containing iron in the ferrous sulfate form are less well tolerated, associated with more nausea, and can cause constipation. Finding a prenatal vitamin with iron as ferrous gluconate can prevent constipation and the risk of bloody stools from it.
If you are constipated, it could lead to further issues that could cause blood in your stool:
A. Hemorrhoids
During pregnancy, there is increased blood flow to your pelvis and all the structures down there, including your rectum and anus. Congestion of these blood vessels as the baby grows and compresses internal organs can cause them to become engorged – swollen called hemorrhoids. According to the National Institutes of Health (NIH) Estimates of hemorrhoid disease in pregnant women vary, but range as high as 35%.
- Constipation causes you to strain while passing stool. Straining can cause hemorrhoids to tear and bleed. This is when you may notice blood in your stool. The condition of passing stools mixed with blood is also called hematochezia
- If your bleeding is because of hemorrhoids, your doctor will ask you to increase your fiber intake and also ask you to drink more water and fluids. Your doctor may give you a stool bulking agentiMedications or supplements that make the stools bulky and easier to pass that will help soften your stool and reduce your need to strain while passing bowel movements.
- A doctor can also prescribe cold compresses to the area, various topical creams, and even wipes to alleviate pain and burning from hemorrhoids.
Paulene Nistal, a mother of two from Canada, had a hemorrhoid flare-up during pregnancy, which caused rectal bleeding. Narrating her experience, she says, “I used to have hemorrhoids before pregnancy, but it didn’t swell like it did in the past week. It smelled so bad and was so painful and uncomfortable. The worst was that it was bleeding. I asked the doctor if there was an option for me to drain the hemorrhoids. But he advised me not to undergo such treatment although that’s an option after giving birth (i).”
 Quick fact
Quick factB. Anal fissures
- An anal fissure is a tear in the mucosal lining of the anus, just inside the bum. It occurs secondary to straining from constipation or passing large, firm stools.
- Anal fissures or tears cause bright red bleeding and are also extremely painful.
- To help ease your pain and discomfort from the anal fissures, your doctor may suggest warm sitz (salt water) baths and also increase the amount of fiber you include in your daily diet. If it does not work, your doctor may recommend you try a stool bulking agent. Also, there are various ointments, such as Nifedipine and Nitroglycerin, which can help soothe the affected area and heal your fissures faster. Make sure that you use them only after you have checked with your doctor. Most anal fissures resolve after delivery.
C. Anal tears
- Anal tears happen only if you have anal fissures. As you remain constipated, you strain harder to pass stool, and it puts a high amount of pressure on your anal fissures.
- As a result, the anal fissures become bigger and can lead to tears in your rectum area. Due to the same, you can notice blood in your stool.
- Most treatments for anal tears are similar to the treatment for anal fissure.
D. Fistula
- A fistula is like a channel from your rectum area to the skin around your anus. In most cases, it helps to discharge a whitish substance, but sometimes, it can also cause bleeding.
- A fistula is often a problem in that particular area, and your doctor will be able to treat it locally. However, sometimes a fistula can also be the cause of a severe type of inflammation in some part of your intestinal tract, and the condition is known as Crohn’s disease.
- To treat a fistula, your doctor may prescribe some antibiotics that will be safe to be taken while you are pregnant. Otherwise, if that is not an option, your doctor can also prescribe certain medications that will help to take care of Crohn’s disease. In rare cases, if a fistula does not get treated with medication, the doctors may suggest a surgery. However, your doctor will ask you to wait till after the birth and only then have the surgery.
2. Polyps and cancer
- Polyps are small growths of the inside lining of the colon or rectum that protrude into it. They are more common with increasing weight, smoking, and age. There can be various types, most small and usually benign. They may cause bleeding seen as darker red blood or cause stool to be black and smelly.
- Larger polyps carry an increased risk of becoming cancerous.
3. Crohn’s disease, ulcerative colitis, and proctitis
- These are diseases that some women may have been diagnosed with before pregnancy. They all can cause intermittent inflammation of various parts of the digestive tract.
- These conditions can “flare up” during pregnancy causing bleeding.
- Thankfully they usually do not have any adverse effects on the pregnancy itself and women can progress to a healthy safe delivery.
Symptoms Associated With Bloody Stool During Pregnancy

Other symptoms that can be associated with bloody stool in pregnancy are:
- Pain when passing stool
- Dark, black and sticky stools
- Symptoms of anemia such as dizziness, feeling light-headed, fatigue or even fainting
When Should You Tell Your Doctor About Blood In Stool During Pregnancy?
