Image: ShutterStock
The presence of blood in a child’s stool can be a worrisome sight for the parents. But you should note that blood passing with stool does not always indicate any serious internal complications or disease (1). Most health practitioners have reported that it is a common occurrence in children and requires minimal to no treatment. However, if this condition is accompanied by pain and other symptoms, contact the doctor immediately. Read on to learn more about the causes, treatment, remedies, and prevention of blood in a child’s stool.

Read on to know more about the causes, treatment, remedies, and prevention of blood in a child’s stool.
Key Pointers
- The presence of blood in a child’s stool does not always indicate a severe underlying condition.
- Some food items, such as beets or iron supplements, might give a bloody appearance to a child’s stool.
- Other common reasons include anal fissures, intestinal obstruction, or hemorrhoids.
- Giving children a diet high in fiber and laxatives and helping them maintain personal hygiene can help them deal with bloody stools.
- If stool in the blood is accompanied by signs of severe abdominal pain and weakness, consult a doctor immediately.
Is It Really Blood In Your Child’s Stool?
It’s important to determine whether the red coloration in your child’s stool is due to blood or other factors. Often, the consumption of certain foods or medicines may give the child’s stool a bloody appearance (2)(3). Such foods include:
- Chocolate
- Flavored gelatin
- Kool-Aid or similar beverages
- Beets
- Tomatoes
- Red licorice
- Iron supplements
- Antibiotics (ampicillin, amoxicillin)
- Bismuth preparations (Pepto-Bismol)
Signs Of Bloody Stool In Children
Depending on the cause and source, the appearance of blood (color and intensity) in the stool may vary. It can range from bright red to tarry black (4)(5)(6).
- The presence of bright red blood in the stool is known as hematochezia. This may be because of the bleeding in the colon or rectum (lower gastrointestinal tract).
- Maroon-colored stool may indicate bleeding in the middle gastrointestinal tract.
- The appearance of dark tarry stools, also known as melena, may indicate bleeding in the upper gastrointestinal tractiThe organs through which food and liquids pass to be ingested, broken down, absorbed, and eliminated as feces or esophagus, stomach, and duodenumiThe first section of the small intestine connected to the stomach and aids in completing the digestion of food .
Causes of Bloody Stool in Children
Age is an important factor in identifying the cause of rectal bleeding in children and adolescents. Some of the common causes in children (2-12 years old) and adolescents (12-18 years old) include the following.
1. Anal fissure
It is a tear or a break in the skin of the anus. One of the most common causes of rectal bleeding in children, this usually occurs due to hard stool or constipation. Sometimes, cases of explosive diarrhea may also result in such tears. Eating a diet low in fiber can also increase the risk.
You may notice streaks of blood in your child’s stool or on the toilet paper. These fissures can also cause pain and discomfort during a bowel movement (7). The Children’s Hospital of Orange County (CHOC) states, the tear usually heals within six weeks with simple care. Often, the fissure gets better once the constipation is treated (8).
2. Juvenile polyp
Juvenile polypsiIrregular tissue development in the bowel's lining are the most common types of intestinal polyps that occur in children aged between three and ten years. They are characterized by bleeding and abdominal pain (9). A study examined the occurrence of polyps in children. The scientific report states, “In a large review series of 563 children aged from 2 months to 17 years, the highest incidence of polyps was between ages 2 and 10 years (85.1%). Rectal bleeding was the presenting symptom in 78.5% of cases (10).”
3. Infectious colitis (infection)
Bacterial, viral, or parasitic infections can cause bloody stool (usually with diarrhea) in any age group. Common pathogens include Salmonella, Shigella, Campylobacter, Yersinia enterocolitica, Clostridium difficile, and Escherichia coli (11). Entamoeba histolytica is a common water-borne parasite that can cause bloody diarrhea.
 Be watchful
Be watchful4. Inflammatory bowel disease (IBD)
Inflammatory bowel disease consists of two conditions (12).
- Crohn’s disease: It can occur in any part of the gastrointestinal (GI) tract – from the mouth to the anus.
A mother of two, Amber Hixson, recalls her story of dealing with her son’s early diagnosis of Crohn’s disease. She says, “My 7-year-old son, Braxton, went to the bathroom, and there was bright red blood in his stool. I reached out to a GI doctor whom I trusted and liked for advice. He suggested just watching it for now and seeing how things went.
