Image: ShutterStock

Chalazion in children is an uncommon ocular condition where a small, slow-developing lump resembling a stye appears on the eyelid; however, it is not the same. A stye is a painful lump on the eyelid resulting from a bacterial infection of the eyelash, while a chalazion is a painless bump caused by a blocked oil gland in the eyelid (1). If left untreated, a stye can turn into a chalazion and vice versa (2). Chalazia are usually harmless and self-limiting, requiring only minor medical attention. However, it may not dissolve in some instances and may develop into chronic issues. This post discusses the causes, diagnosis, and complications of chalazion and how it can be treated and prevented in children.
Key Pointers
- Chalazion, also known as a meibomian cyst, is a painless lump on the eyelid.
- Poor eyelid hygiene, hormonal changes, and various skin conditions and infections can influence chalazion formation in children.
- Warm compression and gentle massage over eyelids and some OTC medicines, ointments, and eye pads may effectively treat chalazion in children.
- If a chalazion obstructs your child’s vision, consult an ophthalmologist for surgical drainage of chalazion.
Why Does Chalazion Occur In Children?
Small oil glands called meibomian glands within the eyelids’ margins secrete oil to lubricate the eye surface and prevent it from drying out. When one or more of these glands get blocked, oil begins to build up inside them. It leads to the formation of a chalazion, a lump visible on the eyelid. It is why chalazion is also known as a meibomian cystiA red, fluid-filled inflamed lump on the eyelid. .
A chalazion is painless, but if left untreated, the oil build-up can rupture the gland, leading to swollen eyelids in children. It is red and the swelling causes concern to the child and parents. Upon rupture, the leaked oil can irritate the eye and the eyelid, making the eye red, swollen, and painful (3).
What Are The Risk Factors For Chalazion In Children?
Children with a history of chalazion or stye are at risk of its recurrence. The following factors could also influence the formation of a chalazion in children (4) (5) (6).
- Eyelid hygiene and care: Studies show that the collection and deposition of debris or foreign bodies on the eyelids can cause chalazion development. Regular cleaning and washing of eyelids to remove any deposits can help prevent chalazion.
- Frequent rubbing of the eyes: When children rub their eyes with dirty hands or wash them with unclean water, it can cause chalazion development.

- Hormonal changes: Tween and teens experience rapid changes in androgen hormoneiThe sex hormone responsible for the development and maintenance of male sexual characteristics. , especially around puberty. These changes increase the production and secretion of sebum from the meibomian glands, increasing the risk of developing a chalazion.
- Chronic blepharitis: Blepharitis is the chronic inflammation of the meibomian glands and their ducts due to poor eyelid hygiene, excess sebum production, allergies, or bacterial infections (7). The inflammation in its chronic state leads to the blockage of the sebaceous secretioniThe release of sebum from the sebaceous (sweat) glands in the eyes. , causing chalazion formation.
