Image: ShutterStock
It is common for a pregnant woman to hear more about the benefits and risks of a C-section vs. normal delivery when her due date is approaching. She may have many concerns about which procedure would be the best for her and the little one. Knowing how and why the procedures are done can help her anticipate what will happen and reduce anxiety and fear.
Vaginal delivery is recommended if there are no indications for C-section delivery. Maintaining a healthy lifestyle from the time you conceive may increase your chances of vaginal delivery. However, you may have to choose the delivery method suggested by your doctor based on obstetric indications. If your doctor determines that vaginal delivery is unsafe due to certain specifications or complications of your pregnancy, a C-section may be recommended.
Read on to know more about the benefits and risks of a C-section compared to normal delivery.
Key Pointers
- Vaginal delivery or normal delivery is the recommended method for giving birth and carries fewer risks than a c-section.
- Vaginal delivery offers benefits such as faster recovery time and beneficial bacteria for the baby, but there are risks associated with painful contractions and bleeding.
- Cesarean delivery, or c-section, is a surgical procedure performed when vaginal delivery is not safe, involving an incision through the abdomen and uterus of the mother.
- Benefits of c-section include a shorter delivery process, less pressure on the vagina, lower risk of infection, less trauma for the baby, and safety with abnormalities, although complications are possible.
- Planning and maintaining a healthy lifestyle can help prevent the need for a c-section delivery.
Vaginal Delivery
The most common option for delivery, vaginal delivery is known to have fewer risks than a c-section. According to the WHO, 70% to 80% of pregnant women who enter into labor are at low risk and can probably deliver vaginally. That’s perhaps why vaginal delivery is often called normal delivery (1). It is also considered as the natural birth procedure because the labor starts on its own, signifying that the baby is ready to come into the world.
That said, not all normal deliveries may be safe. There may be certain limitations along with the advantages too, which we talk about next.
What Are The Benefits Of Vaginal Delivery?
For the mother
- Mother and baby interaction: Women have expressed higher satisfaction, improved interaction with the baby, and control over the delivery in the case of vaginal delivery (2).
- Breastfeeding: Vaginal delivery also aids better maternal breastfeeding success through breast milk maturation. Skin-to-skin contact during normal delivery also leads to better outcomes with regards to breastfeeding and infant crying (2).
- Faster recovery: The recovery time after delivery is shorter with vaginal delivery than with cesarean delivery. It takes just one or two days to recover after a normal delivery, and about two weeks to resume the daily activities (3) (4).
For the baby
- Baby gets beneficial bacteria: During vaginal birth, the baby goes through the birth canal. Here, it gets exposed to bacteria that are known to be beneficial for its immune health, brain, and digestive health. It even helps in preventing infections (5).
- Low risks of TTN: Just before birth, the baby’s lungs are filled with fluid. When the fluid remains even after the birth, the baby may develop a condition called transient tachypnea of the newborn (TTN). However, with vaginal delivery, the fluid is cleared out while the baby is passing through the birth canal. Hence, there is almost no risk (6).
If there are any complications during labor, vaginal delivery can also pose risks for maternal health and may also cause fetal distress.
What Are Possible Problems Associated With Vaginal Delivery?
For the mother
- Painful contractions: Uterine contractions are painful but once you get your bundle of joy, the pain seems worth it. Besides, judicious use of epidural analgesiaiAdministration of medication in the area around the spinal nerves to reduce pain or to numb the lower half of the body. and painkillers have made the journey almost pain free (7).
- Others: There could be risks such as pelvic floor disorders associated with vaginal deliveries, including urinary and fecal incontinenceiThe inability to control bowel movements. , and excessive bleeding (2) (8) (9). A meta-analysis study by multiple institutions revealed that the incidence of postpartum urinary incontinence is 27.9%, which is much higher than the other pelvic floor disorders in the case of vaginal delivery.
For the baby
Usually, vaginal delivery is safe for the baby. However, in rare cases (difficult birth, prolonged delivery, the baby is too large for gestational age), there could be risks of mild injuries that could be resolved a few weeks after the birth (10).
In case there are more risks than benefits related to vaginal delivery, the doctors suggest cesarean birth.
