image: Shutterstock
A burn is a skin or tissue injury resulting from overexposure to the sun, chemicals, heat, or electricity. It is one of the most common household injuries among children. Burns in children may range from minor injuries, such as sunburn, which can be managed with home care, to life-threatening injuries requiring emergency care. Children are at a greater risk of burn injuries due to their natural curiosity and exploratory behavior. Their skin is also softer and more sensitive than that of adults, making it more susceptible to burns.
Read this post to know more about the types, causes, symptoms, signs, complications, prevention, diagnosis, treatment, and home care for burns in children.
Key Pointers
- Thermal, chemical, and electrical burns are the common types that affect children.
- If not treated immediately, burns may cause complications such as scars, infections, or hypothermia.
- In case of electrical or chemical burns, contact your doctor immediately.
- Blocking your child’s access to fireplaces, keeping them away from kitchen stoves, and several other preventative measures as you read through.
Types Of Burns
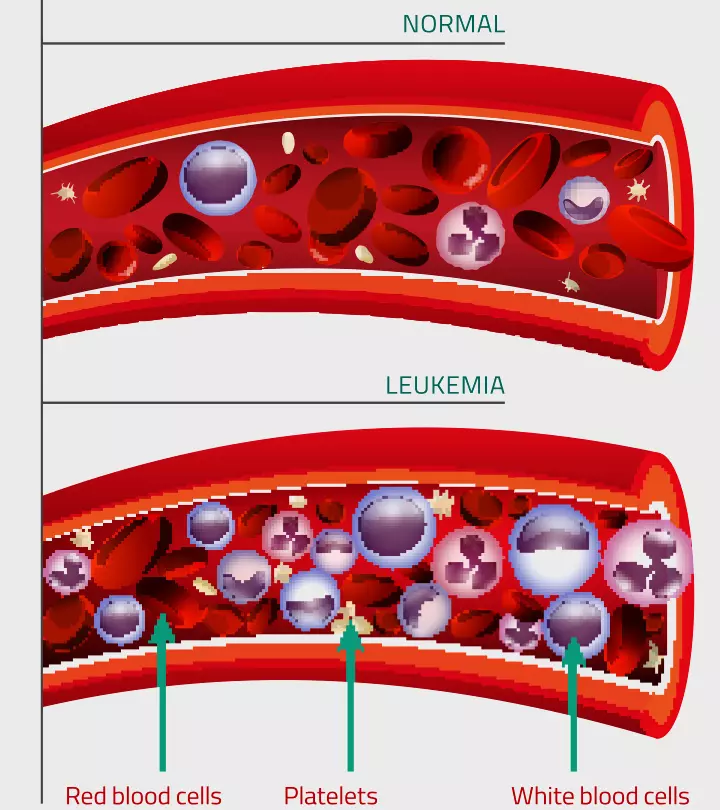
Burns are classified into various degrees depending on how severe and deeply it affects the skin (1).
- First-degree burns or superficial burns affect the outer skin layer (epidermis). Mild sunburn is an example of first-degree burns. This may not cause permanent damage to the skin other than changes in skin color.

Image: Shutterstock
- Second-degree burns or partial-thickness burns involve the epidermis (outer layer of the skin) and the dermis (the layer of skin beneath the outer layer). Second-degree burns may cause swelling and blisters.
- Third-degree burns or full-thickness burns affect the outer and inner layers of the skin and reach the tissue beneath it (subcutaneous tissue). This affected area may appear black or white.
- Fourth-degree burns or full-thickness burns involve the skin layers, subcutaneous tissue, and deeper layers of tissue. They may also involve the muscles and bones. The affected child may experience loss of sensation in the affected area as the nerve endings are destroyed.
Common Causes Of Burns
Understanding the causes of burns may help you protect your child from burn injuries. The following are some common causes of burns (2).
- Thermal burns: Hot liquid spills, hot bath water, steam, flame, hot surfaces, fire, etc., can cause thermal burns.

