Image: Shutterstock
Bedwetting in children under five years of age is normal since their ability to control their bladder is not strong during this time. Their body is still learning to regulate different functions.
There are two types of bedwetting, primary and secondary. If your child has constantly wet the bed since early childhood, it is called primary bedwetting. However, if they suddenly develop this condition after a long period of normal bladder control, it is called secondary bedwetting. Both require your attention. According to the American Academy of Pediatrics, it was found that 20% of children experience occasional accidents of bedwetting at the age of five, which reduces to 10% at the age of seven, ultimately decreasing to a minimal 1% and 3% in teenagers.
In this post, we explain more about bedwetting in children, including its causes, treatment, and some lifestyle changes and home remedies to alleviate it.
Key Pointers
- Children below five years of age commonly experience bedwetting.
- Causes of bedwetting in children include maturation delay, deep sleep, hormonal imbalances, genetics, lower UTI, and psychological issues.
- Treatment options for bedwetting include pelvic floor exercises, bedwetting alarms, and motivational therapies.
- Natural remedies such as massaging, bladder exercises, walnuts, apple cider vinegar, Indian gooseberry, honey, and jaggery may also help reduce bedwetting.
Why Do Children Wet The Bed?
“The vast majority of children who wet (the bed) are going to stop. That should come as a relief, but it’s still a good idea to get the problem checked if the incontinence issues go on for more than two months,”
says Dr. Franco, a Yale Medicine pediatric urologist (1). It is important to know the cause of bedwetting to stop it. Here, we list some of the possible reasons for bedwetting in children.
1. Causes of primary bedwetting in children
There are no definitive causes for primary bedwetting in children. Below are a few factors that studies have found most relevant for bedwetting in children.
- Maturation delay: This is a commonly accepted cause of primary bedwetting but is difficult to prove. Generally, the body develops the necessary bladder control as the child grows, allowing the children to wake up when they need to pee. But in some children, this bladder control is delayed, making it difficult for them to hold the urine all night, resulting in bedwetting (2).
 Quick fact
Quick fact- Deep sleep: Children who sleep very deeply sometimes miss the brain’s signal that the bladder is full and end up wetting the bed. However, studies show that bedwetting can also be a problem for children who have a normal sleep pattern. It is also found that bedwetting is found in children who experience episodes of sleep apneaiA disorder when breathing repeatedly stops and start breathing during sleep. , with upper airway obstruction (2).

Image: Shutterstock
- Hormonal imbalance: Antidiuretic hormone (ADH) prevents the body from creating excess urine at night. If the child’s body is not producing enough of this hormone, then it produces more urine at night. Combined with the lack of bladder control, this can lead to bedwetting in older children (3).
- Lower urinary tract dysfunction or voiding dysfunction: This could be another reason for bedwetting, in this condition, there would be a dis-coordination between the bladder and the bladder outlet, this causes the bladder not to empty effectively resulting in bladder muscle stiffness (4).
- Genetics: Sometimes, this could be the reason for bedwetting. According to research, in families where both parents had nocturnal enuresis (involuntary urination), there is a 77% chance that the children might develop it too. And if one of the parents had the problem, then there is a 45% chance. The chances of bedwetting would be only 15% if neither of the parents had the habit of bedwetting (1).
- Psychological factors: These also play a role in the development of bedwetting, although studies found that this relationship could be coincidental. Children with a bedwetting habit are said to have a 2.88 times higher risk of having Attention Deficit Hyperactivity Disorder (ADHD)iA neurodevelopmental disorder affecting the child's ability to pay attention, control impulses, and manage energy levels. , which could be due to delayed central nervous system development (5). Furthermore, factors like changes in environment, family dynamics, or bullying may trigger bedwetting. However, this does not mean all bedwetting children would have psychological or emotional issues, and it is best to consult your doctor to clarify your doubts.
 Point to consider
Point to considerBedwetting is no one’s fault. So, there is no point blaming the child or scolding them for it. Exposing the child to bedwetting embarrassment or adding shame to the situation may increase stress and exacerbate the problem. Instead, protect your child’s mental health by not allowing bedwetting stigma to have an impact.
2. Causes of secondary bedwetting in older children and teens
If your child has suddenly developed this bedwetting problem, after at least six months of nighttime dryness, then it could be due to the possible causes we list next. Although there are no major differences in the factors that cause primary or secondary bedwetting, there are a few additional bedwetting causes for your child’s sudden and accidental release (6) (7).