A month later, they were out shopping when the episode recurred. Hixson shares, “We were all the way in the back of the store, and I remember looking at Braxton’s face, which had a panicked look that said, ‘I have to go now!’ My husband took off with him in search of the bathroom. Not long after, I started receiving pictures from my husband of what looked like pure snot laced with bright red blood. I knew it wasn’t good. I sent the pictures to the GI doctor again, and we immediately got an appointment that week. After the initial exam, the doctor said he wanted to scope Braxton and that he expected to find polyps. Nevertheless, upon scanning, he told us that he didn’t find any polyps but that he believed Braxton had Colitis. The biopsies would tell us if it was Ulcerative Colitis or Crohn’s Disease. A week or so later, our doctor called and gave me the heartbreaking news that Braxton had Crohn’s Disease (i).”
- Ulcerative colitis: It occurs in the large intestine (colon) or rectum.
It is characterized by chronic inflammation of the GI tract. Some of the common symptoms may include abdominal pain, rectal bleeding, weight loss, fatigue, and diarrhea. Most cases are diagnosed after 15 years of age (13).
5. Solitary rectal ulcer
Although rare in children, it is characterized by bloody stools, constipation, mucus discharge, abdominal pain, and prolonged straining. It is often misdiagnosed or may remain undiagnosed (14).
6. Intestinal obstruction (intussusception)
Intussusception is a common cause of intestinal obstruction in children up to three years of age. It can also occur in older children and teenagers. According to the National Institutes of Health (NIH), approximately 2000 infants in the US experience intussusception during their first year of life, and boys are more prone to intussusception than girls, with a ratio of roughly 3:1 (15). Intussusception is generally characterized by severe abdominal pain, bloody stools, red currant jelly-like stools, fever, extreme fatigue, vomiting, diarrhea, and a swollen abdomen (16).
7. Henoch-Schonlein purpura
This syndrome, also known as IgA vasculitis, affects children in the age group of 3 to 15 years. It is characterized by purple spots on the skin, joint pain, gastrointestinal problems (sometimes bloody stools), and kidney disorders (17).
8. Hemolytic-uremic syndrome
Most common in children, this condition generally occurs after E. Coli infection in the GI tract. Children may experience vomiting, diarrhea, fever, lethargy, bloody stools, and fatigue (18).
9. Hemorrhoids (Piles)
Hemorrhoids are veins around the anus that become swollen because of extensive stretching under pressure. Piles can occur due to prolonged straining during a bowel movement, chronic constipation, or diarrhea. Symptoms of hemorrhoids in children may include pain and swelling around the anus, itching, or bright red blood in the stool (19).
10. Upper gastrointestinal hemorrhage
In younger children, upper gastrointestinal bleeding can sometimes result in the passage of bright red blood in the stool (hematochezia) (20). This may be due to relatively faster intestinal transit time as compared to that of adults.
Besides the above commonly known causes of bloody stool in children, other reasons may include colorectal cancer, Meckel’s diverticulum (a bulge in the small intestine), milk protein intolerance or allergic colitis, and thrombocytopenia (resulting from low platelets) (21)(22)(23)(24).
Diarrhea And Blood In A Child’s Stool
Bloody diarrhea or blood in your child’s stool followed by diarrhea is not common. It could occur due to an underlying condition, such as (25):
- Inflammatory bowel disease (ulcerative colitis & Crohn’s disease)
- Intestinal infection caused by bacteria, virus, or parasite
- Juvenile polyp (not so common)
- Intussusception (not so common)
Mucus And Blood In A Child’s Stool
The presence of mucus and blood in the child’s stool can be caused due to the following conditions (14)(26).
- Inflammatory bowel disease (ulcerative colitis & Crohn’s disease)
- Solitary rectal ulcer
- Infection (Clostridium difficile or amoebic infection)
Diagnosing the Cause of Blood In Stool
Healthcare practitioners may consider the medical history, age of the child, and physical examination to narrow down the causes of rectal bleeding. Physical examination of the anus and perineumiThe slender skin membrane that lies between the genitalia and anus may be performed to identify any signs of fissures or fistulas (27)(28).
The doctor may also recommend further tests for your child.
- Colonoscopy, the most preferred diagnostic technique for rectal bleeding.
- Stool evaluation and culture (e.g., Wright stain) for fecal occult blood testing
- Complete blood count
- Ultrasound of the abdomen
- Ultrasonography
- CT scan or MRI
- Abdominal radiography or X-ray
If necessary, the doctor will suggest a treatment plan based on the underlying cause. Along with that, you could try a few home remedies to minimize the risk of bloody stools. You may use these for mild cases of bloody stool.
