
Image: Shutterstock
Ear infection in toddlers can cause acute pain, fever, and eating difficulty. Although it may happen to anyone, toddlers are susceptible to it. The condition, also known as otitis media, can occur as a result of pathogenic infection and cause soreness in the ears.
According to the National Institute of Deafness and Other Communication Disorders, five out of six children experience an episode of ear infection at least once by the age of three years, and it is a predominant reason for pediatric hospital visits.AD
If you want to protect your children from it, awareness about the risk factors may help. So read on to know about ear infections in children, including their causes, symptoms, treatment, and home remedies.
Key Pointers
- Toddlers are prone to ear infections due to the shorter and more straight eustachian tube that allows bacteria to pass easily into the middle ear cavity.
- Ear infections in children can be caused by common colds, pneumonia, influenza, sinonasal infection, tonsillitis, acid reflux, sore throat infection, etc.
- Symptoms of ear infection include fluid discharge, ear pain, fever, loss of appetite, nausea, loss of balance, and poor response to sound.
- Treatment for ear infections includes a course of antibiotics, insertion of a tympanostomy tube, or removal of tonsils or adenoids.
- Basic hygiene, breastfeeding and immunization of toddlers, and monitoring of allergies can help prevent ear infections.
What Is Ear Infection In Toddlers?
To understand ear infections, one needs to understand the human ear’s anatomy. There are three sections in the human ear – outer, middle, and inner ear. While the external ear and inner ear are isolated, the middle ear is connected to the nasal cavity through a tube called the eustachian tube. The function of the tube is to equalize air pressure and drain the middle ear fluids into the nasal cavity. The tube stays closed for the most part but opens during some functions such as swallowing or sneezing. In infants and toddlers, the eustachian tube is shorter and more straight than curved. Hence, bacteria easily pass from the oral cavity into the middle ear cavity.
The connection with the sinonasal cavity exposes the middle ear to several bacteria and viruses that cause upper respiratory infections. A microscopic pathogen can squeeze and find its way through the closed eustachian tube into the middle ear. Here it infects the mucosal secretions of the middle ear causing an infection called otitis media (1).
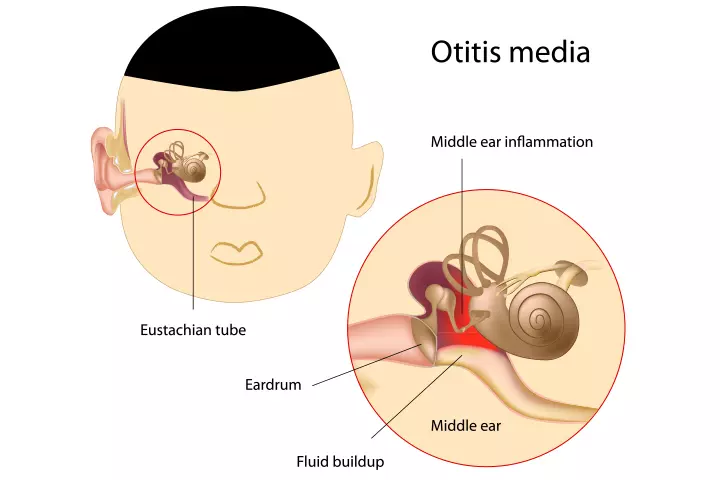
Image: IStock
There are three types of middle ear infection:
- Acute otitis media (AOM): The middle ear suffers an infection due to a bacteria or virus, causing piercing pain and discomfort.
- Otitis media with effusion (OME): The mucous secretions of the middle ear accumulate inside (like the trapped fluid) and are infected by pathogens that cause infection.
- Chronic otitis media with effusion (COME): This is a long-term condition. When the mucus repeatedly gets trapped and infected within the middle ear causing repeated infections.
When ear infection happens in both the ears, then it is called bilateral ear infection or double ear infection. It is essential to learn the cause of an ear infection to understand it better.
What Causes Ear Infections In Toddlers?
Ear infections are among the most common diseases in children. There are several reasons behind a toddler’s ear infection or pediatric otitis. However, some reasons are far more common and widespread.
- Common cold is the leading cause for ear infection among toddlers (2). The cold virus can traverse through the eustachian tube along with the mucus and land in the middle ear, causing an infection.