 Quick fact
Quick factC-Section Birth
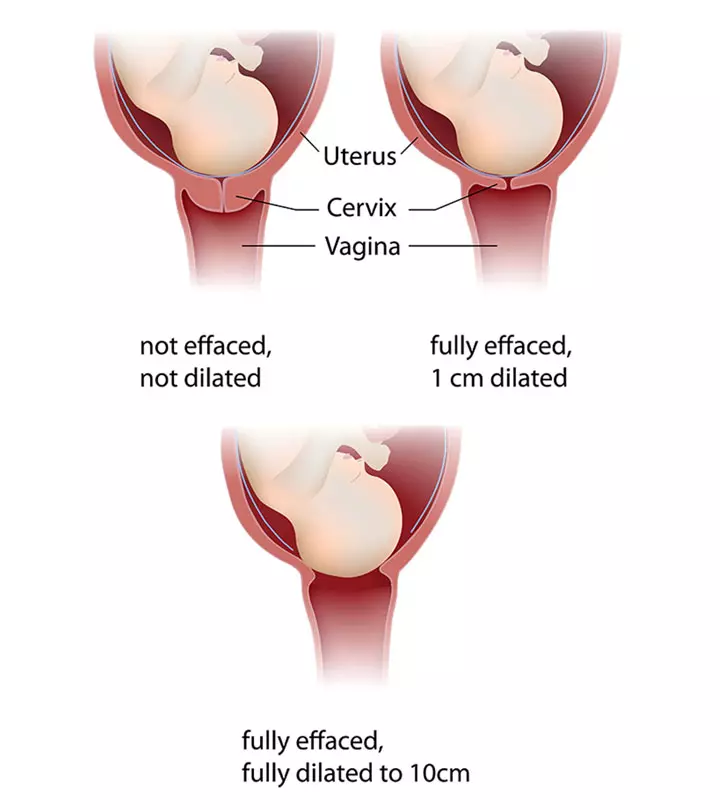
Cesarean or c-section delivery is a surgical procedure, wherein an incision is made through the abdomen and uterus of the mother. When vaginal delivery is not considered safe, the doctor’s have to go with this method of childbirth (10) (11).
Like vaginal birth, cesarean delivery also has its own advantages and disadvantages. More about it in the following section.
What Are The Benefits Of C-Section Delivery?
For the mother
1. Reduced time:
In recent years, the cesarean techniques have been simplified. The results are minimal loss of blood, shorter operating time, and higher patient satisfaction (12).
2. Reduced risk of incontinence: There is no stretching or tearing of the vaginal with cesarean surgery, so there is a lower risk of pelvic prolapseiA condition where pelvic floor muscles lose support and get pushed into the vaginal space. , anal and urinary incontinence (13).
3. Reduced risk of infection transmission: A few studies have found that there is no or reduced risk of transmission of hepatitis B virus or other infections to the infant with the elective cesarean procedure. This risk is high in the case of vaginal deliveries (14).
For the baby
- Reduced trauma: As the baby doesn’t have to pass through the birth canal during a c-section procedure, there is no stress or trauma to the baby. The baby is directly and safely taken out of the mother’s womb.
- Reduced or no injury: There are fewer or almost no risks of injury to the baby through a cesarean delivery.
- Safe delivery with abnormal conditions: Sometimes, the baby settles down in the mother’s womb in certain abnormal positions (such as transverse lie or breechiA position in which the babies’ feet or buttocks are positioned to come out of the vagina at first. ). Or the mom could have obstetric complications like placenta previa (placenta covering the cervix). In such situations, vaginal delivery could be risky, and a c-section would ensure your baby is safe (15).
What Are The Possible Problems Associated With C-Section Delivery?
For the Mother
- Anesthesia-related complications: Anesthesia given before the cesarean is not the actual reason for risks. The condition of the patient might contribute to complications after the administration of anesthesia (16).
- Surgery-related infections: Similar to other surgeries, cesarean surgery could result in surgical site risks such as endometritisiInfection and inflammation of the uterine lining. and wound infections (17). Also, according to a study, the maternal mortality rate was highest among women who underwent emergency cesarean delivery.