Home Remedies to Relieve Symptoms
These simple tips and dietary changes may help your child get some relief from the painful or bloody rectum (29).
- Warm sitz baths: These baths involve sitting in warm, shallow waters to relieve symptoms of fissures, hemorrhoids, and other conditions. Soaking of the bottom or perineum area (around the anus) can soothe pain, itching, irritation, etc. Doctors may sometimes recommend adding medications or soothing agents such as salt, baking soda, or vinegar for better relief.
- High-fiber diet: To relieve constipation symptoms in your child, healthcare practitioners may recommend switching to a high-fiber diet. Including whole fruits (banana, pears, berries, etc.), vegetables (broccoli, green peas, etc.), and whole grains (oatmeal, whole-grain bread, or pasta) can help.
- Plenty of water: Encourage your child to drink water at regular intervals, especially if they have constipation. Staying hydrated can help loosen stool.
- Personal hygiene: Teach and help your child to maintain hygiene in the perineal area (around the anus). Make sure that they wash gently, clean, and pat dry the area after bowel movements.
- Physical activity: Physical activity, including playtimes and age-appropriate exercises, are important in maintaining healthy bowel function in your child.
 Quick tip
Quick tipWhen You Should See A Pediatrician
If you have concerns such as ‘What should I do if my child has blood in his stool repeatedly?’ You should visit a pediatrician to identify the cause of blood in your child’s stool. A proper diagnosis can help manage underlying conditions or rule out any serious problem. Consider taking medical advice if your child experiences the following (3).
- Severe fatigue or weakness
- Bloody diarrhea
- Dark tarry stools
- Abdominal pain
- Abdominal swelling or distention
- Urine that has pink or tea color
- Vomiting blood
Treatment Of Bloody Stool In Children
The line of treatment for rectal bleeding can depend on the underlying cause (27).
1. Stool softeners or laxatives: In most cases, fissures are caused because of the passing of hard stool or chronic constipation. Therefore, doctors often recommend stool softeners or laxatives.
2. Topical ointments: In severe cases of fissures or tears because of constipation, stool withholding, or painful bowel movement, doctors may recommend topical analgesic ointments to help reduce pain. Do not use over-the-counter creams or ointments in children without consulting your healthcare practitioner.
 Experts say
Experts say3. Antibiotics: Antimicrobials or antiparasitic medicines can be prescribed in the case of infectious colitis or intestinal infections. Treatment is based on the identified bacteria, virus, or parasite.
4. Immunosuppressive and anti-inflammatory agents: Such medications may be recommended by your doctor to manage inflammatory bowel disease (ulcerative colitis). Corticosteroids, aminosalicylates, immunomodulators, etc., are effectively used in children to eliminate symptoms and improve the quality of life.
5. Endoscopic treatment/therapy: Full colonoscopy with endoscopic polypectomy may be used to treat polyps. Juvenile polyps are usually small (around 5-15mm in diameter), and, therefore, doctors may recommend a snare polypectomy, which uses heat, to cut the polyps.
6. Surgery: Surgery may be an option in children with bleeding due to intestinal obstruction (intussusception), rectal polyp or any vascular anomaly.
Frequently Asked Questions
1. Should I take my child to the ER for blood in stool?
You need not take your child to the emergency room if only traces or a few drops of blood appear in their stools. However, it is required if your child has passed a lot of blood with stools or has passed only blood without stools (30).
2. Why is my child pooping blood with no pain?
If your child develops internal hemorrhoids, there may be blood in the stools but no pain (31).
3. Can dehydration cause blood in stool?
Dehydration may be a cause of constipation. If left untreated, constipation may cause anal fissures or hemorrhoids resulting in bloody stools (32).
Blood in a child’s stool can appear in several ways, including bright red streaks or clots mixed with the stool. It may also make the stool appear dark or tarry black, called melena. Bright red blood usually indicates bleeding lower in the colon or rectum. Dark red blood points to bleeding higher up in the digestive tract, likely the small intestine or stomach. Black, tarry stool suggests an upper GI bleed like a stomach ulcer. The color and consistency of blood in stool help identify where bleeding is occurring so doctors can better pinpoint and treat the cause. Seeking prompt medical attention for bloody stools is crucial, as bleeding can sometimes be severe (34).
5. How should I support my child emotionally if they have blood in their stool?
Reassure your child that they are safe and encourage them to talk about how they feel. They may be scared or worried about their symptoms, so it’s important to be understanding and supportive.