Image: Shutterstock
- Chemical burns: Accidental spilling or swallowing of chemicals can cause burns to the skin, eyes, or digestive tract. Strong acids such as button batteries, paint thinners, gasoline, drain cleaners, and bleach are common causes of chemical burns in children.
- Radiation burns: Burns may occur in children if the skin is exposed to ultraviolet rays for a prolonged period. Radiation burns may also happen from X-rays.
- Electrical burns: Touching electrical cords, putting fingers in electrical outlets, etc., are common causes of electrical burns in children.
Some children may have burns due to child abuse. Burns from cigarettes, hot metals, hot water (scald burn), chemicals, etc., on different body areas are often a result of abuse.
Signs And Symptoms Of Burns
The signs and symptoms of burns may vary depending on the degree of burn. In severe cases, it may take one or two days for the signs and symptoms to develop (3) (4).
- First-degree burns: Pain and redness on the skin are common symptoms of first-degree burns. The skin may appear dry without blisters, and the outer layer of the skin may peel off in one or two days. The burn injury heals within three to six days in most children.
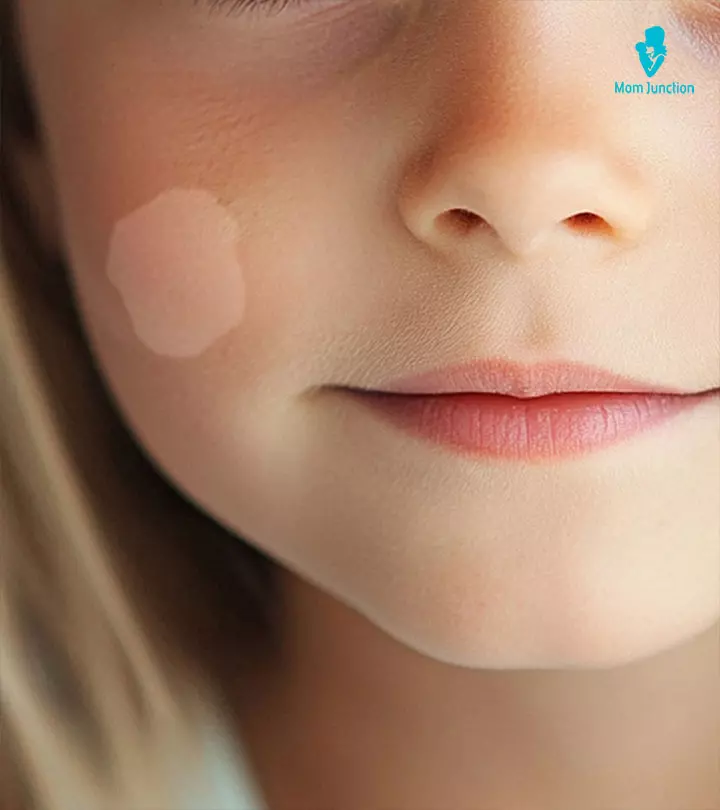
- Second-degree burns: Severe pain, swelling, redness, blotchy skin (white patches on the skin), and blister formation are seen in second-degree burns. The burn site may look wet, pink, or cherry red after the blisters are broken. Healing time may vary based on severity, with the average time being three weeks. Deep second-degree burns may lead to scarring in some children.
- Third-degree burns: Leathery appearance of the skin is a characteristic feature of third-degree burns. The burn site may look charred, blackened, brown, or white since it affects the tissues beneath the skin. Children may complain about numbness if the nerves are damaged.

Image: Shutterstock
Healing time may depend on the severity and could range between three to six weeks. Children may require plastic reconstruction or skin grafts to regain the appearance and function of the affected area.
- Fourth-degree burns: You may see deep burns, and these may involve the muscles and bones. Children may not feel pain since the nerves are damaged.
Full-thickness burns (third and fourth-degree burns) are more severe since they involve all layers of skin and deep tissues. Prompt medical care may help improve outcomes in full-thickness burns.
Complications Of Burns
The following complications are commonly seen in children after burn injuries (5).