- Longer recovery time: Full recovery after c-section may take around six to eight weeks, during which time individuals may experience discomfort, fatigue, and limited mobility. The longer recovery period for c-sections is attributed to the fact that it is a surgical procedure involving an incision through the abdominal wall and uterus. It’s crucial for individuals recovering from a c-section to prioritize rest, follow medical advice, and gradually resume normal activities to ensure a smooth and complete recovery. Some studies suggest that around 60% of women still experience some discomfort at the incision site even 24 weeks after giving birth (18).. Those who undergo a c-section often may also find themselves spending a longer duration in the hospital compared to those who have a vaginal delivery.
- Other long term risks: There is a chance that vaginal delivery may not be possible in the next pregnancy and you may have to opt for c-section (19).
 Quick fact
Quick factFor the baby
- Breathing problems: With a c-section delivery, there is a risk of transient tachypnea of the newborn (TTN), which is the formation of fluid in the baby’s lungs, making it difficult to breathe (20).
- Emergency delivery due to conditions like umbilical cord entanglement have been linked to, adverse neonatal outcomes such as NICU admission, or may even lead to higher rates of perinatal mortality.
Ideally, you should discuss your pregnancy with your doctor and weigh the pros and cons of each method. If your pregnancy is progressing smoothly and the doctors see no risks, then vaginal delivery is recommended. If not, the doctor would suggest a cesarean.
While a c-section is safe, some expectant mothers would prefer a normal delivery. If you too want to avoid a c-section birth, continue reading and know what you can do about it.
How Can You Improve Your Chances ?
Planning and maintaining a healthy lifestyle right from the time you conceive can help you avoid a c-section birth. Here are some tips that you can follow for that.
- Have a proper birth plan by discussing your health conditions and preferences with your doctor. This would let you avoid many risks and help you proceed with normal and safe delivery.
- A lot of studies have shown that the support of a doula during your pregnancy and delivery will help you reduce the chances of c-section.
- Acquire knowledge of the procedures of childbirth. You can read books on birthing and take childbirth classes; this will help you deal with the fear before the delivery.
- Make sure you are eating healthily and engaging in exercises safely. Being active through your pregnancy will prepare your body for labor and normal delivery.
- Try to avoid induction of labor before 41 weeks, as that could increase the chances of a c-section. You should opt to induce labor only when the doctor says, which is generally to avoid medical complications. Try to be patient and relaxed even if everything doesn’t work out as planned and if the doctor says that a cesarean would be safe for you and your baby. After all, the health and safety of your baby and you is the priority.
In the next section, we have some common questions about normal delivery vs. cesarean answered for you.
Frequently Asked Questions
1. Can I choose the mode of delivery?
Yes, but it depends on several factors. For instance, you may wish to have a normal delivery, but doctors may suggest a c-section due to the baby’s position or other factors. In such cases, it is best to side with the doctor’s decision. On the other hand, if you want to have a cesarean due to the fear of pain or incontinence and the doctor says there are no risks with c-section in your case, then you can go for an elective cesarean.
Whatever procedure you choose, the goal should be the health and safety of both the mother and the baby.
2. Is normal delivery possible after c-section?
Yes, vaginal birth after cesarean (VBAC) is possible. According to a study, 75% of such cases are successful (21). However, it is essential that you talk about it with your doctor and then take a decision based on your health condition.
3. How many cesarean births are allowed?
Consecutive cesareans could increase the risk of placenta accreta, which means implantation of the placenta abnormally. The risk increases with every c-section, although it is 0.5% or less for the first three. But after four cesareans, the risk rises to 2%, and with six cesareans, the chances of placenta accreta increase to 6% (22). As the risks increase, labor supervision and management by an experienced medical professional become essential.
4. Upon having a C-section, when will my milk come?
C-sections may cause late milk production postpartum. One of the researchers found that in some women, milk production during the first five days was significantly lower than that in vaginal birth. However, studies also reveal that you may speed up this process by establishing more skin-to-skin contact with your baby(23).
5. Is it harder to breastfeed after a C-section?
Women undergoing C-sections seem to have a higher proportion of breastfeeding issues and delayed milk production(23).