- Pneumonia and influenza: The pathogens of pneumonia and influenza or flu can lead to an ear infection.
- Sinonasal infection, which is the infection of the nasal sinuses called sinusitis, can lead to a swollen eustachian tube, which can increase the pressure within the middle ear. The swelling also prevents the middle ear from draining its secretions thus causing pain and infection (3).
- Tonsillitis is an infection of the pair of tonsil tissue that lies on either side of the throat. Tonsillitis caused by streptococcus bacteria can quite commonly lead to otitis media (4).
- Adenoid infection: Adenoids are related to tonsils and together are part of the lymphatic system that plays a vital role in the immunity system. Adenoid is located right behind the nasal cavity, and an infection there causes the tissue to inflame and mount pressure on the eustachian tube, eventually blocking it. The trapped fluids within the middle ear get infected by bacteria (5).
- Acid reflux: Ear infection can be a result of a complication of acid reflux also known as gastroesophageal reflux disease (GERD). The refluxed stomach contents can reach the nasal cavity through the laryngopharynx that connects the nasal cavity with the throat (6). From the nasal cavity, the stomach contents reach the middle ear where they cause an infection (7).
- Sore throat infection (Pharyngitis): A bacteria or virus that causes sore throat infection (apart from tonsillitis) can also cause otitis media (8).
- Allergies: A general allergy towards airborne irritants can cause inflammation of the sinonasal cavity. The inflammation traps mucus within the middle ear where the secretions can develop a bacterial infection (9).
- Accumulation of milk in eustachian tube: If a toddler drinks from a bottle while lying on the back, the milk/formula can drain into the middle ear from laryngopharynx. The milk or formula accumulates, with superadded bacterial infection and causes middle ear infection along with pain and inflammation (10).
Some toddlers are at a higher risk than others in developing a middle ear infection.
Who are at risk?
The following toddler groups can have a higher susceptibility to develop middle ear infection:
- Prematurely born: Pediatric experts note that infants born prematurely have a higher risk of developing middle ear infections. The high risk is attributed to the slow development of the immune system and eustachian tube not fully developed (12).
- Exposure to smoke and pollution: Chronic exposure to tobacco smoke and vehicular effluents makes the toddler more susceptible to ear infections.
- Toddlers at daycare: Toddlers who spend a bulk of their time at daycare centers have a higher risk of contracting colds and throat infections, due to droplet infections which can lead to ear infections.

Image: IStock
It is vital to spot the symptoms of ear infection in toddlers to initiate quick treatment and mitigate discomfort.
What Are The Symptoms Of Ear Infection In Toddlers?
A toddler with an ear infection will display the following signs of the condition (13).
- Fluid Discharge From Ear: A clear or yellowish discharge from the ear could indicate pus, which is a collection of white blood cells that attack a pathogen. This occurs when the eardrum bursts open and the pus from the middle ear comes out.
- Unpleasant smell from the ear: An unpleasant odor emanates from the ear canal even if the toddler is otherwise clean. The smell comes from the infected middle ear fluid if it drains out.
- Tugging of ears due to pain: The toddler would pull or pinch the ear due to severe earache and discomfort. The ear ache is quite severe.
- Fever: An ear infection can cause fever without any signs of other visible illnesses. It means the toddler would seem otherwise fine. The fever due to ear infection would be greater than 100.4°F (38°C).
- Loss of appetite: A swollen eustachian tube can make swallowing painful due to high pressure within the middle ear (14). Therefore, the toddler develops a loss of appetite and disinterest in food.
- Nausea and vomiting: Younger toddlers may also experience a constant feeling of nausea or vomiting quite likely due to the pressure within the eustachian tube.
- Poor response to sounds: Since the middle ear is obstructed by infected fluids, sound waves do not reach the inner ear efficiently. It means the toddler would have trouble listening and responding to sounds appropriately. The ears feel blocked and there is difficulty hearing.
- Loss of balance: An inflamed middle ear may put pressure on the labyrinth, which is the part of the inner ear responsible for maintaining the body’s balance. Pressure on labyrinths can disrupt its functions causing loss of balance. And, the toddler would walk in a wobbly or zig-zag way. Or the toddler may feel dizzy.