- Bacterial infections and sepsis (bloodstream infection)
- Hypothermia (low body temperature)
- Scars and ridges on the skin
- Keloids (overgrown scar tissues)

Image: Shutterstock
- Breathing issues due to the intake of smoke, toxic gases, or hot air
- Hypovolemia (low blood volume) due to fluid loss
- Contractures of muscles and joints due to scar tissue tightening or shortening of the muscle tendons and skin
- Toxic shock syndrome (TSS), which includes symptoms such as fever, rash, shock, diarrhea, vomiting, and irritability.
When To See A Doctor?
You may consult a pediatrician if your child has a burn injury. They will help them assess the severity and degree of burn and prescribe the right treatment to heal the skin. Seek emergency medical care for burns in the following situations.
- Burns covering more area of the body
- Breathing troubles
- Airway burning
- Burns on the face, feet, hands, and over a major joint
- Deep burns
- Leathery skin
- Skin discoloration such as white or blackened skin
- Electrical and chemical burns
Administer first aid for burn accidents while the emergency help arrives. If you are unaware of first aid, you may immediately call emergency services for guidance.
Contact the child’s pediatrician while or after treatment if you notice
- Blister or burn that does not heal within two weeks.
- New symptoms.
- Extensive scarring.
- Signs of wound infection such as pain, swelling, redness, and oozing of pus or fluid.
 Be watchful
Be watchfulDiagnosis Of Burns
The pediatrician may assess the severity of the burn by examining the skin. Burns covering more than ten percent of the body area and deep burns on the groin, face, or feet are referred to burn centers for more specialized care.
Doctors may order the following tests in burn injuries.
- Lab analysis
- Chest X-ray
- Upper endoscopyi A process in which the doctor inserts a flexible tube with a camera inside the body to view the esophagus, stomach, and duodenum.
- ElectrocardiogramiA test that assesses the rhythm and electrical activity of the heart. (ECG)
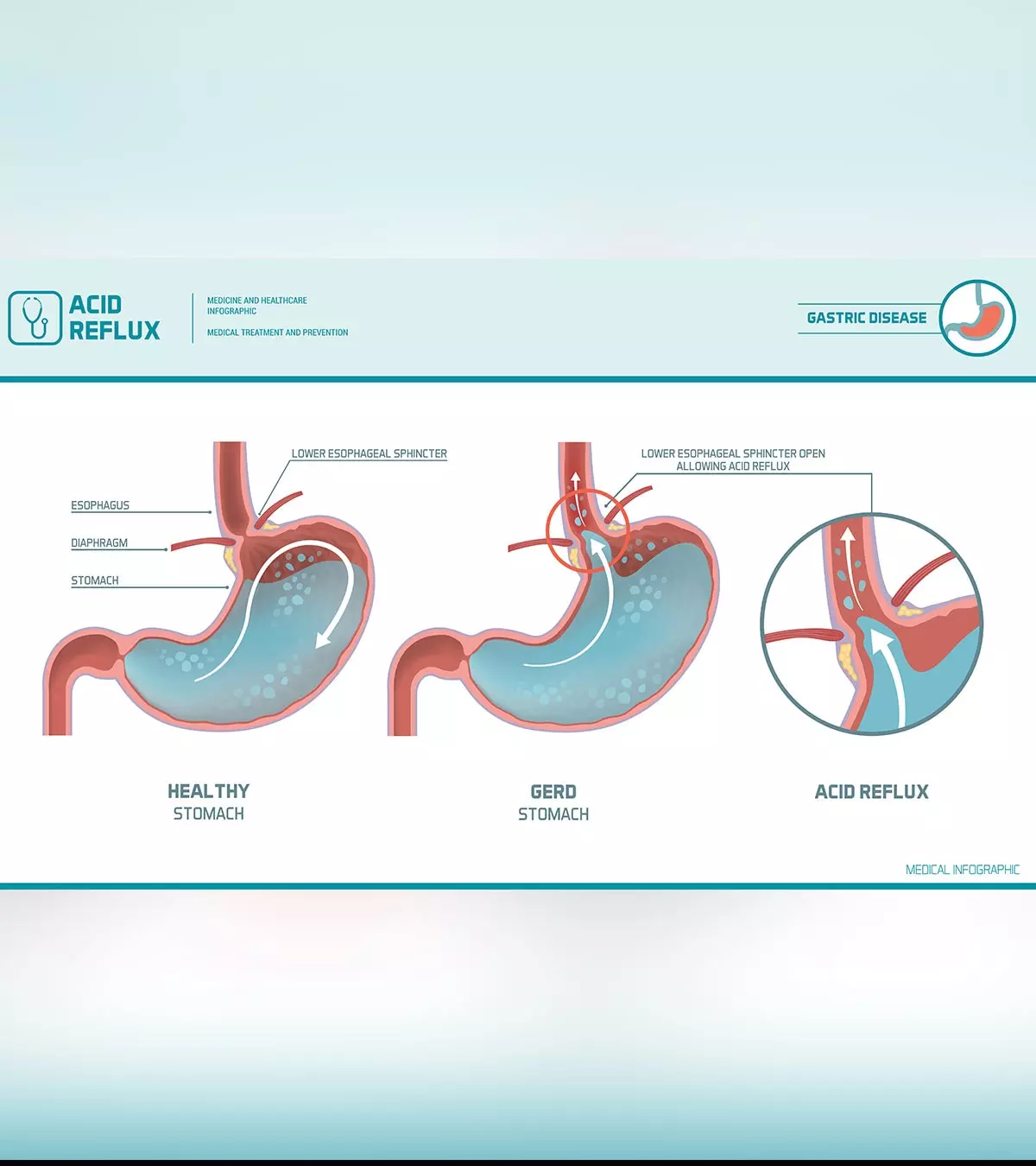
Treatment For Burns
Treatment options for burns may vary depending on the type of burn and the aim of the treatment, such as reducing pain, preventing infection, reducing scarring, removing dead tissue, and regaining the normal function of the burned area.
Minor burns can be treated at home, and they may heal within a few weeks. Severe burns may require hospitalization and treatment at specialized burn centers. After first aid, medical treatment for burns is given to enhance healing. This may include the following (5).