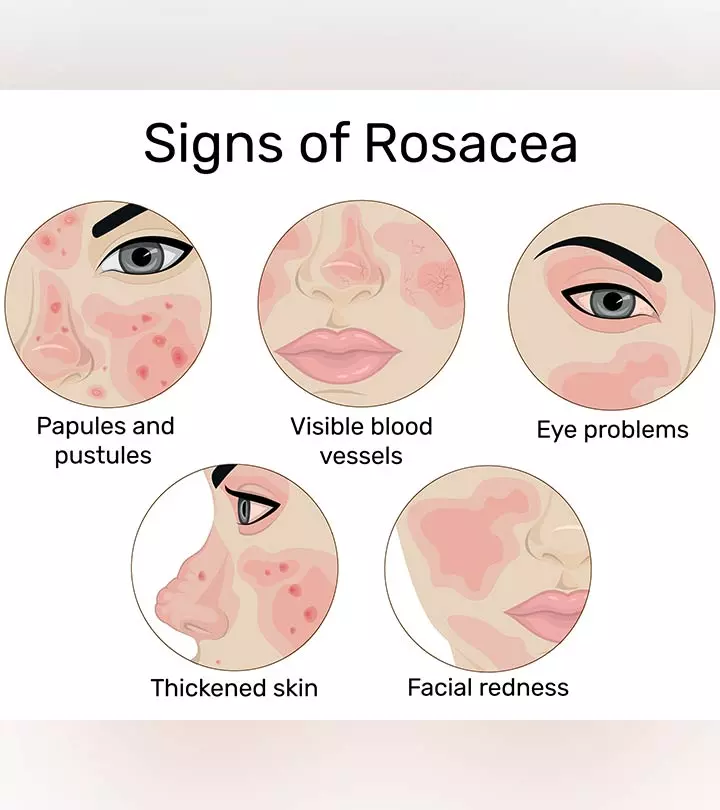
- Acne rosacea: Acne rosacea is a chronic skin condition of unknown etiology wherein the central part of the face, that is, the cheeks, eyes, and nose, becomes red and flushed (8). This inflammatory condition can affect the skin surrounding the eyes and eyelids, causing chalazion development (6) (9).
- Seborrhea: Seborrhea or seborrheic dermatitis is a chronic, inflammatory skin condition affecting the sebaceous gland-rich regions, such as the scalp and face (10). Overgrowth of Malassezia yeast is the likely cause of the condition. Seborrhea could cause chalazion development when the condition affects the eyelids (6).
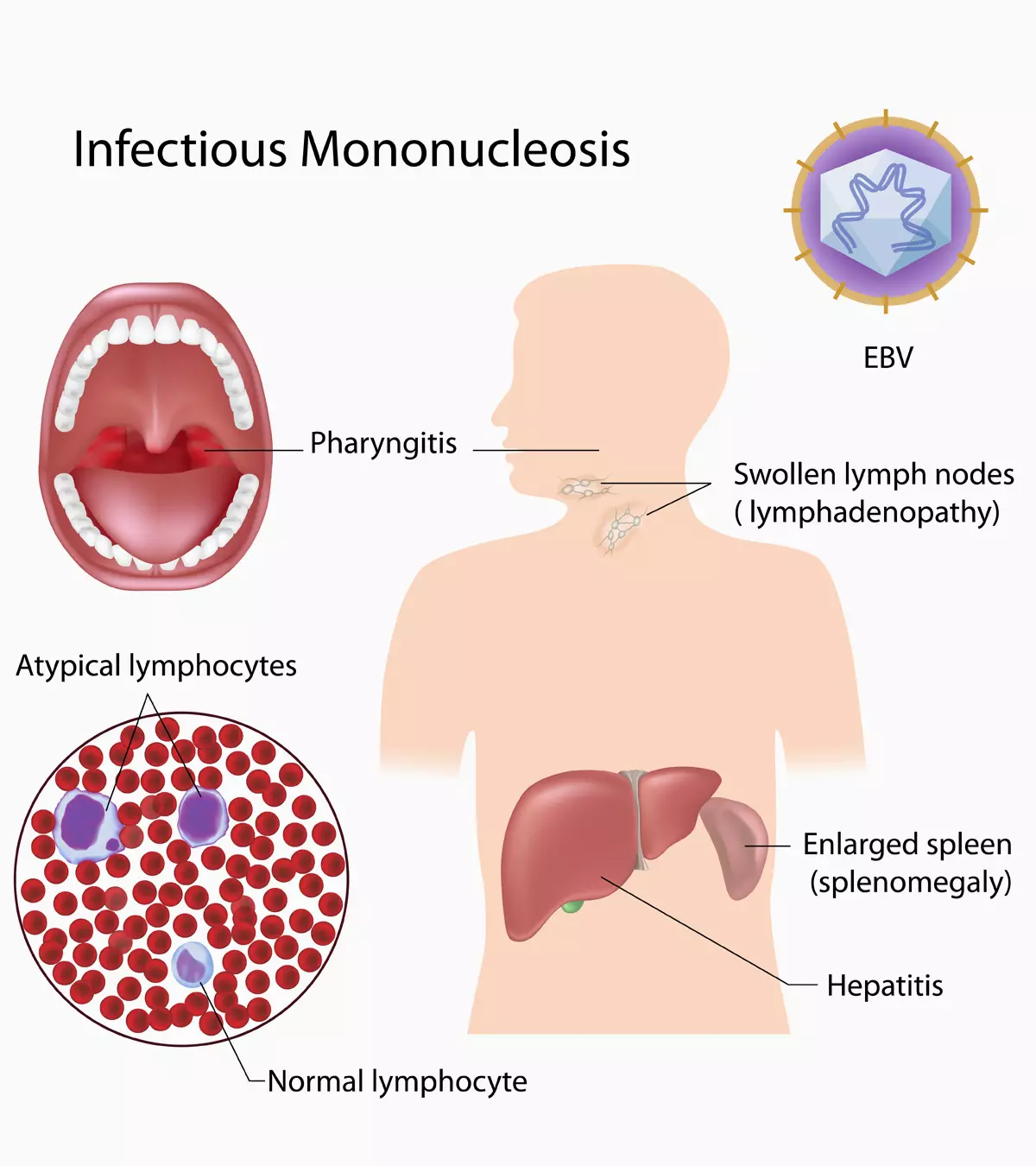
- Bacterial and viral infections in children: Although uncommon, bacterial and viral infections of the meibomian glands and its ducts can cause a chalazion. In such cases, the chalazion may lead to stye in children. Staphylococcus aureus is a common bacteria known to cause 90% to 95% chalazion cases, reports the National Institutes of Health (NIH) (19). A chalazion may also occur following follicular conjunctivitisiAn infectious condition in which the thin tissue that lines the inner part and covers the white part of the eye is red and inflamed. or other systemic infection (6).

Some of the other risk factors for chalazion formation in children include eyelid injury or trauma, exposure to air pollutants, previous history of chalazion, dry skin, tuberculosis, and medical conditions, such as hyperlipidemiaiA condition identified as increased levels of cholesterol or triglycerides in the blood. and diabetes (3) (4) (5).
 Quick fact
Quick factWhat Are The Symptoms Of Chalazion?
