Image: Shutterstock

Key Pointers
- Ectopic pregnancy refers to the implantation of the embryo outside the uterus, commonly in the fallopian tube.
- Symptoms of ectopic pregnancy may include pregnancy symptoms, such as nausea and breast tenderness, as well as abdominal pain, vaginal bleeding, hypotension, and fainting.
- Underlying health conditions, inflammation of the fallopian tubes, and hormonal issues are common causes of ectopic pregnancy.
- The risk of ectopic pregnancy may increase in individuals with a history of similar conditions, surgeries, STIs, and advanced maternal age.
- Treatment for ectopic pregnancy typically involves medications or surgery, depending on the severity of the condition.
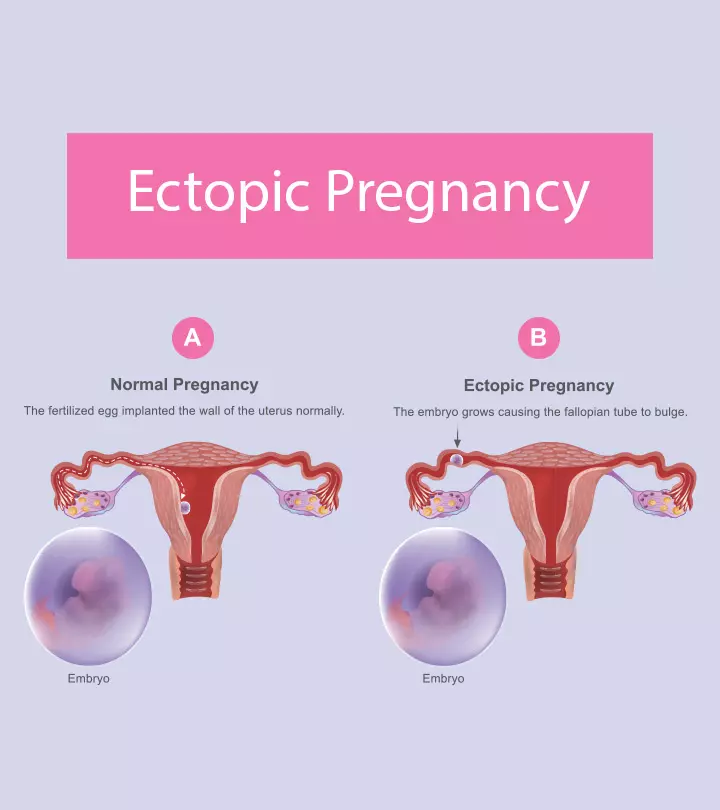
What Is An Ectopic Pregnancy?
Ectopic pregnancy is a pregnancy that occurs outside the uterine endometrium. If left unmanaged, there is a risk of rupture and life-threatening bleeding. It is rare, affecting one in every 100 pregnancies (1). Yet, according to a population-based cross-sectional study conducted by multiple institutes from 2010 to 2019, the prevalence of ectopic pregnancies experienced a marginal rise, increasing from 15.2 to 16.4 per 1000 pregnancies.
The fertilized egg most commonly attaches to the fallopian tube in such a pregnancy, leading to a tubal pregnancy. It can also attach to the cervix, ovary, or somewhere in the abdominal cavity. In most cases, the fertilized egg cannot survive outside the womb in the gestational sac, and the growing tissue can damage surrounding tissues (2).
Read on to know more about the symptoms, causes, risk factors, diagnosis, and treatment for ectopic pregnancy.
Signs And Symptoms Of An Ectopic Pregnancy
Symptoms develop in the early stages of pregnancy and vary from woman to woman. Some women will develop no symptoms until pregnancy ruptures.