1. Wound dressing is done according to the type and severity of the burn. The doctor may cover the wound in dry gauze if the child is referred to a burn center.
2. IntravenousiTo administer medicines, fluids, or nutrients in the body through a needle or tube inserted into the veins. (IV) fluids are often prescribed to prevent dehydration and organ dysfunctions.

Image: Shutterstock
3. Intravenous (IV) antibiotics are given if there are signs of infection on the burn site.
4. Topical medications such as burn ointments and creams are prescribed for wound healing and recovery. Bacitracin and silvadene (silver sulfadiazine) are common topical medications prescribed to prevent infection.
5. Water-based treatments, such as ultrasound mist therapy, may be used to stimulate and clean the burned tissue.
6. A tetanus shot is prescribed for some cases after the burn injury.
7. Pain medications are often required to control the pain caused by burns. Morphine is a preferred drug to manage severe burn pain, primarily during wound dressing changes.
8. Anxiety medications are often prescribed for some children with increased anxiety or fear due to the injury.
One or more of the following surgical and other procedures are sometimes required in children with severe burns (5):
- Breathing assistance is needed for children with burned neck, throat, and face or swelling of the throat. A tube is inserted into the trachea (windpipe) to supply oxygen to the lungs.
- Feeding tubes are required to provide nutrition to children with severe burns.
- Skin graft, a surgical procedure that replaces the deep burn scars with healthy skin from other parts of the body or donors, may be required.
- Plastic reconstruction or surgery may help increase joint flexibility and improve skin appearance.
- Removal of eschar (burn scab) is done to ease the blood flow around the wound. An eschar may cause breathing trouble if the skin on the chest wall is tightened. If left untreated, it may cut off blood circulation in the skin and delay healing.
Doctors may also recommend physical and occupational therapy to children with severe burns or trauma, especially those that involve the joints. Physical therapy exercises may help with rehabilitation, stretch the skin, and keep the joints flexible, while occupational therapyiTherapeutic activities to help people manage physical, emotional, mental, or cognitive problems. may help your child perform their daily activities. Some older children with large burns, especially on the face and other visible areas, may require psychological therapy to cope with emotional issues (6).