- General irritability and trouble while sleeping: The toddler will seem irritable and fussy while having trouble sleeping due to acute pain in the ear. They will experience frequent sleep disruption as every time the toddler turns his head to the side of the infected ear, he would squeal in pain.
Take your toddler to a doctor to understand the exact cause of the ear infection.
 Point to consider
Point to considerHow Are Ear Infections In Toddlers Diagnosed?
A pediatrician uses the following procedures to determine the presence of an ear infection (5):
- Ask questions about medical history: The doctor will ask you about the toddler’s medical history to know if he suffered from a cold or throat infection recently. Cold and throat infections commonly lead to ear infection.
- Ear inspection with otoscope: The doctor inserts a specialized camera equipment called otoscope into the ear canal to inspect the eardrum. A reddened or inflamed eardrum indicates an ear infection. This is the most common way to diagnose otitis media.

Image: IStock
- Acoustic reflectometry: Pneumatic otoscope sends short puffs of air to the eardrum. A healthy eardrum flutters due to the air, but an infected middle ear stays stiff. This procedure is called acoustic reflectometry.
- Tympanometry: A tiny speaker with a sensor is placed within the ear canal, and sound waves of different frequencies are emitted. The sensor measures the movement of the eardrum at various frequencies. The extent an eardrum moves can determine the severity of the ear infection. Tympanometry requires the patient to stay still, and not talk. Therefore, it is better suited for older toddlers who can understand instructions.
- Tympanocentesis: In very rare instances, the doctor may pierce the eardrum to collect the infected fluid from the middle ear. This is called tympanocentesis, and the fluid is sent for laboratory analysis to determine the cause of ear infection. This diagnosis could be the last resort when the doctor is unable to decide on the reason behind the ear infection.
Depending on the cause behind the ear infection, the doctor suggests the treatment methods.
How To Treat Ear Infection In Toddlers?
The following treatment procedures could be used to treat an ear infection in toddlers (15):
- Antibiotics: A course of antibiotics are prescribed along with ear drops to alleviate pain and inflammation. The duration of the antibiotic course and the type of antibiotics depend on the severity of ear infection and toddler’s age. Common antibiotics prescribed for ear infections are cefprozil and amoxicillin. If the toddler has a fever, then he would be prescribed fever alleviating medicines such as acetaminophen and ibuprofen.
- Tympanostomy tubes: If a toddler suffers from repeated ear infections, then the doctor may recommend ear tube surgery wherein they insert a tympanostomy tube in the ear. This is done rarely in repeated infections. These tubes are about 1 to 1.5mm in length and made from plastic. It is surgically inserted into the eardrum to provide a passage for the fluids from the middle ear. Since the fluids drain into the ear canal, the middle ear becomes less prone to ear infections. The tympanostomy tube can be designed to stay for as little as six months to three years before they fall off on their own. If the toddler still has no improvement, then a new tube is inserted again. This treatment is a long-term procedure and is only done for toddlers with severe chronic otitis media that repeatedly happens for three consecutive months (5).
- Adenoid or tonsil removal: If a chronic ear infection is a result of repeated adenoid or tonsil infection, then the pediatrician would remove the tissue to provide relief.
Alternate medicines such as homeopathy can be given a try, but only with caution. Most medical experts do not recommend chiropractic adjustment for ear infection treatment as there is no substantial scientific evidence about the effectiveness of the treatment (17).
In most cases, a toddler would not require any treatment and the ear infection would clear on its own. Even antibiotics are prescribed only after observing the toddler for a few days without any medication. Nevertheless, treatment is vital to prevent the onset of complications.
What Are The Complications Of Ear Infection In Toddlers?
When ignored and left untreated, ear infections can lead to the following complications in toddlers.
- Ruptured eardrum: The constant pressure can rupture the eardrum leading to a tear. While an eardrum perforation can heal on its own, it would cause immense pain and lead to a diminished ability to hear. There is repeated ear infection, repeated ear discharge and hearing is affected. Diminished hearing can lead to delayed speech.
- Mastoiditis: The skull bone beneath the ear is called mastoid, and chronic middle ear infection can cause mastoiditis. The mastoid is hollow and has air pockets that drain into the middle ear thus making the bone susceptible to disease as well (16). There is pain and swelling in the mastoid bone.
- Cholesteatoma is the abnormal accumulation of cells right behind the eardrum within the middle ear. The cells form a thickened tissue, which creates pressure on the middle ear bones, leading to their damage (17).
- Labyrinthitis: Chronic middle ear infection can cause pathogens to pass into the inner ear and infect the vital inner ear bone called labyrinth, causing labyrinthitis. The bone is crucial for maintaining body balance and hearing, thus any infection to it can severely impair hearing and movement (18).
- Meningitis: Pathogens from the middle ear can pass into the skull bone called mastoid from where they can find their way into the brain. Once in the brain, the pathogen infects the outer membrane of the brain called meninges thus causing the disease meningitis. This condition is rare and may occur if the ear infection is entirely ignored and not treated (19).
Treatment is essential, but parents also wonder if natural home remedies alleviate the pain caused by the ear infection.
What Are The Home Remedies For Ear Infection In Toddlers?
The treatment of an ear infection is only possible through prompt medical treatment. However, you may try these ways to reduce the intensity of pain:
- Sleep with the sore ear up. It is helpful particularly when the toddler has an infection in only one ear. Let the toddler sleep with their infected ear up, that is, sleep on the side opposite to their sore ear. The middle ear’s fluids trickle into the nasal cavity due to gravity thus relieving pain and pressure (20). Avoid drinking milk from a bottle while lying on the back.

Image: IStock
- Use warm compresses. Placing a moist warm cloth on the ear is certainly effective at cutting down the intensity of the pain.
- Keep the toddler’s nose clear. If the toddler has an ear infection as a result of cold, then he is quite likely to have a runny nose. The nasal secretions could carry more bacteria from the nose to the middle ear. Therefore, it is essential to keep the nose clear of mucus. For younger toddlers, use a nasal suction bulb to pull out nasal congestion. In case of older toddlers, you can use a handkerchief to squeeze out mucus from the nostrils gently.
Remember, experts recommend against the use of any herbal or natural remedy to treat ear infections in toddlers. Also, do not pour tea tree oil or hydrogen peroxide into the toddler’s ear canal or insert earbuds with the objective of curing the pain. Use pain relieving ear drops only after consulting the pediatrician (21).
Also, take care to prevent the ear infection from recurring, to save your toddler from pain.
 Caution
CautionHow To Prevent Ear Infections In Toddlers?
Use these measures to prevent ear infections in toddlers (11):
- Protect the toddler against pathogens: Ear infection is often the result of an infection that begins in the sinonasal cavity or the throat. These infections result from poor protection against pathogens. When you shield your toddler against pathogens that cause diseases such as cold, sore throat, etc., you also protect him from ear infections. In infants, regularly put normal saline drops in the nose. It all begins with good hygiene. For instance, teach the toddler to wash hands after playing, cover mouth and nose if someone sneezes around them, and always wash hands if they pick at their nose. Gargling is very helpful. Also, keep the toddler’s personal items clean to minimize the risk of contracting a pathogen that can cause an ear infection.
- Drink from a cup and not bottle: The American Academy of Pediatrics (AAP) states that bottle-drinking should be discontinued during toddlerhood (22). Instead, you must encourage your toddler to have milk or formula from a sippy cup. In fact, pediatric experts recommend the introduction of open cups right at the age of 12 months (23). Sleeping with milk or formula bottle has been widely linked to ear infections among toddlers (24).
- Immunize your toddler against pathogens that cause upper respiratory infections as they can also lead to ear infections. For instance, immunization against pneumonia and influenza pathogens has proven to prevent ear infections among toddlers (25).
- Stay alert to allergies: If you know your toddler is allergic to something, then proactively prevent him from being exposed to it. Ear infection can happen as a collateral result of suffering a bout of respiratory allergy.
- Prevent exposure to pollution and tobacco smoke: Research has shown that toddlers exposed to secondhand tobacco smoke are more prone to repeated ear infections (26). Automobile pollution also has similar effects. So, keep the toddler away from places where he is likely to inhale vehicular effluents or tobacco smoke.
- Breastfeed your toddler: The AAP recommends breastfeeding even after the first birthday whereas the World Health Organization (WHO) recommends breastfeeding throughout toddlerhood that is even beyond the age of two years (27) (28). Experts consider breastfeeding vital to protect the toddler against several pathogens, including those that can cause ear infections. A research study has noted that babies who were breastfed beyond the age of nine months had 53% fewer chances of ear infections up to the age of six years (29). It means breastfeeding not just protects your toddler in the present, but also offers him substantial long-term protection against ear infections.