During early pregnancy, some women will begin to experience symptoms similar to that of a healthy pregnancy. They may include:
- Missed menstrual period
- Sore breasts
- Upset stomach
- Low back pain or pelvic pain
- Vaginal spotting or bleeding
- Abdominal pain or tenderness
- Mild cramping at one side of the pelvic region
 Quick fact
Quick factAround this phase, it is not easy to understand if it is a normal or ectopic pregnancy. But as the ectopic pregnancy develops, you could experience certain severe symptoms (3):
- Sudden and severe pain in the abdomen, shoulder, neck or pelvis
- Vaginal spotting or bleeding that is light to heavy
- Dizziness, weakness or fainting
- Rectal pressure
Recalling her symptoms and diagnosis of an ectopic pregnancy in her blog, a mother of three says, “I had life growing inside me. Around seven weeks, I came down with what I thought was a stomach bug or problems with my irritable bowel, but then it worsened. I called out sick from work. I felt awful. I laid in bed feeling bloated and terribly uncomfortable. No change of position seemed to help. I had to go to the bathroom, so I stood up and almost passed out. I crawled to the toilet and threw up. I crawled back into bed and thought, my, I’m really sick. The next morning, I had a routine appointment at the midwives’ to meet with a nurse to go over proper nutrition, etc. I met with the nurse, answering many questions about my family’s medical history and mine. She was going to check and see if she could get me in for a quick ultrasound to make sure everything was okay.
She further shares how she went for an ultrasound, upon being guided by her nurse and an ultrasound technician, “After what seemed like forever, she (the technician) spoke as she moved the cursor over a very large, dark area on the screen. She said, ‘See this large, dark area? This is blood. Your abdomen is full of blood.’ After reviewing the ultrasound pictures, one of the two doctors from the group came in and explained what was happening. The fetus attached itself to the wall of my left fallopian tube and began to grow there, producing a positive pregnancy test. As it grew, it ruptured my tube, causing blood to leak into my abdomen. He explained that the pregnancy was not viable and that there was no way to move the pregnancy to my uterus. I would need surgery to remove the pregnancy and repair my fallopian tube (i).”
You should see your doctor if you know about the pregnancy and are experiencing these symptoms.
Causes Of An Ectopic Pregnancy
The exact reason for an ectopic pregnancy is unknown. However, the condition is likely to be associated with one or more of the following conditions (4):
- Scarring or inflammation of the fallopian tubes from a previous infection, medical condition or surgery
- Hormonal reasons
- Birth defects
- Genetic abnormalities
- Medical conditions that influence the shape and condition of the reproductive system organs, such as fallopian tubes
Note that only your doctor can make the correct diagnosis and give you specific treatment options based on the probable cause and risk factors.
Risk Factors For Ectopic Pregnancy
Factors that increase the chances of an ectopic gestation include (4):
- Maternal age of 35 years and more
- Previous ectopic pregnancy
- History of fallopian tubeiTube-like structures connecting the ovaries and uterus that help transport eggs for the fertilization process. , abdominal or pelvic surgeries or multiple abortions
- History of pelvic inflammatory disease (PID)iInfection in the female genital tract characterized by pelvic pain, fever, and abnormal vaginal discharge.
- History of endometriosisiCondition in which tissue that lines a female uterus begins to develop outside the organ leading to pelvic pain and bleeding.
- Sexually transmitted infections (STIs) such as chlamydiaiInfectious, Sexually transmitted bacterial infection causing pain and abnormal discharge in women, sometimes linked to adverse pregnancy outcomes. or gonorrheaiSexually transmitted bacterial infection, which, when untreated, may increase the risk of negative pregnancy outcomes.
- Conception despite intrauterine device intrauterine device (IUD)iSmall, contraceptive copper device (in T shape), which, when placed inside the uterus, helps prevent pregnancy. or tubal ligation
- Conception through fertility drugs and procedures
- Cigarette smoking
- Structural abnormalities in the fallopian tubes
 Research finds
Research findsIf you think you are at risk, discuss with your obstetric or a fertility specialist to minimize the chances of ectopic pregnancies in the future.
How Is An Ectopic Pregnancy Diagnosed?
Diagnosing an ectopic pregnancy is tricky. If the symptoms suggest that you are experiencing an ectopic pregnancy, your doctor may (5):
- Test your blood for the pregnancy hormone, human chorionic gonadotropin (hCG)
- Perform an ultrasound to check the uterus and fallopian tube condition
- Conduct a pelvic examination
If an ectopic pregnancy is confirmed based on the above findings, your doctor will suggest the best treatment plan.
Treating Ectopic Pregnancy
Ectopic pregnancies can be fatal to a pregnant woman. As the zygote cannot survive outside the uterus, it has to be immediately removed for the safety of the mother. Treatment may depend on the pregnancy stage, hormonal levels, and location of the ectopic pregnancy.