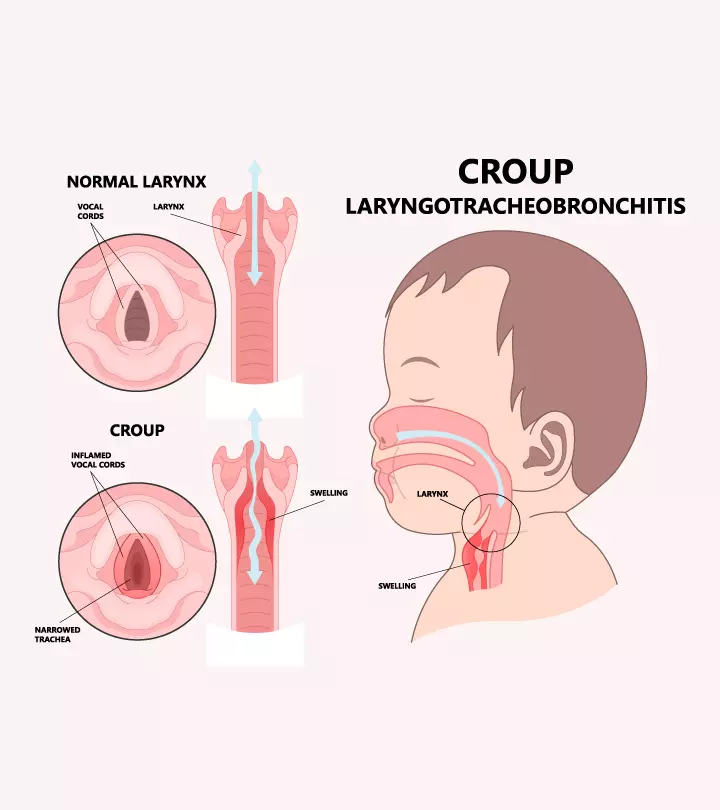
Home Remedies For Burns
Although minor burns can be treated with home care measures, it is recommended to seek advice from a pediatrician. You may give the following first aids if the child has a burn injury (5).
- Cool the burn area by pouring cool (not very cold) water. Do not apply ice since this may cause more damage to the tissue.
- Remove jewelry, if any, on the burn area before the tissue swells.
- Do not break fluid-filled blisters since this may cause infections. You may clean the area with water and mild soap if the blister breaks by itself. You may apply antibiotic ointment over the area.
- Apply lotions after the area cools down. You may apply moisturizers or lotions with aloe vera gel to prevent drying of the burn site. The gel should be free of additives. Apply it gently and do not rub it into the skin.
- Bandage the burn site with sterile gauze to protect the area. Wrap the gauze loosely around the wound to avoid pressure on the injury.
- Administer pain relievers such as acetaminophen (Tylenol) after consultation with the pediatrician.
- Get an up-to-date tetanus shot.
You may apply prescribed antibiotic cream or ointments over the burn area after the blister is broken. Discontinue the application and contact the doctor if you notice any rashes on the burn site. Moisturizers and sunscreens can be applied regularly after the burn injury is healed.
Prevention Of Burns In Children
The following tips may reduce household burn injuries in children (5) (7).
- Do not hold or carry a child while cooking on the stove.
- Never leave cooking items unattended on the stove.
- Keep hot liquids and food items out of your child’s reach.
- Turn the pot handle toward the rear of the stove.
- Keep electrical appliances away from water.
- Do not heat feeding bottles in the microwave.
- Always check the temperature of food or liquid before serving it to the child.
- Do not use dining table mats and clothes that the child can pull from below.
- Block the child’s access to fireplaces, stoves, outdoor grills, and other heat sources.
- Unplug the iron and other devices when not in use and keep them away from the reach of children.
- Keep electrical wires and codes out of the child’s reach since younger children may chew on them.
- Cover unused electrical outlets with safety caps.
- Check for hot buckles and straps on the car seat before placing a child.
