Image: Shutterstock
A chemical pregnancy is a miscarriage that happens before five weeks, immediately after the embryo implants (1). It is a pregnancy that home pregnancy tests or blood tests may confirm but is not seen on an ultrasound. It is also called a biochemical pregnancy (2).
Most women do not know they are pregnant when they have an early miscarriage. About 50-75% of all miscarriages are chemical pregnancies (3). Read this post to learn more about the causes, chemical pregnancy signs and symptoms, risk factors, and diagnosis of chemical pregnancies.
Key Pointers
- A chemical pregnancy, also known as a biochemical pregnancy, is a type of miscarriage that happens when the embryo implants but is lost before five weeks of pregnancy.
- Chemical pregnancies account for over 50% of all spontaneous abortions.
- Symptoms of chemical pregnancy include abdominal cramps, spotting before the next period, and a positive pregnancy test that eventually turns negative.
- Possible causes of chemical pregnancy are improper implantation, chromosomal abnormality, low maternal body weight, and insufficient hormone levels.
- An ultrasound is used to confirm a clinical pregnancy.
Symptoms Of Chemical Pregnancy

Chemical pregnancy symptoms may vary from one woman to another. While some women do not experience any symptoms, others may notice the following miscarriage symptoms (2).
- A positive pregnancy test that soon turns negative.
- Spotting for a week before the period is due
- Mild abdominal cramping
- Vaginal bleeding after a positive result
- Low HCG levels in a blood test
 Did You Know?
Did You Know?However, some women may experience more severe symptoms. An anonymous blogger shares the symptoms she experienced with her chemical pregnancy, “I woke up one morning without the hunger pangs that had been haunting me the past week. I thought it was because I had finally figured out how to eat and control my hunger by eating a larger snack before bedtime. I got out of bed and went to the bathroom. I saw spotting. My heart fell, and I frantically tried to think of a benign reason why I might see spotting. Wildly, I told myself it was implantation bleeding, except I knew it wasn’t. It was long past the time for implantation. A few minutes later, I began bleeding more heavily. I was having a chemical pregnancy (when a heartbeat is detected, it then becomes a clinical pregnancy). I was really sad about this loss and didn’t take it well for a couple of days. The cramping was awful. People have described it as being a bad period cramp. It was way worse than that. I laid contorted in pain on the couch, but worse than the physical pain was the emotional pain of losing a pregnancy that I so badly wanted (i).”
Causes Of A Chemical Pregnancy
While the exact cause is not always identifiable, it may happen due to one or more of the following reasons (3) (4).
- Chromosomal abnormalities in the embryo
- Inadequate hormonal levels
- Improper implantation which can occur due to issues such as uterine abnormalities or poor-quality embryos
- Problems with the uterine lining (due to anatomical, immunological, or other reasons)
- Low maternal weight

- A problem with the DNA of the sperm
- Low progesterone levels
- Unsuccessful IVF
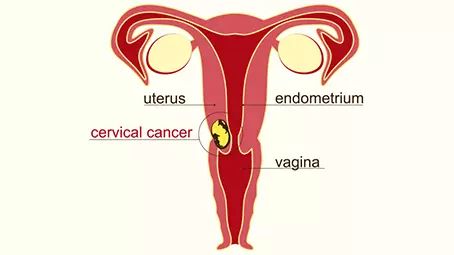
Chemical Pregnancy And Clinical Pregnancy
The main difference between a chemical and a clinical pregnancy is that ultrasound can confirm a clinical pregnancy.
A gestational sac and fetal heartbeat are seen in clinical pregnancy, whereas not detected in a chemical pregnancy.
Risk Factors For Early Pregnancy Losses
The following factors may increase one’s risk of experiencing a miscarriage early in pregnancy (5).
- Advanced maternal age
- Alcohol consumption
- Excessive caffeine consumption
- Cigarette smoking
- Cocaine abuse
- Blood clotting disorders
- Thyroid problems

