Pregnancy may, at times, be difficult to attain for some couples. In such cases, couples may consider IVF and also hear of the term chemical pregnancy. It may lead you to wonder about the difference between a chemical pregnancy and IVF.
Those couples with concerns about infertility can go for fertility treatments like in vitro fertilization (IVF) and intrauterine insemination (IUI)i, two medically approved techniques that assist in artificial conception. However, chemical pregnancy after IVF and IUI is common.
A positive pregnancy test can be an instant source of joy in most families. Unfortunately, many couples suffer from infertility issues that compel them to resort to medical assistance to fulfill their dream of having a baby.
These processes are often tedious and involve an array of diagnostic tests, different hormonal medications, or surgical interventions. However, in the end, these medical techniques may not be a fool-proof solution to a successful pregnancy and come with their own share of adversities. One such phenomenon is referred to as “Chemical Pregnancy.” Continue reading this post as we tell you in detail about this condition, what may cause it, the diagnosis and how it can be prevented.
Key Pointers
- Chemical pregnancy is an early miscarriage often unnoticed by women.
- Causes during IVF include embryo abnormalities, implantation dysfunction, and autoimmune issues.
- Tests like sonohysterogram, ultrasound, blood and chromosome testing aid diagnosis.
- Treatment for recurrent cases includes progesterone supplements, embryo testing, and immune system therapies.
- Lifestyle changes like quitting smoking, reducing alcohol and caffeine intake, and managing stress can help prevent it.
What Is IVF?

Image: Shutterstock
Before we tell you about chemical pregnancy, let’s understand IVF a little better.
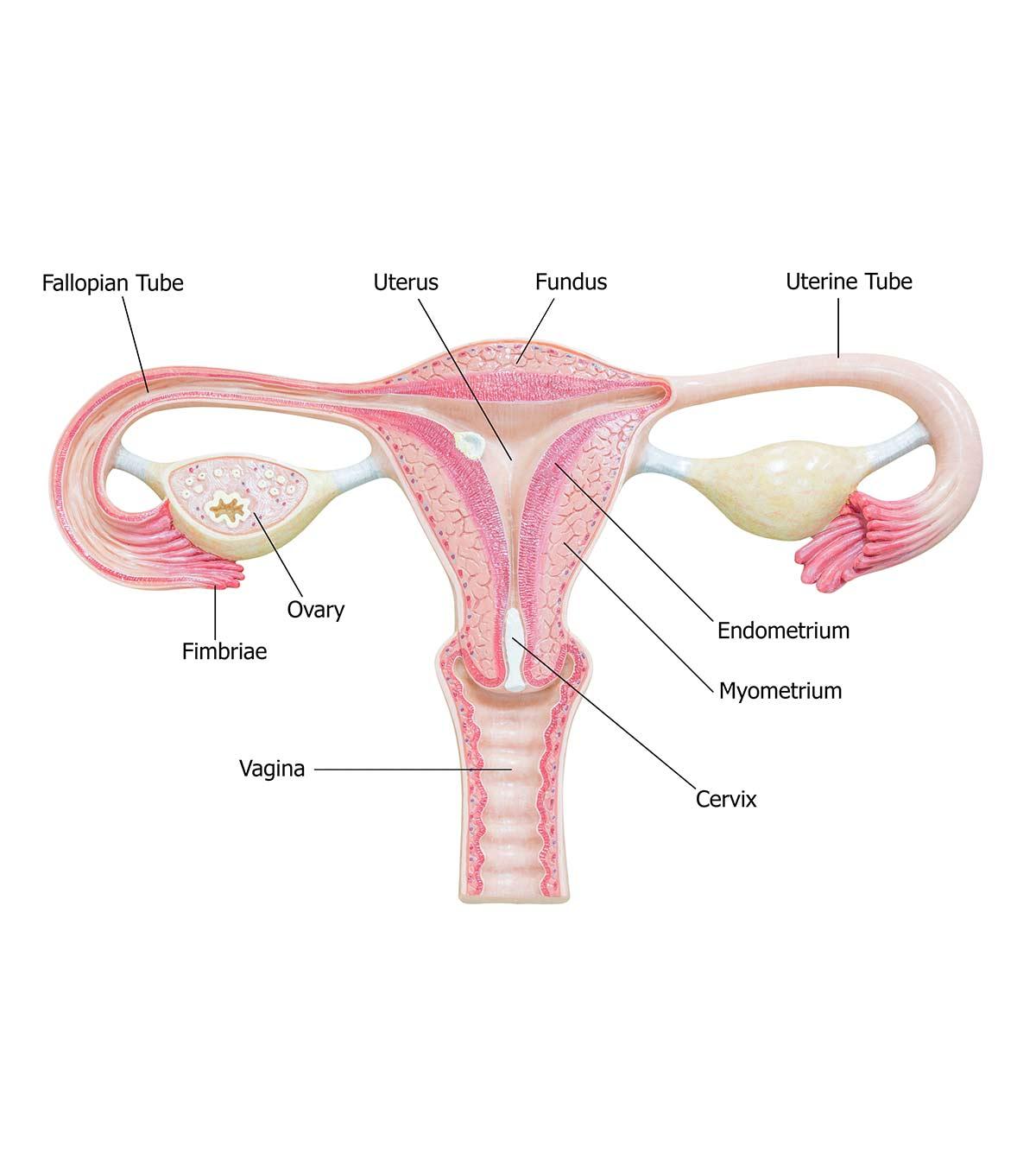
IVF or In Vitro Fertilization is a type of assisted reproductive technology (ART) involving hormone therapy, which encourages the development of numerous eggs in a woman’s ovaries.