A chalazion may develop on the upper or lower eyelids of one or both eyes. The following are the various signs and symptoms of a chalazion (2).
- A chalazion presents as a painless red lump on the eyelid, making the eye appear swollen with mild to no tenderness.
- It can make the eyelid feel heavy and may lead to watery eyes in children.
- Depending on its location and size, a chalazion may press against the eyeball, causing redness in the conjunctiva (the layer of tissue that covers the eyeball). It may also blur vision or block it in extreme cases.
- In rare cases, with superadded bacterial infection, a chalazion may turn tender, red, swollen, and painful.
Younger children may have difficulty expressing their symptoms and rub their eyes, worsening the condition. Keep monitoring them closely to address any concerns promptly. Since a chalazion’s symptoms resemble other medical issues, it is advisable to consult an ophthalmologist (eye specialist) to determine the precise cause.
How Is Chalazion Diagnosed?

There is no single test to diagnose a chalazion. Typically, an ophthalmologist will examine the bump on your child’s eyelid and discuss their symptoms. During the physical exam, they will check your child’s eyes, eyelids’ margins, and oil gland openings. They will also take details of your child’s medical history to ascertain the possible causes for chalazion development (2) (11).
How Is Chalazion Treated?

According to the American Association for Pediatric Ophthalmology & Strabismus, a chalazion is mostly benign and resolves on its own within a few days or weeks (12). Sometimes, large chalazion may take months to heal with minimal medical intervention (4). Yet, if you are worried, consult an ophthalmologist and try the following (2) (5).