There could be several medical reasons for blood in a child’s stool. In most cases, minor spotting or infrequent bloody stools are easily treatable with medical interventions and homecare measures. The causes include common conditions, such as hemorrhoids, and long-term problems, such as inflammatory bowel disease. Although rectal bleeding in children is not uncommon, you must still contact a doctor if the bleeding is persistent, increases in frequency, and is accompanied by other symptoms such as pain and fatigue. Furthermore, timely evaluation and prompt treatment help prevent serious consequences.
Infographic: What Are Advanced Diagnostic Tests For Blood In Stool In Children?
Doctors may do regular physical examinations and order basic diagnostic tests in the initial stage of diagnosing blood in the stool. However, more advanced tests are recommended if they cannot establish a diagnosis with the given symptoms and obtained results. Go through the infographic to learn advanced diagnostic tests used for determining the causes of blood in stools or gastrointestinal bleeding. Illustration: Momjunction Design Team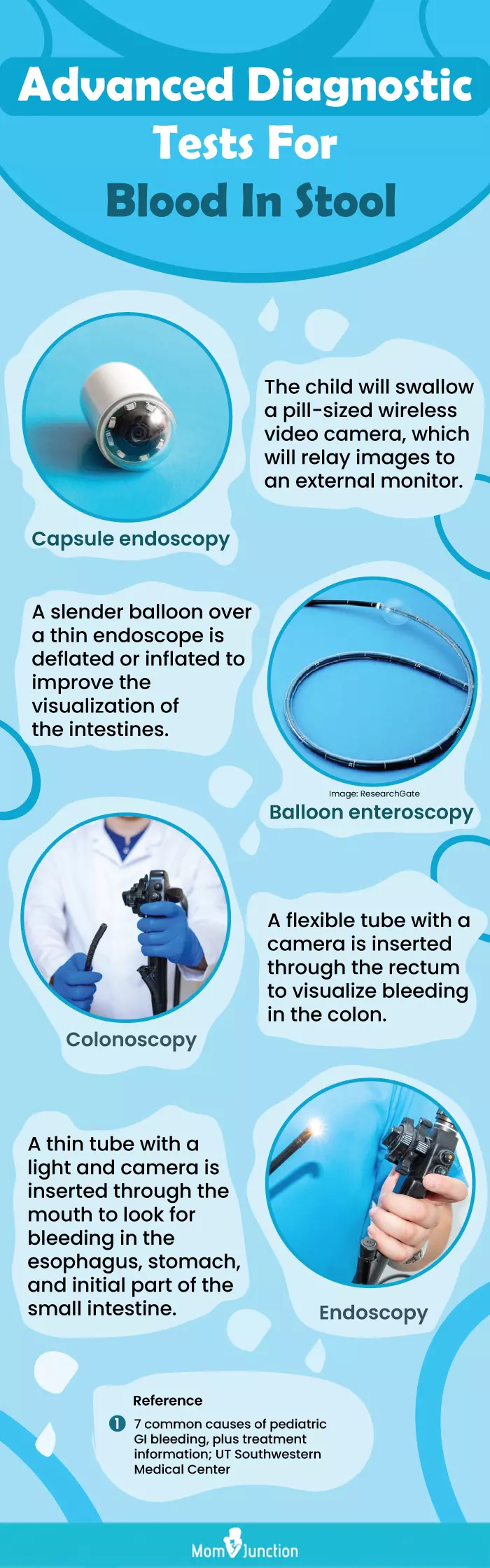
Illustration: What Causes Blood In Child&039s Stool And Its Treatment

Image: Stable Diffusion/MomJunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Living with Crohn’s: I thought I was watching my son die — Part 1.https://medium.com/@cfrei/living-with-crohns-i-thought-i-was-watching-my-son-die-2d3a3754a40
References:
- Blood in the Stool.
https://www.rwjbh.org/treatment-care/pediatrics/conditions-treatments/pediatric-gastroenterology/blood-in-the-stool/ - Red Stools in Children: Common Causes.
https://www.healthychildren.org/English/health-issues/conditions/abdominal/Pages/red-stools-in-children-common-causes.aspx - Stools – Blood In.
https://www.childrenscolorado.org/conditions-and-advice/conditions-and-symptoms/symptoms/stools-blood-in/#:~:text=The%20things%20listed%20below%20can,such%20as%20amoxicillin%20or%20omnicef) - R Bhanu Pillai and Vasundhara Tolia; (2008); Gastrointestinal bleeding in infants and children.