These eggs are then collected and fertilized in a test tube using healthy sperm received from a man. These fertilized eggs make embryos that are allowed to grow for 2-5 days. The most vigorous of these embryos are transferred to the uterus. Pregnancy typically begins when these embryos nestle nicely in the uterine lining (implantation). According to the Centers for Disease Control and Prevention, approximately 2.3% of all babies born in the United States are conceived through Assisted Reproductive Technology (ART) annually (1).
What Is A Chemical Pregnancy?
Now that you know, in brief, what IVF is, let’s move on to a chemical pregnancy. What exactly is a chemical pregnancy? How is it different from a miscarriage?
A chemical pregnancy is a practical name given to a pregnancy loss. Here’s a brief account of what a chemical pregnancy entails (2):
- A chemical pregnancy is an early miscarriage, a rather early miscarriage. In fact, more women than you can imagine have a chemical pregnancy but don’t even know about it.
- It usually occurs around the time or a little after your period is due. That is when you are technically four to five weeks pregnant.
- A chemical pregnancy implies that your body did make the hCG (human chorionic gonadotropin) hormone, a sure-shot indicator of pregnancy.
- Most women experience their periods within days of a positive pregnancy test when they have a chemical pregnancy.
- A chemical pregnancy usually does not have differentiating symptoms. It feels like a period that came a little late.
Women who suffer from reproductive health issues such as infertility, especially those undergoing IVF, experience a chemical pregnancy more often than others.
Women with reproductive health issues such as infertility, especially those undergoing IVF, experience a chemical pregnancy more often than others. Women who conceive naturally, in most cases, treat a chemical pregnancy as a late period because they have no clue they were even pregnant in the first place! On the other hand, women using artificial reproductive techniques like IUI and IVF, test (whether HPT or a blood test) a maximum of 14 days after transfer, which allows them to realize an early pregnancy. Unlike clinical pregnancies where a fetus can be seen in an ultrasound and the woman starts to have pregnancy symptoms, chemical pregnancy can be confirmed if there’s an increase in hCG levels in the blood.
Blogger Kimberly Currie observed a second line on the home pregnancy test kit seven days post-embryo transfer, but it faded after ten days. She recounts, “Ten days past transfer, the line was drastically lighter. They (the healthcare team) wanted me to continue the progesterone and come back in two days to see if that number would rise. I went in for my final blood draw ( on the 12th day after embryo transfer). That afternoon, the nurse called me and said she was sorry, but I had a chemical pregnancy and to stop all my medications and that I should expect a period in the next week or so (i).”
Chemical Pregnancy And IVF – Causes
Many women experience chemical pregnancy while undergoing IVF. Here are the major causes of a chemical pregnancy after IVF:
1. Embryo abnormalities
The biggest cause of a chemical pregnancy and miscarriage is embryo abnormality. What exactly does embryo abnormality mean? Well, a normal embryo consists of many chromosomes. But an abnormal embryo contains a disproportionate number of chromosomes. Other factors that can cause the growth of abnormal embryos include structural, chromosomal, epigeneticiStudy of the impact that one’s behavior and environmental factors can have on the way their genes work , and metabolic factors. Older women and women with PCOS (polycystic ovarian syndrome)iA hormonal disorder causing ovaries to produce more than usual male hormones in women are more likely to experience embryo abnormalities during IVF too (3).