- Apply a warm compress to your child’s eyelid four to six times a day. Each time, keep the compression on the eyelid for about ten to 15 minutes. It may soften the hardened oil, triggering the blockage to open and allowing the oil to drain. You can make a warm compress by soaking a clean, soft, cotton cloth in warm water and then squeezing the water out. Instruct your child not to pop or squeeze a chalazion as it could have adverse effects. Anita, a blogger and a mother from Oceanside, CA, shares about her daughter’s chalazion diagnosis. She says, “Laylabug has had a pea sized chalazion on her left eyelid for about 2 1/2 months. We saw a pediatric ophthalmologist who told us to continue with warm compresses 4 times a day for 15 minutes. If the chalazion doesn’t clear in 6 months when we have the follow up appointment he will schedule surgery to remove it. It doesn’t hurt or bother her but it seems to be getting bigger. We were not that consistent about compresses initially, it’s tough to do it on a 1 1/2 yr old, but have been doing them at least twice daily now (i).” Anita’s daughter’s chalazion ultimately subsided and disappeared with consistent warm compresses.
- Gently massage your child’s eyelid for a few minutes a day. It will prompt drainage by putting mild pressure on the duct opening. If the chalazion drains, clean the area using a clean, soft cloth. Instruct the child to keep their hands away from the eye and use a clean cloth to dab their eye if it feels itchy. Tell them to wash their hands before and after touching their eyes to prevent infections. Massaging your child’s eye lids using a baby shampoo may also help (18).
- Over-the-counter (OTC) medicines, ointments, and eye pads may help drain the blockage and control/prevent infection. If a chalazion gets infected, oral antibiotics, antibiotic eye drops, or antibiotic or anti inflammatory ointments or drops may be used. Consult a doctor before you use any medications and follow the correct instructions for use. If the chalazion occurs due to an infection, Tetracycline antibiotics, including Doxycycline and Minocycline, are usually the preferred treatment. Otherwise, the doctor may recommend Metronidazole to treat the infection. Another medical treatment for chalazion is intralesional steroid injection if the infection is not the cause (18).
- Surgical drainage of a chalazion is an option when the chalazion doesn’t go away, or a large chalazion interferes with the vision. The chalazion is drained through an incision in this procedure. This surgery is performed at a doctor’s office under local anesthesia.
The eye will be patched for a day or so after the drainage. There will be some redness, swelling, and pain in the eye for a few days after the removal of the eye patch. You may also notice a pinkish discharge for a day or so. However, if the discharge is yellow or green, it may indicate an infection, warranting immediate medical intervention (13).
In some cases, chalazia may recur, warranting continued treatment and medical monitoring. If a chalazion occurs at the same location often, the ophthalmologist may recommend a biopsy to determine the cause of recurrence, especially to rule out skin cancer.
 Quick tip
Quick tipHow To Prevent Chalazion?

The following steps could ensure chalazion prevention in most cases.
- Guide your child to thoroughly wash their face, with soap or face wash, including the eye area, after waking up and before going to bed. It will help remove the excess oil and dirt stuck around the eyes.
- Instruct them to wash hands each time they touch their eyes or surrounding areas. If they wear contact lenses, they must wash their hands with water and soap before and after handling the lenses. a
- Show them how to use eyelid scrubs or eye wipes to clean the eyelids. Eyelid scrubs may help remove any crust or dirt particles covering the oil gland’s opening (13). A doctor can recommend an appropriate eyelid scrub for the purpose.
- Help them wash their eyes with cold water instead of rubbing them when they feel irritation in and around the eyes.
- Provide sunglasses and guide your child to use them as much as possible for sun protection. You may also provide them with safety glasses to protect the eyes from dust and dirt.
- Have the child take sources rich in omega-3 fatty acids, such as seafood, fish oil, or flaxseed oil, which are essential for eye health (12).
If your tween or teen uses eye makeup, tell them to change their makeup products every three to six months to prevent bacterial growth. They should also avoid sharing eye makeup with others and remove eye makeup before going to bed. The essential issue is cleanliness and hygiene of eyes.
 Quick fact
Quick factWhen To See A Doctor?