- Do not smoke indoors or while sitting on the bed.
- Check the smoke detectors periodically and change the batteries on time.
- Keep fire extinguishers on every floor of the house.
- Keep lighters and matches away from children.
- Keep chemicals out of children’s reach.
- Test bath water temperature before placing the child in it.
- Do not let children play near sparklers or fireworks.
- Keep burning candles out of children’s reach.
- Keep space heaters at least three meters away from the bed, and do not leave them on when you are sleeping.
- Use cool mist vaporizers instead of hot steams.
- Do not leave the child unattended at home while heat and electric devices are in use.
- Educate children about fire safety, including the dangers of flames and hot surfaces.
 Quick tip
Quick tipFrequently Asked Questions
1. Why are burns in children more serious?
Burns in children are more serious than in adults since (8)
- A child’s skin is thinner than an adult’s and takes less time and energy to burn.
- Young children have a larger surface area to body mass ratio and are at a higher risk of hypothermia during the initial cooling of the burn and increased evaporative loss.
- They have a higher risk of damage to the airways.
- Children have a larger blood volume per unit of body weight. So during fluid replacement, small children may become hypoglycemic (low glucose) if the maintenance fluids do not incorporate glucose replacement.
- Children have stronger systemic inflammatory responses than adults, resulting in increased severity of a hypermetabolic state (more energy expenditure occurring due to inflammatory responses after burns).
2. What should I put on my child’s burns?
Mepilex Ag® silver dressing, Silvadene Cream 1%® burn cream, Xeroform® Bismuth Tribromophenate gauze dressing, Bacitracin® topical antibiotic ointment, and Aquaphor® moisturizer healing ointment may be used at home on children after a healthcare professional has assessed and treated the burn (9).
3. Should I cover a burn or let it breathe?
Covering the burn with a dry bandage helps to keep it clean. As first aid, you may use cling film as well. Discard the first few inches of film from the roll and then use it to cover the burn area (12).
4. How do I know if a burn is healing?
The skin on the burn area could be of a different color. However, if the area is dry, it shows that the burn area is healing (13).
Burns in children may occur due to exposure to heat, chemicals, or electricity. Fireworks can also cause burns in children. Therefore, sharing about chemical, electrical, fire, and fireworks safety for kids is essential. There are four degrees of burns depending on the severity and depth of tissue damage. The percentage of the body affected is also considered for prognosis. Pediatricians examine burn injuries in detail since they can be accidental or indicate child abuse. First-degree burns may cause redness and pain and resolve with basic care measures. In contrast, burns involving deep tissue damage can affect physical functioning depending on the area affected and often require reconstructive plastic surgeries.
Infographic: How To Manage Burns In Children At Home?
If your child has sustained a minor burn injury, it can be treated at home. However, even in the case of severe burn injury, you must know to give first aid to the child until they are sent to the hospital. The infographic below provides certain useful first aid measures you can use to attend burn injuries.

Illustration: Momjunction Design Team
Illustration: Burns In Children: Treatment And Home Remedies

Image: Dalle E/MomJunction Design Team
References
1. Classification of Burns;University of Rochester Medical Center
2. Burns;Children’s National Hospital
3. Taking Care of Burns;American Academy of Family Physicians
4. Burn Stages;Stanford Health Care
5. Burns;St. Clair Health
6. Understanding a Burn Injury;Model Systems Knowledge Translation Center
7. Burn Treatment & Prevention Tips for Families;American Academy of Pediatrics
8. Burns; The Royal children’s Hospital, Melbourne
9. Caring for Your Child’s Burn After Treatment; Children’s National Hospital
10. Burns in Children; Johns Hopkins Medicine
11. Burn Prevention: Preschool and School Age; Nationwide Children’s
12. Jackie Hudspith and Sukh Rayatt; First aid and treatment of minor burns; NAtional Library of Medicine; (2004)
13. The right way to treat burns; UW Health
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Dur Afshar Agha
Read full bio of Dr Bisny T. Joseph
Read full bio of Dr. Ritika Shah
Read full bio of Vidya Tadapatri