 Quick fact
Quick fact2. Implantation dysfunction

Image: Shutterstock
Several chemical pregnancies occur due to implantation failure or dysfunction. Some of the causes of implantation dysfunction include (4)
- Endometrial polypsi Finger-like overgrowth of uterine tissue that occurs in the inner wall of the uterus
- FibroidsiAbnormal non-cancerous growth tissue in the uterus during child-bearing years
- Surgical scarring
- Advanced maternal age
- PCOS
3. Autoimmune issues
Sometimes, a woman’s immune cells are wired in such a way that they attack a growing embryo instead of nurturing it. This happens because the immune system is unable to differentiate between embryo cells and disease-causing cells (5).
4. Other issues

Image: Shutterstock
Other possible causes of chemical pregnancy can include (2):
- Infections (especially sexually transmitted infections)
- Thyroid issues
- Hormonal imbalance
- Endometriosis
- Unbalanced embryo chromosomal translocationsiGenetic mutation that may cause rearrangement of genetic material
 Point to consider
Point to considerTesting To Avoid A Chemical Pregnancy
If you are experiencing repeated chemical pregnancies, it may be time to dig a little deeper.
Some tests that can help unearth the real cause of repeated chemical pregnancies are:
1. Sonohysterogram, hysteroscopy, or a pelvic MRI
Any of these tests can help evaluate the condition of your uterus and pinpoint any abnormalities. It makes sense to undergo these tests before you embark on IVF so that you can avoid chemical pregnancies and early pregnancy losses (6).
2. Ultrasound scan
An ultrasound scan determines the thickness of your endometrial wall lining. If your lining measures less than 8mm, it makes sense to wait till it is thicker before embryo transfer.
3. Natural killer cell activity (NKa) test
This primary immune test can help your doctor to find out if it is your immune system that is causing the chemical pregnancies.
4. Blood tests

Image: S: iStock
If you are undergoing IVF, the chances are high that you would have undergone a plethora of blood tests, including those measuring levels of hormones, such as follicle-stimulating hormone (FSH) and luteinizing hormone (LH). But something may have changed in your body since your last series of tests. So, it is better to take new tests to learn more about your recurring chemical pregnancies.
5. Molecular and biochemical testing
Your doctor can also check the molecular and biochemical factors in your endometrium. These tests can help discover your chances of implantations.
6. Chromosome testing
Thanks to the development of medical science, your doctor can now choose the healthiest embryo to transfer! Tests like using Comparative Genomic Hybridization (CGH) can help identify chromosomally healthy and normal embryos (7).
 Research finds
Research findsIVF And Chemical Pregnancy – Prevention
Once the exact cause is clear, your doctor can go on to treat the condition. Some of the treatment options for recurrent chemical pregnancies are:
1. Progesterone
If your body is not making enough progesterone and that is causing your early pregnancy losses, your doctor may prescribe oral or vaginal progesterone use (8).
2. Baby Aspirin
Baby Aspirin acts as a blood thinner and can help prevent chemical pregnancy in certain women (9).
3. Antibiotics

Image: S: iStock
If an infection is causing you to lose your pregnancies, a course of antibiotics can do the trick.
4. Surgery
As mentioned above, abnormalities in the uterus can in many cases cause chemical pregnancies. In such a case, your doctor may prescribe surgery to fix the problem.
Coping Strategies After A Chemical Pregnancy
Unlike miscarriages, chemical pregnancy occurs at the very early stage of pregnancy. For those trying to conceive through IVF or other fertility treatments, a chemical pregnancy may have a similar effect as a miscarriage. Some coping strategies that may help them through the healing process include:
- Giving yourself time to grieve
- Surrounding yourself with family and supportive friends
- Seeking professional help
- Prioritizing yourself and practicing self-care
- Joining support groups
Frequently Asked Questions
1. When does a chemical pregnancy happen in IVF?
Chemical pregnancy may happen anytime after IVF, and the elapsed time may vary case-to-case basis. Speak to your doctor to understand the phase when you may be at a high risk of experiencing a chemical pregnancy after an IVF (10).