- Acquired urinary tract problems: Some children could develop secondary bedwetting due to urinary tract problems such as tumors. However, there would be other symptoms for such problems, and a doctor’s diagnosis is required (8).
- Poor bathroom habits: Holding urine for too long during daytime can lead to bladder control problems, which could lead to bedwetting in children. This could be the reason for the sudden onset of bedwetting.
- Hormonal changes in puberty: Teenagers go through hormonal changes, which could affect their ADH levels. This can result in increased production of urine when they are sleeping.
Image: Shutterstock
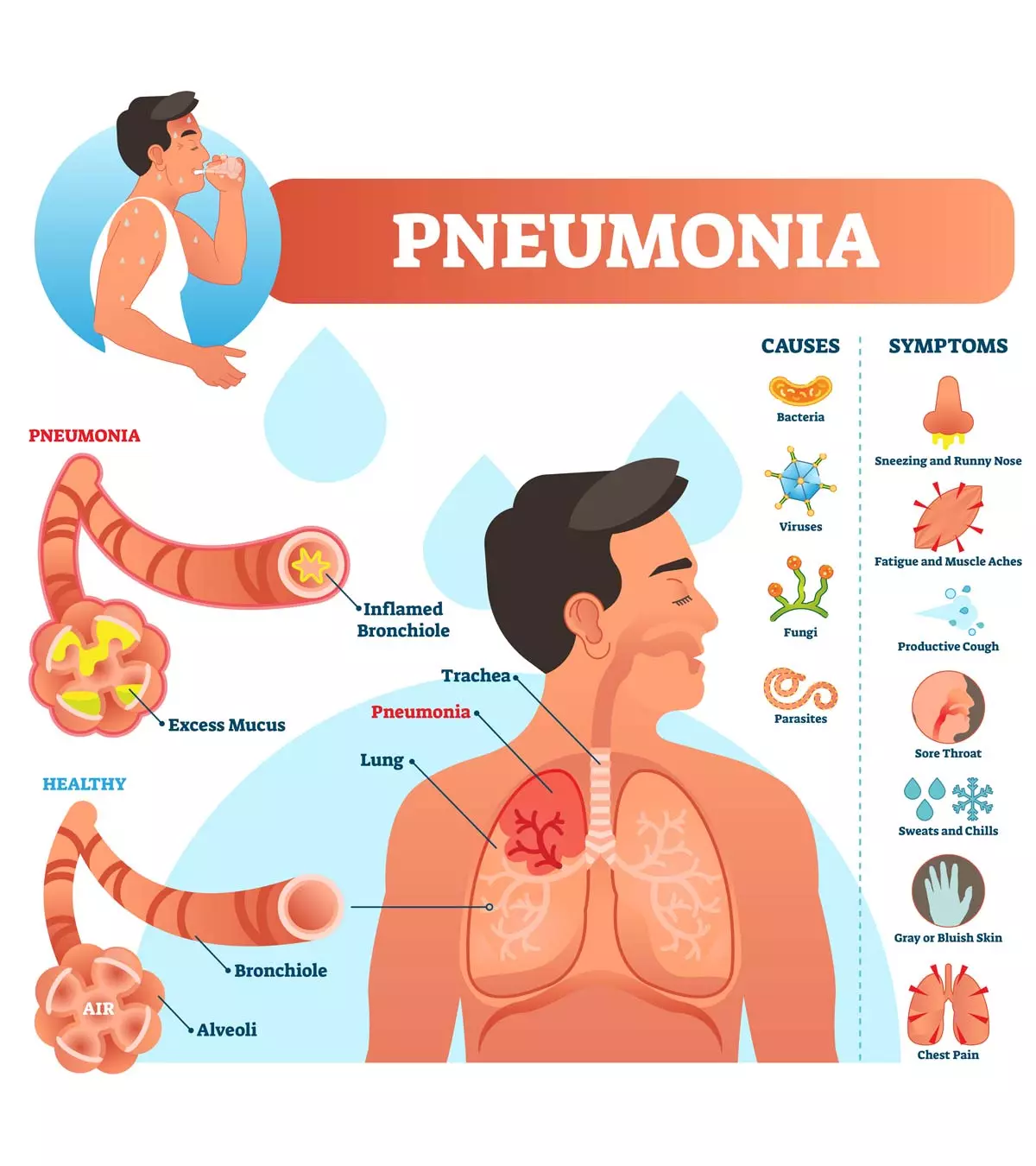
- Medical problems: Secondary bedwetting might also happen due to an underlying medical condition, such as diabetes, urinary tract infectionsiA bacterial infection that occurs when bacteria that typically pass through the skin or rectum infect the urinary system. , and constipation. These conditions can increase the number of times the child urinates during the day and night.