It is advisable to see a doctor right away if:
- Along with chalazion, your child has a fever.
- The chalazion becomes painful, red, and swollen.
- The pain, redness, and swelling of the lump don’t resolve even after treatment and care.
- The chalazion is accompanied by other symptoms, such as fever, persistent headache, and severe eye irritation.
Frequently Asked Questions
1. Do chalazions in children get worse before they get better?
If the chalazion is small, it might not cause much pain and go away within a few weeks. However, large chalazion accompanied by any signs of infection must be evaluated and treated promptly (4).
2. Does lack of sleep cause chalazion in children?
Some specialists believe that poor eye hygiene, stress, and insufficient sleep are some factors that may increase the risk of stye and chalazion (14).
3. Is Chalazion in children contagious?
A chalazion is not contagious. It means it cannot spread from one person to another through direct contact or by any other means (17).
4. Is surgery necessary for more severe cases of chalazion in children?
When conservative treatments, such as eyelid massage, OTC medications, and warm compress, do not work, an ophthalmologist may recommend surgical intervention (17). The surgical procedure involves draining the accumulated pus or fluid from the chalazion.
5. Are chalazion in children more likely to recur than in adults?
A chalazion is an uncommon ocular condition with a high risk of recurrence. No clinical evidence suggests that it may recur in children more often than adults (18).
Chalazion in children is an uncommon condition that might require medical attention if it does not show signs of healing after a few days. It is usually painless and mostly occurs due to the frequent rubbing of the eyes or due to a lack of proper hygiene and care of the eyelids. Therefore, it is advised that you teach your child to wash and clean their face regularly and avoid touching their face and eyes with dirty hands. In case the chalazion becomes painful and causes irritation, consult your pediatrician immediately.
Infographic: Complications Of Chalazion
In most cases, a chalazion resolves on its own; however, seeking a doctor’s advice is important. If a chalazion increases in size and is left untreated, it may lead to complications. Read this infographic to learn what complications might arise due to chalazion.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Illustration: Chalazion In Children: Symptoms Causes Risks & Treatment

Image: Stable Diffusion/MomJunction Design Team
Learn about Chalazion, its causes, signs and symptoms, diagnosis and treatment. Get the facts and understand how to manage this condition.
Personal Experience: Sources
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. CHALAZION (KUH-LEY-ZEE-UHN);https://peaceloveandlaylabug.blogspot.com/2012/07/chalazion-kuh-ley-zee-uhn.html
References
1. Styes and Chalazia; University Of Michigan
2. Chalazion; American Optometric Association
3. Chalazion; Cleveland Clinic
4. Chalazion in Children; University of Rochester Medical Center
5. What Is the Difference Between a Stye and a Chalazion? Causes, Symptoms, Treatment; American Academy Of Ophthalmology
6. Alaa Alsammahi et al.; Incidence and predisposing factors of chalazion; International Journal Of Community Medicine And Public Health
7. Blepharitis And Chalazion; University Of Utah
8. What Is Rosacea?; American Academy of Dermatology Association
9. Ocular Rosacea; Eyecare Trust
10. Seborrhoeic dermatitis; DermNet NZ
11. Chalazion | Diagnosis & Treatment; Children’s Hospital
12. Chalazion; American Association for Pediatric Ophthalmology & Strabismus
13. Chalazion; About Kids Health
14. Diagnosing Stye; NYU Langone Hospitals.15. Chalazion; American Association for Pediatric Ophthalmology and Strabismus
15. T A Mustafa and I H Oriafage; Three methods of treatment of chalazia in children; Saudi Med J.
16. Chalazion Management: Evidence and Questions; American Academy of Ophthalmology
17. Chalazion; Queensland Government
18. Gary A. Jordan and Kevin Beier; Chalazion; Chalazion.
19. Davis Willmann et al.; Hordeolum (Stye); NCBI.
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Mubina Agboatwalla
Read full bio of Swati Patwal
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny