Image: ShutterStock
Like adults, cardiopulmonary resuscitation in children can also help save a life. Nobody anticipates these health emergencies, but it can help to be hands-on with certain first-aid techniques such as cardiopulmonary resuscitation or CPR. If a child stops breathing for any reason, CPR can help avoid fatality.
In addition, getting prompt CPR from a CPR-trained adult in an emergency can help in quick recovery and better outcomes. Read this post to know indications for CPR in children, steps on how to perform CPR, and other important things to remember while performing CPR for children.
Note: This post is only an informational source and not a substitute for professional CPR training.
Key Pointers
- Cardiopulmonary Resuscitation (CPR) is followed when a child is not breathing or has a weak or no pulse.
- One or two rescuers can perform the procedure that involves compression, airway, and breathing.
- Compression improves blood circulation to the heart and other organs, airway relieves obstructed airway, and breathing helps to breathe in some air.
- The child should not bend the elbows or cross the hands during compression.
What Is CPR For Children?
CPR is a life-saving procedure in which a set of life saving steps are followed when a child is not breathing or when there is weak or no pulse.
This procedure involves compressing the chest to keep the blood circulation going and inducing artificial respiration by blowing air directly into the victim’s mouth.
When Would You Perform CPR On A Child?
CPR is performed when the child is unconscious and not breathing or gasping due to drowning, suffocation, choking, cardiac arrest, and trauma. According to a meta-analysis conducted by several institutions, it was observed that the mortality rate for out-of-hospital cardiac arrest (OHCA) among children is as high as 70%. To mitigate this statistic, administering CPR in these situations can be crucial in lowering the mortality rates.
Follow the below steps before administering CPR:
- Secure the scene first. Make sure that you and the child are in safe surroundings.
- Check if the child is conscious and breathing. Gently shake or tap the child and see if they make any movement or sound.
- Ask “Are you okay?” and see if there is any response.
- If there is no response, then ask someone to call the emergency helpline.
- Check for any head or spine injuries, and lay the child on their back.
- Check the pulse for 5 seconds. If you find no pulse or less than 60 beats per minute, then you must get ready to perform CPR.
How To Perform CPR On A Child?
1. When there is one rescuer
The single-rescuer CPR involves three basic steps – Compression, Airway, Breathing in the sequence C-A-B. Here the rescuer needs to perform all the steps.
Earlier the sequence used to be A-B-C, but in 2010 the American Heart Association (AHA) changed it to C-A-B. It has been observed that in the A-B-C sequence, chest compressions are delayed as the rescuer is trying to open up the airway, whereas in the C-A-B sequence the compressions are administered sooner and the delay in ventilation is minimal (1).
Steps Involved in one-person child CPR
Compression: Chest compressions help in improving the blood circulation to the heart, brain, and other organs.
- Position the child on their back on a firm and hard surface.
- Remove any clothing that is obstructing the chest.
- Get down on your knees next to the child’s neck and shoulders.
- The correct hand placement for child CPR is to place the heel of the hand on the lower half of the breast bone in the middle of the chest in a line connecting the nipples.
- For infants, use two fingers (middle and ring) to give compression. For children less than eight years use the heel of one hand and for older children use two hands as shown in diagram below.
 Things to know
Things to know- Put your body weight on your hands by keeping your arms as shown in the below illustration:
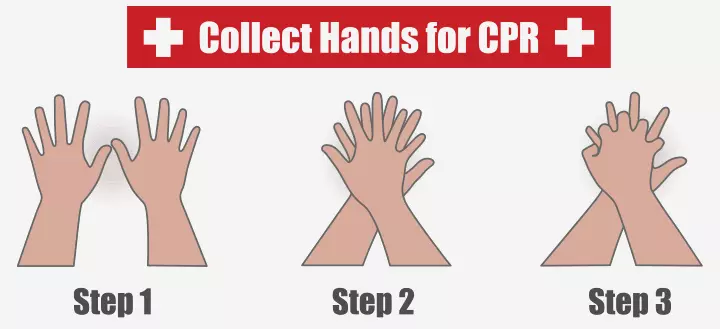
Image: Shutterstock
- After you have secured the position, give compressions hard and fast, and this part is crucial.
- Each compression must be one-third in depth of the chest anterio-posterior diameter or two inches (5cm) deep, and be given at a rate of at least 100 compressions/ minute.
- Allow the chest to recoil between two compressions.
- Count out and perform 30 compressions.