- Certain maternal diseases—chlamydiaiA bacterial infection spread through oral, anal, or vaginal intercourse , listeriaiA type of bacteria that contaminates the food and causes listeriosis infection , syphilisiA sexually transmitted bacterial disease, typically causing sores in the genital and oral regions, linked to fetal complications , toxoplasmosisiAn infection caused by the Toxoplasma gondii parasite, typically found in undercooked meat, animal feces, and contaminated soil , vaginal mycoplasmaiThe most common microorganisms to cause genital infections , ureaplasmai Bacteria found in urinary or reproductive tracts and is primarily transmitted through sexual contact , etc
- Certain medications—venlafaxine, retinoids, paroxetine, NSAIDs, methotrexate, itraconazole, etc
- Obesity
- Previous history of miscarriages
- Abnormalities in the reproductive tract, such as uterine anomalies, short cervix, and uterine adhesions
- Exposure to toxins—pesticides, radiation, some gases, etc
 Quick fact
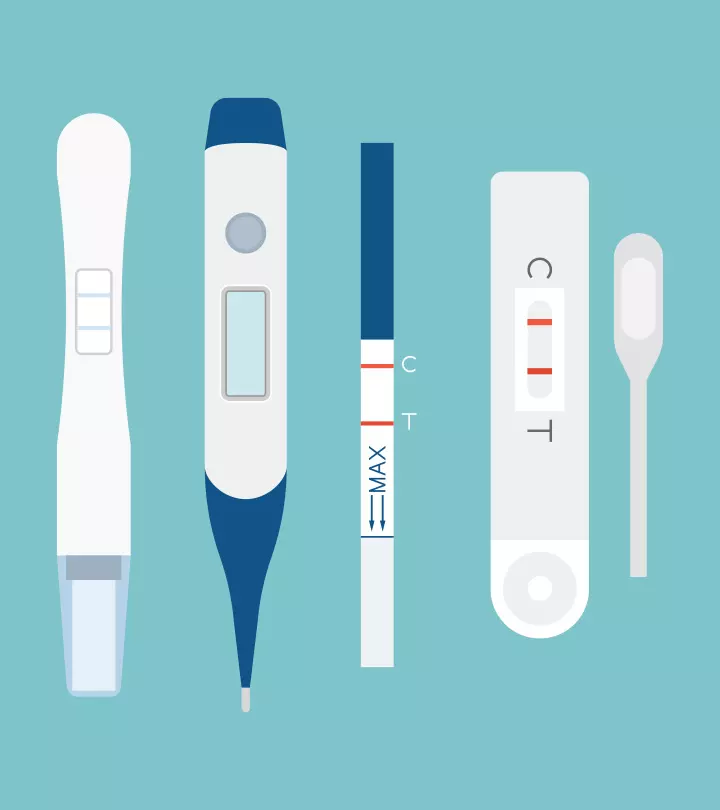
Quick factDiagnosis Of A Chemical Pregnancy

Women who test positive in home pregnancy tests or blood tests and then test negative in the next few days might be asked to go for additional blood tests. If the pregnancy hormones show a declining pattern, it might indicate a chemical pregnancy (1). However, these blood tests are not suggested for all women.
Carrie, a working mother, shares her experience when her OB/GYN ordered some blood work to detect pregnancy hormones to confirm a viable pregnancy. She says, “On Sunday morning, I got a positive pregnancy test. The blue + sign was very faint but definitely present, so I rushed out to the store to purchase another test…just to be sure. Sure enough, the pink lines revealed the same result. I was pregnant! Evelyn would be a big sister! Michael and I were immediately excited, even though we were also a little cautious. On Monday, I called my OB/GYN, and they ordered the blood work. On Tuesday, when I called to get the results, a nurse told me that my HCG was only 10. She said that anything higher than 5 is considered positive, but it was lower than they wanted to see. Immediately, my heart sank. She told me they would test again in a few days to see if the number was higher. She said it would be best to wait until Friday or Monday if I could… I had decided that I would go back for more blood work on Friday instead of waiting all weekend, and I had an extra pregnancy test I was planning to use on Thursday morning just to see if the line got any darker (or lighter)… So, in the wee hours of Thursday morning, Evelyn woke up with a fever… At 2:30 am, this was as close to FMU (first-morning urine) as I was going to get. I waited a few minutes and cautiously looked at the stick. There was the faintest line, just barely visible, and much lighter than the one from just two days ago… When I woke up later that morning, Aunt Flo made her appearance, and that stick in the trash can stared back at me with its stark white face (ii).”
Treatment For A Chemical Pregnancy
As many women are not aware of their pregnancy until five weeks of gestation, miscarriage from a chemical pregnancy may be misunderstood for a usual or a late period. While some women may experience a little heavier blood flow with clots, others may have a blood flow similar to their usual period.
For women with Rh-negative blood group, the healthcare provider may administer a shot of Rh immunoglobulin after experiencing a pregnancy loss. An Rh-negative mother with an Rh-positive fetus might face some complications that may be avoided by the shot (6).
These miscarriages occur early in the pregnancy, and for most women, they resolve naturally, and no treatment is needed. However, the recovery is quick, and the doctor may ask you to try again after one menstrual cycle (1) (2). It’s important to follow all the doctor-recommended precautions after the miscarriage to ensure a healthy recovery.
Prevention Of Chemical Pregnancy
While it is not always possible to prevent a chemical pregnancy, addressing some risk factors or intervening for treatable health conditions can help prevent a chemical pregnancy (5)
Chemical Pregnancies And IVF