Try to relax and go through the details again and talk to your doctor to clarify any doubts. The more relaxed you are, the smoother your pregnancy and labor will be. Stay healthy and maintain a healthy lifestyle to avoid any complications during delivery. And once the baby is in your arms, all fear and doubt will disappear. Perhaps then, you will also realize the strength of a woman who is a mother.
Infographic: Difference Between A Vaginal Delivery And A Cesarean Delivery
During the third trimester, your healthcare provider will decide on your delivery method, depending on the high-risk or low-risk pregnancy. However, know that both these methods have their pros and cons. Check out the infographic below to learn about the differences between these methods and what are their benefits.

Illustration: Momjunction Design Team
What were your delivery experiences? Do share them with us in the comment section below.
Illustration: C-Section Vs. Normal Delivery: How Are They Different

Image: Stable Diffusion/MomJunction Design Team
Having a baby is a life-changing experience. Learn the differences between a Caesarean and and vaginal birth to make an informed choice that aligns with your preferences.
References
1. I. Brunt; Normal Birth; The Permanente Journal (2005)
2. C. S. Buhimschi and I. A. Buhimschi; Advantages of Vaginal Delivery; Clinical Obstetrics and Gynecology (2006)
3. S. Liu et al.; Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term; Canadian Medical Association Journal (2007)
4. Vaginal Vs. Cesarean Delivery; Health Care University of Utah (2015)
5. Building Your Microbiome from Birth; American Museum of Natural History
6. Transient Tachypnea of the Newborn; NCBI
7. N. M. A. Beigi, K. Broumandfar, P. Bahardoran, and H. A. Abedi; Women’s experience of pain during childbirth; Iranian Journal of Nursing and Midwifery Research (2010)
8. J. S. Moldenhauer; Excessive Uterine Bleeding at Delivery (Postpartum Hemorrhage); MSD Manual
9. M. Solans-Domenech et al.; Urinal and anal incontinence during pregnancy and postpartum: incidence, severity, and risk factors; Obstetrics and gynecology (2010)
10. Vaginal Birth and Cesarean Birth: How Do the Risks Compare?; Childbirth Connection
11. M. P. Hehir et al.; Cesarean delivery in the United States 2005 through 2014: a population-based analysis using the Robson 10-Group Classification System; American journal of obstetrics and gynecology (2018)
12. Cesarean Delivery; Stanford Children’s Health
13. T. R. Vejnovic, S. D. Costa, and A. Ignatov; New Technique for Caesarean Section; Geburtshilfe and Frauenheikunde (2012)
14. A. Rosenman; Childbirth and Incontinence: Things You Should Know; Female Pelvic Medicine and Reconstructive Surgery
15. Y. Hu et al.; Effect of elective cesarean section on the risk of mother-to-child transmission of hepatitis B virus; BMC Pregnancy and Childbirth; (2012)
16. What Every Pregnant Woman Needs to Know About Cesarean Section; University of South Florida
17. Somrat Charulaxananan et al.; Anesthesia-related complications of caesarean delivery in Thailand: 16,697 cases from the Thai Anaesthesia Incidents Study; Journal of the Medical Association of Thailand; (2010)
18. Recovery following cesarean section; Caesarean Section; National Library of Medicine
19. C-Section Mothers; Stanford Medicine
20. Transient Tachypnea of the Newborn; Children’s Hospital of Philadelphia O. E. Keag; J. E. Norman, and S. J. Stock; Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis; PLOS Medicine (2018)
21. What is vaginal birth after cesarean (VBAC)?; Eunice Kennedy Shriver National Institute of Child Health and Human Development
22. D. Hernandez; You Asked: How many c-sections can a woman have?; Texas A&M University Health Science Center
23. Amy J. Hobbs et al.; The impact of caesarean section on breastfeeding initiation, duration and difficulties in the first four months postpartum; National Library of Medicine (2016)
24. Assisted Vaginal Delivery; The American College of Obstetricians and Gynecologists
25. Postpartum Hemorrhage; Stanford Medicine
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sangeeta Agrawal
Read full bio of Rebecca Malachi
Read full bio of Swati Patwal
Read full bio of Dr. Joyani Das