Image: Shutterstock
Airway: After successful compressions, revive the child’s obstructed airway.
- Tilt the head/chin of the victim back only when there is no head injury.
- With your fingers on the lower jaw, gently lift the jaw to bring it upward. Make sure you press the bony part and not the soft tissue as it may further obstruct the airway. Also, avoid using the thumb to lift the jaw.
- This helps the child’s mouth to slightly open.
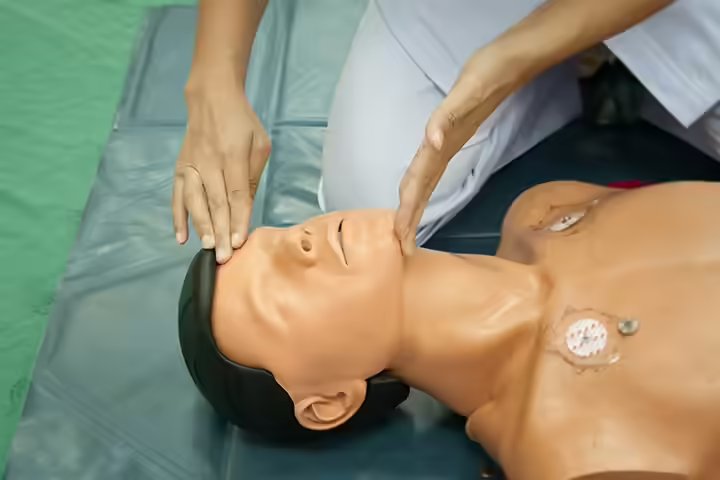
Image: Shutterstock
Breathing: When you have succeeded in opening the child’s airway, the next step is to breathe in some air.
- You may use a barrier device or directly place your mouth into the child’s mouth, pinch their nose with your fingers, and breathe gently and slowly. For infants, cover the baby’s mouth and nose with your mouth and give breaths; each breath must last for a second.
- The chest must rise after every breath; if it does not, then change the position of the head, make a better seal and breathe again. It may be necessary to move the head to various positions to find the optimal airway position.
- Make sure the chest recoils after each breath, repeat and give the next breath.

Image: Shutterstock
Each CPR cycle must comprise 30 chest compressions and two breaths. After the first cycle, check for the pulse and start the second cycle until help arrives or the child is showing a pulse.
2. CPR when there are two rescuers
A two-rescuer CPR is done when two persons are available. If there is a third person to make the emergency call, then the other two can start CPR immediately, else one person must first make the call, while the other person checks the child and prepares for starting compressions.
The two-person CPR is more effective as one person performs the compressions and the other does the breathing. However, it needs good coordination between the two rescuers to sync the breathing and compressions.
Who can do what in a two-person CPR?
If both are certified to perform CPR, then they can take turns in performing the compressions and breathing.
Alternatively, one rescuer may perform a few (say, five) CPR cycles and then the other rescuer may continue.
In two-person CPR, the compression-to-breathing ratio drops to 15:2.
Steps involved in two-person child CPR
Compression:
The rescuer-1 (R1) must check for the pulse by placing the hand on the neck of the child and start compression, while the rescuer-2 (R2) will make the emergency call and take up airway and breathing (2).
- Compressions must begin immediately and done in the same way as mentioned in the one-person CPR.
- The compressions must be hard and fast with 15 compressions to 2 breaths, 100-120 compressions per minute.
- If the R1 is tired, then switch positions after two minutes, but make sure you do not spend too much time switching.
Airway and breathing:
After raising the alarm, the R2 will open the airway.
- Once the airway is opened, the R2 will be ready to give breaths after every 15 compressions (as it is 15 compressions and two breaths in the case of two-person child CPR)
- The R2 can also periodically check the neck for the pulse and encourage the R1 to give effective compressions.
How To Know If You Are Performing CPR Effectively?
Look for the below signs to know if your CPR has been effective.
- The chest recoils after every compression.
- Whenever you administer breathing, the chest must rise indicating that you have opened the airway properly.
- check for pulse near the neck after every 2 minutes of effective CPR.
CPR is only a basic first-aid technique, and the victim must be rushed to the nearest healthcare center at the earliest.
What Are The Important Things To Remember While Performing Child CPR?
| Component | Value |
|---|---|
| Child CPR sequence | Compression-Airway-Breathing |
| Child CPR compression rate | At least 100 compressions/minute |
| Child CPR depth | At least ⅓ depth of the chest AP diameter or about two inches. |
| 1 person CPR compression-to-breathing ratio | 30 compressions: 2 breaths |
| 2 person child CPR ratio | 15 compressions: 2 breaths |
| Chest wall recoil | Complete recoil between compressions |
What Not to Do While Performing Child CPR?
- Do not bend the elbows while performing chest compressions; putting the arms straight helps the right weight to drive the compression and maintain depth.
- Do not cross your hands during compression; to exert the correct amount of pressure, the hands must be over each other.
- Do not bend the fingers into the child’s chest as the force of the compressions must come only from the heel of the hand.
- Do not lean or exert pressure during recoiling, as this will not allow the chest to recoil fully, thus reducing the effectiveness of CPR. At the same time, do not remove your hands from the chest between compressions.
- Do not forget to count the number aloud while doing compressions; this will help you and the others to know at what stage the CPR is. Also, do not reduce the compression number, they must be at least 100 compressions/minute.
- Do not talk much; give your undivided attention to the process.
- You might be in shock in such emergencies, but do not forget to call an ambulance or paramedics.
- Do not do mouth-to-mouth respiration without completing the compressions. Even though the victim stops breathing, there will be oxygen in the blood, and the chest compressions will help in circulation.
- Do not hesitate to perform CPR with the fear that you might break the child’s ribs or cause damage to the chest.
 Point to consider
Point to considerWhat Is Foreign Body Airway Obstruction?
Foreign body airway obstruction (FBAO) is a condition where a foreign object blocks the child’s airway.
FBAO is a common cause of choking in children. Balloons, small objects such as coins, beads, marbles, and food items such as nuts, round candies, grapes, etc., come under FBAO. A child with FBAO will have these symptoms:
- Difficulty in breathing, gasping, coughing and wheezing.
- Cyanosis (bluish discoloration of the skin) and gradual loss of consciousness in the case of severe FBAO.
How To Relieve A Foreign Body Airway Obstruction On A Conscious Child?
Relief management depends on the severity of the condition (3).
- If the FBAO is mild, then encourage the child to cough to flush out the foreign object. While the child is doing that observe for the signs of severe FBAO.
- If the child is unable to cough out the foreign object, then follow the below procedure:
- Place the child’s head down while supporting them in a forward-leaning position.
- While supporting the chest with one hand, give five sharp blows with the heel of the other hand on the back in between the shoulder blades.

Image: IStock
- If the obstruction doesn’t come out, give abdominal thrusts (for children above one year).
- Place both hands around the child’s torso by kneeling behind the child.
- Place the clenched fist between the umbilicus (navel) and xiphisternum (lower part of the sternum).
- Grasp the clenched fist with the other hand and pull inwards and outwards sharply, do this five times.

Image: IStock
How To Relieve An FBAO In An Unconscious Child?
If the child falls unconscious after the back-blows and abdominal thrusts, then shout for help and lay the child flat on the ground. Open the mouth and look for the foreign object; if you can spot it remove with a single finger sweep. Never do the blind finger sweep if you don’t see the object. If you cannot find the foreign object and the pulse seems to drop, then perform child CPR.
Frequently Asked Questions
1. Can CPR be performed on a newborn baby?
Yes, CPR can be performed on a newborn baby. Taking an official course to learn hands-on CPR is recommended, including chest compressions and rescue breaths, since CPR is slightly different for newborns (5).
2. What are the risks associated with CPR on a newborn baby?
Improper CPR on newborns may lead to injuries such as broken ribs. Newborns have softer bones, and even less force can result in harm. Thus, it’s crucial to exercise caution during CPR on newborns (6).
3. What is the success rate of CPR in children?
Currently, no updated pooled prevalence demonstrates survival rates after CPR for pediatric patients. The National Registry of Cardiopulmonary Resuscitation (NRCPR) reports that 43-64% of resuscitated patients achieve a return of spontaneous circulation (ROSC), while 36% live for 24 hours and 25-33% survive until discharge (7).
4. What should I do if the child is not responding to CPR?
If a child doesn’t respond to CPR, call for help and send someone to retrieve an automated external defibrillator (AED) and dial 911. Don’t leave the child alone to proceed to Defibrillation until you’ve performed CPR for about two minutes (8).
5. What should I do if I’m unsure about performing CPR on a child?
If you are not trained in CPR, try the rescue breathing technique (9). Children are more likely to face breathing issues than heart problems and may respond to this technique. If the child remains unresponsive, call emergency services immediately.
Infographic: Notable Points About CPR For Children
In critical moments, performing CPR can be crucial. This infographic provides vital guidelines to remember when performing it on a child. From the correct sequence and compression rate to depth and compression-to-breathing ratios, it acquaints you with key points to deliver effective chest compressions and save a child’s life.
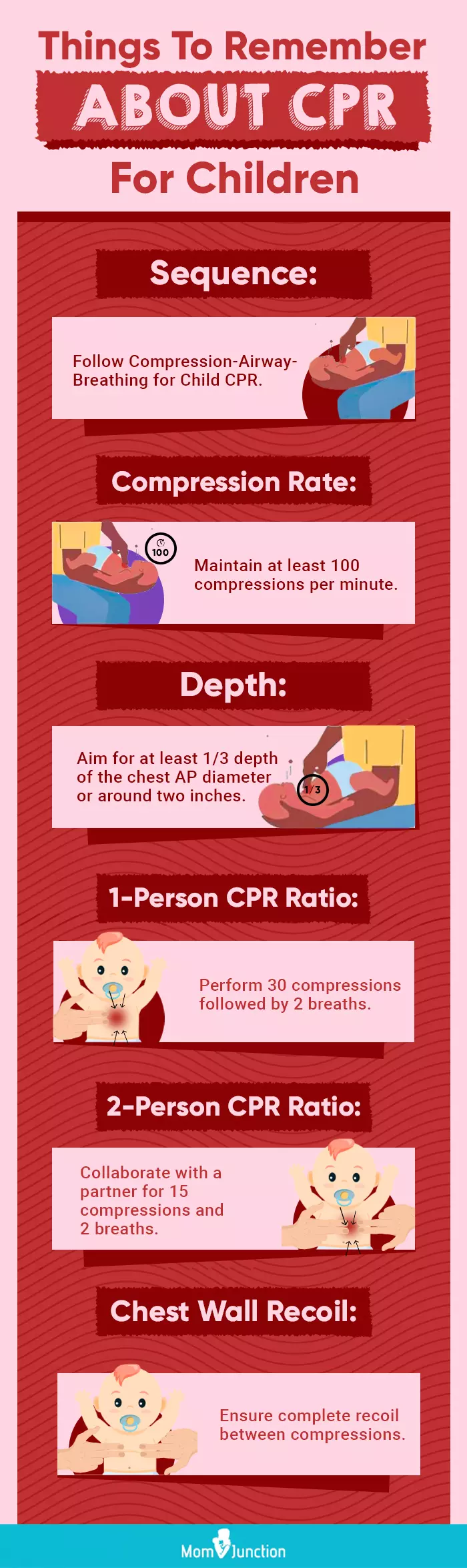
Illustration: Momjunction Design Team
Cardiopulmonary resuscitation in children is a life-saving procedure and an introductory medical training course. It is advisable to take formal CPR training under supervision to ensure that the procedure is learned in the right and most effective way. Also, you must remember to follow the sequence of the procedure correctly. Ensure to contact an ambulance if the situation does not improve. Learning this lifehack can come in handy in case of emergencies.
Have you ever done CPR or seen CPR being done? Let us know in the comments section below.
Illustration: How To Perform Cardiopulmonary Resuscitation (CPR) In Children
Image: Dall·E/MomJunction Design Team
CPR is a life-saving procedure and this video demonstrates how to perform this on a child. Watch the video to gain some valuable insights.
References
1. John M. Field et al. (2010); 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care; AHA Journals
2. Study Guide 2017 BLS for health care providers, CPR Emphasis as of February 2016 for Health care providers; American Heart Association
3. Child Foreign Body Airway Obstruction (FBAO); The University of Warwick
4. CPR – child (1 to 8 years old) Mount Sinai Hospital
5. CPR – child (1 to 8 years old) Mount Sinai Hospital
6. Is it Safe to Perform CPR on Infants?; First Edition First Aid
7. The Success Rate of Pediatric In-Hospital Cardiopulmonary Resuscitation in Ahvaz Training Hospitals; NCBI
8. CPR – child (1 to 8 years old) Information; Mount Sinai – New York
9. CPR-First aid; National Health Service
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Vivek Goswami
Read full bio of Dr Bisny T. Joseph
Read full bio of Swati Patwal
Read full bio of Anindita Ghatak