Parents may have a few questions about ear infections in toddlers. We answer those queries in the next section.
Frequently Asked Questions
1. Are ear infections contagious in toddlers?
No, ear infections are not contagious. But the pathogen that could have led to the infection can be communicable. For instance, if the ear infection is a result of pneumonia or sore throat then pneumonia or sore throat is contagious but not the ear infection itself.
2. Why does my toddler get ear infections repeatedly?
Toddlers have shorter, narrower, and horizontal eustachian tubes than adults, which makes it easy for bacteria to enter, but difficult for the middle ear’s fluids to exit. Toddlers also have weaker immune system than older children. These factors make them prone to repeated ear infections. However, if parents actively work on it, they can easily prevent chronic ear infections.
3. Can a toddler travel by air with an ear infection?
No, a toddler should not travel by air if they have ear infection as the change in air pressure inside the aircraft can cause piercing ear pain (30). The eustachian tube opens and closes due to cabin pressure, which can cause earache in kids. A toddler can travel two weeks after complete recovery from the ear infection. The AAP recommends consulting a pediatrician before flying with the toddler within two weeks of the ear infection (31). If the doctor finds the toddler’s ear in a healthy state for air travel, then he may recommend doing so.
4. Can swimming cause ear infections in toddlers?
Yes, however, the infection is not of the middle ear, but of the skin of the outer ear canal. The infection does not reach the middle ear and stays restricted to the external ear. For this reason, the condition is called otitis externa or swimmer’s ear (32). Otitis externa usually occurs when excessive water enters the ears as the toddler spends too much time in the pool. The wet conditions eventually cause bacterial and fungal invasion leading to an infection.
5. How long does an ear infection last in toddlers?
It entirely depends on the extent of the ear infection. Pediatric experts state that some toddlers show improvement, without treatment, within 24 hours while in some cases the infection can last for a week. In most cases, the doctor will wait for 72 hours before administering antibiotics to see if the condition improves on its own (11).
6. Can I check for ear infections in my children?
Yes, you may use an otoscope to check for an infection in your child’s ear. However, if pus or blood oozes from the ear, it is better to consult a doctor.
7. Will my child’s ear infection go away without antibiotics?
Antibiotics are occasionally not required for middle ear infections. But severe middle ear infections lasting more than three days require antibiotics (33). Children under six months will require antibiotics if they develop ear infections. The standard treatment in the US is giving the child antibiotic treatment immediately (34).
The Eustachian tube or the ear is shorter and more straight in infants and toddlers, making them prone to ear infections. Otitis media or middle ear infection in toddlers may occur with or without accumulation of mucus. Common cold, pneumonia, sinusitis, tonsilitis, pharyngitis, or allergies may cause such bacterial or viral ear infections. Toddlers born prematurely, are exposed to pollutants, or spend long hours in daycare are more susceptible to being infected. Consult a doctor right away if you observe discharge from your child’s ears or symptoms of ear pain.
Infographic: What Might Trigger Recurrent Ear Infections In Toddlers?
If your little one is experiencing recurrent ear function, knowing the underlying cause and trigger may help prevent a recurrence. Take a look at the infographic below to learn about the various reasons that might contribute to the recurring ear infection in toddlers. Illustration: Momjunction Design Team
Illustration: Ear Infection In Toddlers: Causes Symptoms And Treatment

Image: Stable Diffusion/MomJunction Design Team
The signs of ear infections can be hard to spot in a toddler. Learn what to look for with this educational video on ear infections in toddlers.