Blood in the stool is quite common while you are pregnant. If the bleeding is minimal, a few drops at a time – it is probably not something you need to be worried about. However you should keep your obstetrician updated about any changes you notice while you are pregnant.
- You are unsure where the bleeding is coming from – your back passage vs. vaginal bleeding. Suppose you have been bleeding and have not experienced any discomfort or pain while passing stools.
- If you have abdominal or back pain, or nausea associated with bleeding.
- If you experience heavy bleeding, instead of just seeing a few red spots in your stool
- If you feel excessive pain or bloating in your stomach, you have also spotted blood in the stool. If you experience weight loss during your pregnancy. Call your doctor if you have a fever, in addition to spotting blood in your stool.
- If you feel that you are losing control over your bowel movements, you may sometimes notice the involuntary passing of stool, even while not in the washroom. If this happens, make sure to tell your doctor about it.
- If you are suffering from diarrhea for more than three days, or if the diarrhea is severe.
- If you have been suffering from gastrointestinal infections or problems.
- If you notice changes in your stool color, such as your stool becoming darker or black in color.
- Another condition in which you need to inform your doctor immediately is if you cannot pass stool for a few days at a stretch. It means that your constipation is severe, leading to other health issues.
 Point to consider
Point to considerHealth Concerns Of The Gastrointestinal Tract While You Are Pregnant

When you are pregnant, there are several anatomical and physiological changes that happen in your gastrointestinal tract. During pregnancy, your doctor will investigate and treat any issues , so that both you and your unborn baby remain safe and healthy.
- The many changes that happen in your gastrointestinal tract during the months of pregnancy can also lead to symptoms such as nausea, bloating, constipation, gastroesophageal refluxiCondition where stomach acids move back into the food pipe, leading to gastric discomfort and heartburn and more.
- In some cases, you may also be suffering from Crohn’s disease, which can make treatment rather tricky.
- It can also get extremely challenging for the doctors to diagnose and start treatment at the earliest, as there are a lot of medical restrictions they will have to follow while you are pregnant. In the case of patients who are not pregnant, the doctors can make use of various tools such as radiologic proceduresiImaging techniques such as CT, ultrasound, and MRI that help evaluate the body’s internal organs as well as a host of medicines that can help to heal the condition faster. However, when you experience the same during your months of pregnancy, the doctors will try to avoid the same as much as possible, as it could lead to health issues in the unborn baby.
- To make sure that you do not suffer from severe constipation or any of the other health issues that could lead to blood in the stool while you are pregnant, doctors advise that you take precautionary measures instead of waiting for treatment (1).
Alleviating Blood In Stool During Pregnancy

The first thing you should do when you feel discomfort due to the blood in your stool is to inform your doctor. Once your doctor has spoken to you, here are a few things you can do at home that will put you at ease, even if you continue to spot the blood:
- Clean up properly after you have been to the washroom. Make sure that you clean your rectal area each time after you pass stool.
- Be gentle when you wipe yourself or dry the area, so that you do not cause further damage to the hemorrhoids or fissures that you may have. Instead of rubbing the rectal area dry, pat it gently.
- If you feel you are in too much pain and discomfort, and if it interferes with your passing stool, ask your doctor if there are any pain medications that you can safely take while you are pregnant.
- If you still feel pain and discomfort, ask your doctor to suggest some creams or ointments that will help to heal the skin around your rectal area. There are also some medicated creams that will numb your rectal area so that you will experience less pain while you pass stool.
- Wear clothes that are loose fitting, especially lowers, so that they will not scrape or stretch the skin that is already sore from the fissures or tears.
- Increase the amount of water you drink throughout the day. If you do not want to drink too much water, you can also include a lot of different types of fluids, such as fresh juices, soups, stews, shakes and such in your everyday meal plan. When you are pregnant, your body uses a lot more water, so it is more important to make sure that you are properly hydrated.
- Increase the amount of fiber you have in your everyday meals, as the roughage will help your stool to become soft and prevent constipation. Most cereals contain a good amount of fiber. Also, one of the richest sources of fiber is bran.
- Make sure to include some amount of exercise and activity in your daily lifestyle. Check with your doctor what all exercises you can do or how much activity is good for you.
- Try to pass the stool after you have had meals, as your colon activity will be at its highest when you have had a meal. It will put less stress on your colon and result in less blood in the stool.