- Medication: If your doctor determines that there are no chances of immediate complications, medicinal treatment is suggested. According to the American Family Physician (AFP), the common medication prescribed is methotrexate (Rheumatrex). This drug inhibits the growth of the quickly dividing cells or ectopic mass in this case.
It is available in the form of an injection and results in miscarriage-like symptoms including bleeding, cramping, and the passing of the trophoblast tissue. But the only downside with this treatment is that you will not conceive for several months after taking medicine (6).
- Surgery: The embryo is removed using a procedure called laparoscopy. A small incision is made near the belly button, into which a tiny camera is passed for a better view. The surgeon then removes the pregnancy using surgical tools. Sometimes, the surgery can scar the fallopian tubes, which will then be either repaired (salpingostomy) or removed (salpingectomy) (7).
- Emergency surgery: Ectopic pregnancies can cause serious complications like internal bleeding, infection, and damage to reproductive organs. If your doctor detects these risks, you may need immediate surgery using laparotomy. It involves an abdominal incision and removal of the ectopic mass. Also, the tube may be removed if it is ruptured (7).
 Point to consider
Point to considerAre There Any Side Effects Of Surgery?
The possible side effects of surgery for ectopic pregnancy include bleeding, pain, fatigue, and infection (8)
. Your doctor will discuss these before the procedure.
Home Care After Surgery
Follow the doctor’s instructions to take care of the incision site at home. The primary goal is to keep it dry and clean as it heals. You should also check the incision for signs of infection regularly. This can be:
- Severe and uncontrollable bleeding
- A foul smell at the incision site
- Tender to touch
- Swelling and redness
You may also notice some light spotting and tiny blood clots after the surgery, which could last for nearly six weeks post-surgery.
Here are a few more self-care measures that may help you at home:
- Avoid lifting anything heavy
- Have lots of fluids to treat constipation
- Rest as much as you can
- Avoid sexual intercourse, douchingiA method of cleansing (flushing) the inner vaginal region with water and other liquids. , and using tampons to give some rest to the pelvic area
See your doctor if you feel any pain or that something is not right.
Can You Prevent Ectopic Pregnancy?
No, ectopic pregnancy cannot be prevented entirely, but there are certain ways to reduce the chances of developing it (9).
- Use condoms during intercourse to avoid the risk of sexually transmitted infections and pelvic inflammatory diseases.
- Avoid sex with multiple partners.
- Quit smoking before you try for pregnancy.
Next, we address some common queries for your better understanding of the condition
Frequently Asked Questions
1. Can a baby survive in an ectopic pregnancy?
No, the baby cannot survive in an ectopic pregnancy as it is formed outside the womb. The tissues outside the uterus cannot provide enough blood supply that the fetus needs to survive.
2. How soon would I know if I have an ectopic pregnancy?
You can detect an ectopic pregnancy as early as four to five weeks. Symptoms to look for include a missed period, positive pregnancy test result, severe abdominal pain, spotting, dizziness, or rectal pressure. However, not everyone can detect an ectopic pregnancy through these early signs and may need to get an ultrasound scan.
3. Can a pregnancy test detect an ectopic pregnancy?
Positive urine or blood pregnancy tests can be seen in ectopic pregnancy as well. Beta-hCG levels less than 1,500 mIU per mL may indicate an ectopic pregnancy. However, lower hCG levels can also be seen in a failing pregnancy. The lack of doubling of hCG hormones in 48 hours can indicate ectopic pregnancy in most cases. Diagnostic ultrasonography is required to confirm ectopic pregnancy (10).
4. How long after ectopic pregnancy, will I get my period?
You will get your first period within six weeks after the ectopic pregnancy is terminated. It might not be like a normal period, but heavier or lighter and more painful (11).
5. Can you have an ectopic pregnancy without bleeding?
In some cases, an ectopic pregnancy is absorbed, and there will be no symptoms of vaginal bleeding. According to Andy Raffles, author of ‘Mother and Baby Health: The A-Z of Pregnancy, Birth and Beyond,’ modern ultrasound scans detect ectopic pregnancies that occur without symptoms such as pain or spotting.