2. What causes early miscarriage in IVF?
Advanced maternal age and atypical uterus shape may increase the risk for early miscarriage followed by IVF. Thyroid disorders, polycystic ovarian syndrome (PCOS), diabetes, sexually transmitted infection (STI), and high or low hormone levels are some other risk factors (10).
3. How long does a chemical pregnancy last?
A chemical pregnancy typically lasts less than five weeks (11).
4. How quickly does hCG drop after a chemical pregnancy?
The drop in hCG levels after chemical pregnancy may vary from one person to another. However, a study found that the average decline in hCG after a chemical pregnancy is approximately 35-50% in the first two days and 66-87% in the next seven days (12).
5. Are you more fertile after a chemical pregnancy?
It is unclear if fertility increases after a chemical pregnancy. Some women may experience no changes in fertility, while others may notice changes (13).
7. Does a faint line mean chemical pregnancy?
A faint line does not necessarily mean chemical pregnancy. Even a successful pregnancy can show a faint line if the test is done too early (14).
Chemical pregnancy and IVF are common concerns for anyone undergoing assisted reproductive technologies to conceive. Chemical pregnancy indicates an early miscarriage where a positive hormone test is the only evidence. Usually, the chemical pregnancy is detected after IVF since the early hormone tests are conducted to determine the procedure’s success. Ultrasound imaging and other tests can be normal. Early pregnancy loss can be like a normal period, and often there can be a slight delay, such as one or two days. Abnormalities of the embryo, issues in the procedure, infections, hormonal issues, and autoimmunity can cause chemical pregnancy. It may go unnoticed, and the hormone levels can be normal while the time most seek testing.
Infographic: What You Should Know About A Chemical Pregnancy?
A chemical pregnancy is early pregnancy loss that occurs even before a woman knows she is pregnant. It is not possible to prevent chemical pregnancy in most cases when the causes are not known. Go through the infographic to learn more facts about a chemical pregnancy. Illustration: Momjunction Design Team
Illustration: Illustration: Chemical Pregnancy After IVF And IUI: Is It A Good Sign?
Image: Dalle E/MomJunction Design Team
Chemical pregnancies can have serious implications for couples trying to conceive. Learn more in this video about the effects of chemical pregnancies, the signs, and what to do next.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Our journey for a miracle baby; Our IVF journey.https://kimberlycurrie.blogspot.com/
References
- Chemical Pregnancy: Here Are The Facts.
https://rmccares.org/2019/10/08/chemical-pregnancy-here-are-the-facts/ - In Vitro Fertilization (IVF).
https://fertility.wustl.edu/treatments-services/in-vitro-fertilization/ - Recurrent pregnancy loss.
https://fertility.wustl.edu/learn/multiple-miscarriages/ - Assessment and treatment of repeated implantation failure (RIF).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3510376/ - Recurrent pregnancy loss and autoantibody profile in autoimmune diseases
https://academic.oup.com/rheumatology/article/38/12/1228/1783669?login=false - Sonohysterography.
https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/sonohysterography - Chromosome Analysis Test.
https://www.nationwidechildrens.org/family-resources-education/health-wellness-and-safety-resources/helping-hands/chromosome-analysis-test - Arri Coomarasamy et al.; (2020); Progesterone to prevent miscarriage in women with early pregnancy bleeding: the PRISM RCT.
https://pubmed.ncbi.nlm.nih.gov/32609084/ - Anticoagulant drugs for the prevention of recurrent miscarriage in women with antiphospholipid antibodies.
https://www.cochrane.org/CD012852/anticoagulant-drugs-prevention-recurrent-miscarriage-women-antiphospholipid-antibodies - Chemical Pregnancy.
https://my.clevelandclinic.org/health/diseases/22188-chemical-pregnancy - Chemical Pregnancy;
https://www.miscarriageassociation.org.uk/information/miscarriage/chemical-pregnancy/ - Predicting the Decline in Human Chorionic Gonadotropin in a Resolving Pregnancy of Unknown Location
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3752097/ - Trying to Conceive After an Early Pregnancy Loss: An Assessment on How Long Couples Should Wait;
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4780347/ - 5 Things to Remember During the Two Week Wait;
https://www.lancastergeneralhealth.org/health-hub-home/motherhood/getting-pregnant/5-things-to-remember-during-the-two-week-wait
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Karla S. Sanchez-Banos
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das