- If you are not able to include exercise in your daily routine, you can speak to your doctor about a fiber mix you can create at home with the doctor’s approval. Take four to six tablespoons full of bran and mix it with a bulk forming agent, such as Psyllium, Polycarbophil or Methylcellulose. Have the mix with one or two glasses of warm water. The mix will help to increase the water content in your body as well as reduce the amount of time it takes for your stool to pass through the colon. Speak to your doctor about the measurements and such before you take it.
- Some probiotic formulaiFood products containing gut-friendly microorganisms can also reduce the pressure you experience while passing stool that often causes blood in the stool. The supplements will help to change the flora that is present in the colon and may cause an improvement in your bowel function. Probiotics are considered very safe and hence are suggested when you are pregnant. However, make sure you speak to your doctor first and only then go for it.
Foods To Ease Constipation

Here are a few foods you can include in your everyday diet to reduce constipation. Before you do so, make sure to check with your doctor first:
- Garbanzo beans
- Kidney beans
- Black eyed peas
- Kiwi
- Sweet potatoes
- Almonds
- Pecans
- Pumpkin seeds
- Pears
 Quick tip
Quick tipFrequently Asked Questions
1. What tests are done to diagnose blood in stool during pregnancy?
A physical examination of the rectum and anus and a fecal occult blood test may be performed to identify the underlying cause of blood in stools. Your doctor may suggest a colonoscopy if necessary (5).
2. Can stress cause blood in stool during pregnancy?
Stress is not a common cause of blood in stool during pregnancy. However, chronic psychological stress may aggravate inflammatory conditions such as ulcerative colitis (6). This, in turn, may cause rectal bleeding.
3. Can infections cause blood in stool during pregnancy?
Yes, infections such as infective diarrhea may cause blood in stools during pregnancy (7). Diarrhea during pregnancy can be concerning, so it’s essential to seek medical advice if this occurs.
4. Can alcohol consumption cause blood in stool during pregnancy?
A study shows that alcohol intake may aggravate hemorrhoids, leading to blood in stool during pregnancy (8). In fact, alcohol consumption is contraindicated during pregnancy due to the risk of fetal alcohol spectrum disorders (9).
5. Can miscarriage happen through stool?
Gynecologist & obstetrician Dr. Nisarg Patel says, “In most cases, miscarriage results in spontaneous abortion but can also occur through vaginal bleeding or cramping. While there are rare cases where tissue from a miscarried fetus may be passed through stool, it is not considered a common way for the miscarriage to manifest itself.”
Blood in stool during pregnancy isn’t uncommon and is usually not a cause of concern. Constipation, leading to hemorrhoids and anal fissures, Crohn’s disease, and ulcerative ulcerative colitisiInflammation and ulceration of the large intestine, including the rectum are some of the issues that can cause some blood to pass in stools. Consult a doctor if you don’t know where the blood is coming from or have additional issues, such as excessive pain or bloating in the tummy. Cleaning your rectal area thoroughly every time after passing stool, staying optimally hydrated, and eating a fiber-rich diet are a few ways to alleviate blood in stools during pregnancy.
Infographic: What Happens When Blood In Stool During Pregnancy Is Left Untreated?
Rectal bleeding or blood in stool during pregnancy requires immediate management to prevent discomfort and complications. Some conditions may resolve without medications, while others may require medical care. Go through the infographic to know the possible complications of untreated rectal bleeding in pregnancy. Illustration: Momjunction Design Team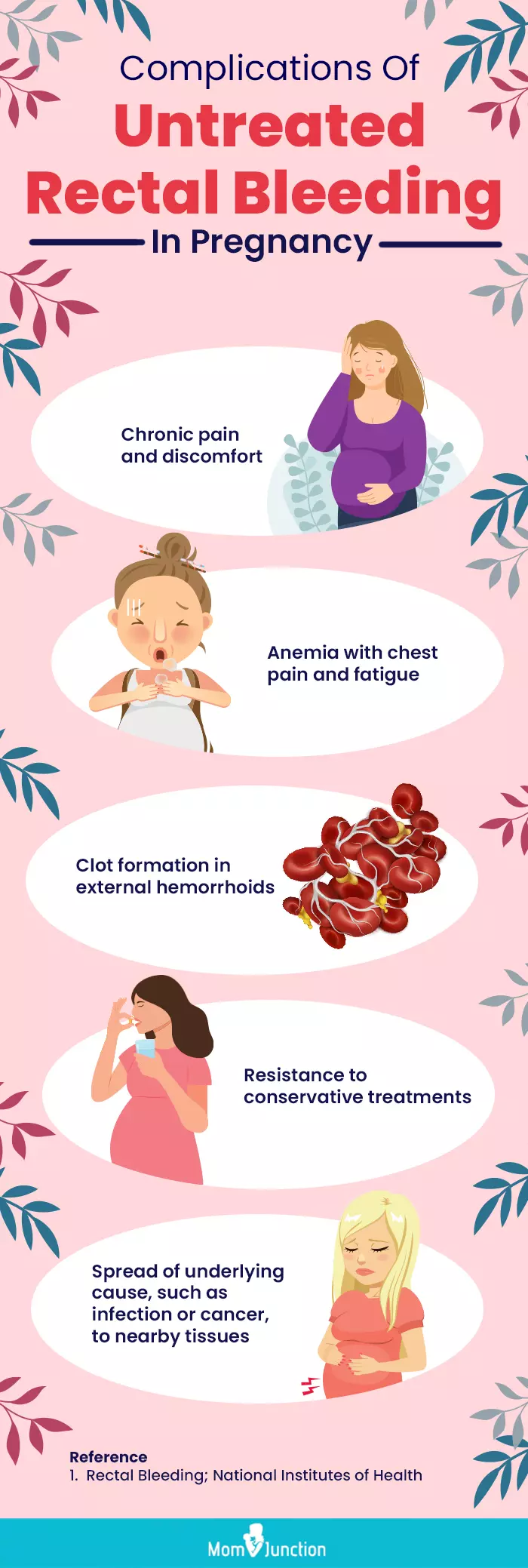
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Brought to the ER for my pregnancy hemorrhoids and 32-week ultrasound │Paulene Nistal.https://www.youtube.com/watch?feature=shared&v=GNfJ8pbM6fw
References
- Sherri A. Longo et al.; (2010); Gastrointestinal Conditions during Pregnancy.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2967327/ - Piles in pregnancy
https://www.nhs.uk/pregnancy/related-conditions/common-symptoms/piles/ - L Story et al.; (2025); Lower gastrointestinal bleeding in pregnancy: Differential diagnosis assessment and management
https://journals.sagepub.com/doi/full/10.1177/1753495X20948300 - An Essential Guide on What to Eat During Pregnancy
https://www.fhcsd.org/prenatal-care/what-to-eat-during-pregnancy/#:~:text=Your%20prenatal%20nutrition%20must%20includefor%20your%20baby%27s%20physical%20development - Rectal Bleeding.
https://my.clevelandclinic.org/health/symptoms/14612-rectal-bleeding - Joel E Mawdsley et al.; (2006); The effect of acute psychologic stress on systemic and rectal mucosal measures of inflammation in ulcerative colitis.
https://pubmed.ncbi.nlm.nih.gov/16890594/ - L Story et al.; (2025); Lower gastrointestinal bleeding in pregnancy: Differential diagnosis assessment and management.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8504301/ - François Pigot et al.; (2005); Risk factors associated with hemorrhoidal symptoms in specialized consultation.
https://pubmed.ncbi.nlm.nih.gov/16518286/ - About Fetal Alcohol Spectrum Disorders (FASDs)
https://www.cdc.gov/fasd/about/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/fasd/facts.html#
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Ben Abbes Taarji Hicham
- Dr. Nisarg Patel is a gynecologist, obstetrician, and laparoscopic surgeon from Ahmedabad, India, with over 13 years of experience in the field. He did his post graduation in Obstetrics and Gynecology from Pravara Institute of Medical Sciences, Ahmednagar, and holds a fellowship of Reproductive Medicine.
 Dr. Nisarg Patel is a gynecologist, obstetrician, and laparoscopic surgeon from Ahmedabad, India, with over 13 years of experience in the field. He did his post graduation in Obstetrics and Gynecology from Pravara Institute of Medical Sciences, Ahmednagar, and holds a fellowship of Reproductive Medicine.
Dr. Nisarg Patel is a gynecologist, obstetrician, and laparoscopic surgeon from Ahmedabad, India, with over 13 years of experience in the field. He did his post graduation in Obstetrics and Gynecology from Pravara Institute of Medical Sciences, Ahmednagar, and holds a fellowship of Reproductive Medicine.
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das