References
- Ear infections Kids Health.
https://www.kidshealth.org.nz/ear-infection - Ear infection in children: Frequently asked questions University of Iowa Stead Family Children’s Hospital.
https://uihc.org/childrens/health-topics/ear-infections-children-frequently-asked-questions - Sinus infection (Sinusitis) Cleveland Clinic.
https://my.clevelandclinic.org/health/diseases/17701-sinusitis - Tonsillitis McGovern Medical School.
https://med.uth.edu/orl/2020/01/09/tonsillitis-2/ - Ear infection (Middle ear) Mayo Clinic.
https://www.mayoclinic.org/diseases-conditions/ear-infections/symptoms-causes/syc-20351616 - J Poelmans et al.; (2001); Chronic middle ear disease and gastroesophageal reflex disease: a causal relation?
https://pubmed.ncbi.nlm.nih.gov/11449097/ - Robert C O’Reilly et al.; (2015); The role of gastric pepsin in the inflammatory cascade of pediatric otitis media.
https://jamanetwork.com/journals/jamaotolaryngology/fullarticle/2089813 - Pharyngitis Johns Hopkins Medicine.
https://www.hopkinsmedicine.org/health/conditions-and-diseases/pharyngitis - Middle ear infections (Otitis Media) Kids Health.
https://kidshealth.org/en/parents/otitis-media.html - Ear infection (Otitis Media) Cleveland Clinic.
https://my.clevelandclinic.org/health/diseases/8613-ear-infection-otitis-media - Jacqueline M. Melville and Timothy J M. Moss; (2013); The immune consequences of preterm birth.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3659282/ - Otitis Media (middle ear infection) CHOP.
https://www.chop.edu/conditions-diseases/otitis-media-middle-ear-infection - H. Takahashi et al.; (1996); Cause of eustachian tube constriction during swallowing in patients with otitis media with effusion.
https://pubmed.ncbi.nlm.nih.gov/8800060/ - Ear infections in children, NIH.
https://www.nidcd.nih.gov/health/ear-infections-children#7 - Otitis Media (Middle Ear Infection) Stanford Children’s Health.
https://www.stanfordchildrens.org/en/topic/default?id=otitis-media-middle-ear-infection-90-P02057 - Mastoiditis in Children Stanford Children’s Health.
https://www.stanfordchildrens.org/en/topic/default?id=mastoiditis-in-children-90-P02048 - Cholesteatoma Mount Sinai.
https://www.mountsinai.org/locations/ear-institute/conditions/cholesteatoma - Labyrinthitis and vestibular neuritis, NHS.
https://www.nhs.uk/conditions/labyrinthitis/ - Meningitis CDC.
https://www.cdc.gov/meningitis/index.html - Home Remedies for an Ear Infection: What To Try and What To Avoid.
https://health.clevelandclinic.org/home-remedies-for-ear-infection - Colds coughs and ear infections in children NHS.
https://www.nhs.uk/conditions/baby/health/colds-coughs-and-ear-infections-in-children/ - Discontinuing the bottle Healthy Children.
https://www.healthychildren.org/English/ages-stages/baby/feeding-nutrition/Pages/Discontinuing-the-Bottle.aspx - Sippy Cup Sagas: When to transition Childrens MD.
https://childrensmd.org/browse-by-age-group/toddler-pre-school/sippy-cup-sagas-when-to-transition/ - Otitis Media Childrens Hositals and Clinics of Minnessota.
https://www.childrensmn.org/images/pdf/otitismedia.pdf - Sppech Language and Hearing Sciences Cal State East Bay.
https://www.csueastbay.edu/slhs/ - Health Effects of secondhand smoke CDC.
https://www.cdc.gov/tobacco/secondhand-smoke/health.html - Continuing breastfeeding beyond the first year Healthy Children.
https://www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/Continuing-Breastfeeding-Beyond-the-First-Year.aspx - Breastfeeding WHO.
https://www.who.int/health-topics/breastfeeding - Ruowei Li et al.; (2014); Breastfeeding and risk of infections ar 6 years.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4258846/ - Flying with baby: Parents FAQ Healthy Children.
https://www.healthychildren.org/English/safety-prevention/on-the-go/Pages/Flying-with-Baby.aspx - Travel safety tips Healthy Children.
https://www.healthychildren.org/English/safety-prevention/on-the-go/Pages/Travel-Safety-Tips.aspx - Otitis Externa (OE), AAFP.
https://www.aafp.org/pubs/afp/issues/2001/0301/p941.html - Ear Infection.
https://www.seattlechildrens.org/conditions/a-z/ear-infection-questions/ - Ear Infection.
https://www.cdc.gov/ear-infection/about/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Mubina Agboatwalla
Read full bio of Rohit Garoo
Read full bio of Dr. Ritika Shah
Read full bio of Shinta Liz Sunny
