https://www.proquest.com/openview/cd6f0796f65c2611761908d722da0ee1/1?pq-origsite=gscholar&cbl=54584 - Marisa Piccirillo et.al; (2025); Gastrointestinal bleeding in children: diagnostic approach.
https://ijponline.biomedcentral.com/articles/10.1186/s13052-024-01592-2 - What Can Your Child’s Poop Color Tell You?
https://www.hopkinsmedicine.org/health/conditions-and-diseases/stool-color-guide - Anal Fissure.
https://fascrs.org/patients/diseases-and-conditions/a-z/anal-fissure - Anal Fissures.
https://choc.org/programs-services/gastroenterology/constipation/anal-fissures/ - Vincent R Adolph and Kathryn Bernabe; (2008); Polyps in Children.
https://pmc.ncbi.nlm.nih.gov/articles/PMC2780254/ - Konstantinos H Katsanos et.al; (2011); Juvenile polyp presenting with rectal bleeding in a 2-year-old girl.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3959461/#:~:text=Rectal%20polyps%20in%20children%20are,presenting%20symptom%20in%2078.5%25%20cases. - Infectious Colitis.
https://www.ncbi.nlm.nih.gov/books/NBK544325/ - Inflammatory Bowel Disease.
https://www.ncbi.nlm.nih.gov/books/NBK470312/ - The Facts About Inflammatory Bowel Diseases.
https://www.crohnscolitisfoundation.org/sites/default/files/2019-02/Updated%20IBD%20Factbook.pdf - Nafiye Urgancı et.al; (2013); Solitary Rectal Ulcer Syndrome in Children: A Report of Six Cases.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3848538/ - Child Intussusception.
https://www.ncbi.nlm.nih.gov/books/NBK431078/ - Intussusception in Children.
https://www.stanfordchildrens.org/en/topic/default?id=intussusception-in-children-90-P02002 - IgA vasculitis – Henoch-Schonlein purpura.
https://medlineplus.gov/ency/article/000425.htm - Hemolytic-uremic syndrome.
https://medlineplus.gov/ency/article/000510.htm - Hemorrhoids.
https://choc.org/programs-services/gastroenterology/hemorrhoids/ - Upper Gastrointestinal Bleeding.
https://www.ncbi.nlm.nih.gov/books/NBK470300/#:~:text=Upper%20gastrointestinal%20bleeding%20describes%20blood,to%20the%20ligament%20of%20Treitz. - Farah Mushtaq et.al; (2014); Rectal bleeding in children – causes and investigations.
https://www.sciencedirect.com/science/article/abs/pii/S175172221400198X - Thrombocytopenia.
https://www.healthdirect.gov.au/thrombocytopenia - What is allergic colitis?
https://www.childrenshospital.org/conditions/allergic-colitis - Colon Cancer Symptoms.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/colon-cancer/colon-cancer-symptoms - M Stephen Murphy; (2008); Management of bloody diarrhoea in children in primary care.
https://pmc.ncbi.nlm.nih.gov/articles/PMC2364807/ - Investigation of rectal bleeding.
https://pmc.ncbi.nlm.nih.gov/articles/PMC1792853/pdf/archdisch00652-0007.pdf - Makbule Eren and Hasan Özen; (2011); Gastrointestinal bleeding in children.
https://dergipark.org.tr/en/download/article-file/178895 - Gastrointestinal Bleeding or Blood in the Stool.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/gastrointestinal-bleeding-or-blood-in-the-stool - Treatment-Anal fissure.
https://www.nhs.uk/conditions/anal-fissure/treatment/ - Stools – Blood.
https://www.stlouischildrens.org/health-resources/symptom-checker/stools-blood - Hemorrhoids and what to do about them.
https://www.health.harvard.edu/diseases-and-conditions/hemorrhoids_and_what_to_do_about_them - Constipation.
https://my.clevelandclinic.org/health/diseases/4059-constipation - Peptic ulcer.
https://www.mountsinai.org/health-library/diseases-conditions/peptic-ulcer - Rectal Bleeding.
https://my.clevelandclinic.org/health/symptoms/14612-rectal-bleeding - Stools – Blood In.
https://www.seattlechildrens.org/conditions/a-z/stools-blood-in/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Saroj Kumar
Read full bio of Dr Bisny T. Joseph
Read full bio of Swati Patwal
Read full bio of Anindita Ghatak