According to fertility experts, a chemical pregnancy after an IUI or IVF cycle is a good sign. This is because assisted reproductive technologies aid in getting pregnant. However, whether or not implantation and pregnancy will happen depends upon the body’s and embryo’s natural processes. Therefore, some IVF specialists consider a chemical pregnancy as good news as it confirms a woman’s ability to get pregnant and is a sign of hope that they will get pregnant in the future.
Frequently Asked Questions
1. How long do I bleed after a chemical pregnancy?
The duration of bleeding varies from woman to woman. In some, bleeding and cramping may last only a few hours, whereas, in others, it may last for a few days.
2. Can stress cause chemical pregnancy?
Chronic stress can adversely affect the health of the mother and her unborn baby. However, no direct link was found between stress and a chemical pregnancy.
3. Will I pass tissue with a chemical pregnancy?
The amount of blood a woman loses during chemical pregnancy varies. However, most women pass tissues from the uterus usually at the same time they have their period (8).
4. What is the emotional impact after a chemical pregnancy and how to find support?
Experiencing a chemical pregnancy can be emotionally challenging for women, often bringing feelings of loss, confusion, and grief. The brevity of the pregnancy may leave them struggling to validate their emotions, as others might not fully understand the depth of their pain. These emotions can include guilt, sadness, or even isolation, making it essential to seek support. Talking to trusted friends or family can provide comfort, while counseling services offer a safe space to process feelings and heal. Support is vital for emotional well-being and recovery.
Experiencing a chemical pregnancy does not mean you will have more of them. It is common and normal to feel anxious after experiencing a chemical pregnancy. However, consult your doctor if you experience one or multiple chemical pregnancies.
Infographic: Causes Of A Chemical Pregnancy
Chemical pregnancy can be emotionally challenging. You learn you are pregnant and, after a few days, experience pregnancy loss suddenly. The infographic below explains the reasons why a chemical pregnancy may occur. Exploring the reasons behind a chemical pregnancy can provide insight and support for those affected by this early pregnancy loss. Illustration: Momjunction Design Team
Illustration: What Is Chemical Pregnancy? Causes Symptoms And Treatment

Image: Dall·E/MomJunction Design Team
Navigating yourself through a chemical pregnancy is a heart-wrenching journey. Gain insights into this type of miscarriage and discover strategies for coping through an enlightening video below.
Personal Experience: Sources
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. My chemical pregnancy and miscarriage.https://afastpacedlife.wordpress.com/2020/12/16/my-chemical-pregnancy-and-miscarriage/
ii. Chemical pregnancy (and the problem with testing too soon).
https://ascenicdetour.wordpress.com/2013/08/05/chemical-pregnancy-and-the-problem-with-testing-too-soon/
References
- Chemical pregnancy
https://www.tommys.org/baby-loss-support/miscarriage-information-and-support/types-of-miscarriage/chemical-pregnancy-information-and-support - Chemical pregnancy
https://www.miscarriageassociation.org.uk/information/miscarriage/chemical-pregnancy/ - Chemical Pregnancy: Here Are the Facts
https://rmccares.org/2019/10/08/chemical-pregnancy-here-are-the-facts/ - John Jude Kweku Annan et al; (2013); Biochemical Pregnancy During Assisted Conception: A Little Bit Pregnant
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3712881/ - Office Management of Early Pregnancy Loss
https://www.aafp.org/pubs/afp/issues/2011/0701/p75.html - Early Pregnancy Loss
https://www.acog.org/womens-health/faqs/early-pregnancy-loss - Trying to conceive soon after a pregnancy loss may increase chances of live birth
https://www.nih.gov/news-events/news-releases/trying-conceive-soon-after-pregnancy-loss-may-increase-chances-live-birth - Early Pregnancy Loss.
https://familydoctor.org/condition/early-pregnancy-loss/ - Chemical Pregnancy.
https://my.clevelandclinic.org/health/diseases/22188-chemical-pregnancy
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Pamela Adhiambo Muga
Read full bio of Dr. Ritika Shah
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das