6. How painful is an ectopic pregnancy?
Ectopic pregnancy may cause dull and mild to sharp and severe pain (12). You may experience pain in the abdomen, pelvis, and also the neck and shoulder regions.
7. How long does it take to heal from an ectopic pregnancy?
The time for healing from an ectopic pregnancy treatment, whether with medication or surgery, would be four to six weeks (13).
8. Is it possible to remove an ectopic pregnancy without surgery?
Yes, if the fallopian tube has not ruptured and the pregnancy is in its initial stages, your doctor would give you an injection to remove the ectopic pregnancy.
9. Can I have an ectopic pregnancy without a positive test?
Yes, there are chances you could have an ectopic pregnancy without a positive result for a home pregnancy test because of the low levels of the hCG hormone.
10. Can I get pregnant after an ectopic pregnancy?
Most women who experience an ectopic pregnancy can have normal pregnancies in the future. It does not matter if one of the fallopian tubes was removed since one healthy working tube is enough to help the fertilization. The earlier the ectopic pregnancy is removed, the lesser the damage to the tube, the higher are the chances of conception again (14).
If an infection or sexually transmitted disease were the cause for your ectopic pregnancy, then getting the condition treated improves the chances of conception. But, if the ectopic pregnancy occurs due to tubal ligation or exposure to diethylstilbestrol (DES), the chances of a healthy pregnancy are lesser.
If you’ve had an ectopic pregnancy, check with your doctor before you plan for the next pregnancy. Ensure that you give enough time for yourself to heal emotionally and physically, especially if you’ve had surgery to treat it. Dealing with an ectopic pregnancy, when you want to have a child, is not easy. If necessary, join a counseling group or talk to a therapist.
Do you have any experiences to share? Let us know in the comment section below.
Infographic: Factors Increasing The Risk Of Ectopic Pregnancy
Ectopic pregnancy is an uncommon condition that may lead to severe complications if left unmanaged. From hormonal changes to some medical conditions, there are several underlying causes of ectopic pregnancy; however, certain factors also increase the chances of having this condition. The below infographic includes information on such risk factors.
Some thing wrong with infographic shortcode. please verify shortcode syntaxEctopic pregnancy is a serious medical condition. Learn about its causes, signs, symptoms, diagnosis and treatment in this informative video.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Our ectopic pregnancy #1;http://www.thyhandhathprovided.com/2009/12/our-ectopic-pregnancy-story-1.html
References
1. Dr. V Kumar et al.; Tubal ectopic pregnancy; BMJ Clin Evid (2015)
2. Tian Zhu; Ectopic Pregnancy; The Embryo Project Encyclopedia (2010)
3. Signs and Symptoms of an Ectopic Pregnancy; Penn Medicine Lancaster General Health
4. J I Tay et al.; Ectopic pregnancy; BMJ (2000)
5. Heather Murray et al.; Diagnosis and treatment of ectopic pregnancy; CMAJ (2005)
6. Hansa Dhar et al.; Methotrexate Treatment of Ectopic Pregnancy: Experience at Nizwa Hospital with Literature Review; Oman Med J (2011)
7. BS Duggal et al.; Laparoscopic Management of Ectopic Pregnancies; Med J Armed Forces India (2004)
8. Ectopic Pregnancy; The American College of Obstetricians and Gynecologists
9. Albers K; Comprehensive care in the prevention of ectopic pregnancy and associated negative outcomes; Midwifery Today Int Midwife (2007)
10. Ectopic pregnancy; American Family Physician
11. Your body after an ectopic pregnancy; The ectopic pregnancy test
12. Constance J. Creech; Ectopic Pregnancy; JOURNAL OF THE AMERICAN ACADEMY OF NURSE PRACTITIONERS
13. Treatment – Ectopic pregnancy; The National Health Service in England, NHS Scotland, NHS Wales, and Health and Social Care in Northern Ireland
14. Chanda Karki et al.; Ectopic Pregnancy and its Effect on Future Fertility; South Asian Federation of Obstetrics and Gynecology (2009)15. Antonette T. Dulay; Ectopic Pregnancy; MSD Manual
16. Ectopic Pregnancy; ACOG
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Subhashis Samajder
Read full bio of Rebecca Malachi
Read full bio of Dr. Ritika Shah
Read full bio of Reshmi Das