- Psychological problems: Anxiety and stress can sometimes trigger secondary bedwetting in teenagers. If not dealt with early on, it could become a difficult habit. As bedwetting, in turn, causes stress, blaming or reprimanding the child may only worsen the situation.
- Caffeine: If your children have caffeinated drinks before going to bed, chances are they’ll end up with a full bladder before the night is over.
- Constipation: Irregular bowel movements can put pressure on the rectum, thereby might interfere with the nerve signals between the bladder and the brain.
- Sexual abuse: sometimes, children start bedwetting suddenly if they were victims of sexual abuse, look for other signs such as repeated urinary tract infections, vaginal pain, unusual discharge.
- Abnormalities in the nervous system may cause neurological problems that may have enuresis as a side effect (8).
How To Stop Bedwetting In Older Children?
The first step is to visit a pediatrician or pediatric urology expert to find out why your child is wetting the bed. It may not be easy to pinpoint the cause of bedwetting without a proper diagnosis.
Treatments To Reduce Bedwetting In Children
Sometimes, bedwetting could be treated with a few changes in the bedtime routine, while in other cases, it may need medical intervention. Your child’s doctor is the best person to decide on an appropriate bedwetting solution for your child. Still, it is important to know the available treatment options.
The treatment for bedwetting can be categorized into two, behavioral and pharmacological. Usually, combination therapy is recommended based on the underlying cause for bedwetting in your children. Your child’s doctor will tell you more about the treatment required.
1. Motivational therapy

Image: Shutterstock
Also known as Urotherapy, this is considered as the first line of treatment for bedwetting in children. This therapy contains a series of exercises to develop bladder control in children. Regular de-voiding of the bladder, voiding posture, and restricting fluid intake one to two hours before going to bed are a few things that your child’s doctor would train your child on.
It also includes exercises such as pelvic floor muscle training and behavioral modifications. However, a Cochrane review found that Urotherapy was found effective when compared to no treatment but was inferior to other treatments. As this treatment involves no medications, it has fewer side effects (5). Sometimes, cognitive behavioral therapy (CBT) is also included to manage and treat behavioral issues or overactive bladder (1).
2. Bedwetting alarm
In this method, portable bedwetting alarms that the child can wear during night, when the first drops of urine moist the fabric, will set off and wake up the child to empty the bladder. The parents must wake the child if they fail to wake up. However, this method should not be used if:
- The bedwetting is only once or twice a week.
- There is no enthusiasm for participation from either the child or parents.
- If the parents seem to blame the child for bedwetting (5).
Positive reinforcements such as rewarding stickers and positive encouragement are necessary for the continuation and success of these bedwetting management therapies.
3. Pharmacotherapy
This therapy is advised when the bedwetting is due to hormonal disturbances. Medication includes Desmopressin Acetate (DDAVP), which is used to treat the symptoms of the condition. The doctor may also prescribe anticholinergic drugs that help increase the bladder capacity by preventing bladder contractions (5).
 Things to know
Things to knowLifestyle Changes That Might Reduce Bedwetting In Children
You can also try these simple changes in the child’s lifestyle to prevent nocturnal enuresis. These tips and tricks will not completely cure bedwetting but will help the child deal with it.
- Reduce liquid intake during the second half of the day. Let the child drink more water during the day and minimize it during the evening and night.
- Avoid giving the child any bladder irritants such as caffeine, which may be present in cocoa or chocolate drinks, at night. Also, avoid citrus juices, sweeteners, and artificially flavored drinks like sodas.

Image: Shutterstock
- If your child’s daytime bathroom habits are erratic, schedule the breaks through the. Yes, he will say that he “doesn’t have to go.” But encourage him to stick to the schedule. Make sure he goes to the bathroom at least twice within two hours before going to bed.
- Keep the child hydrated to prevent excessive thirst. Keep a water bottle handy for him to sip water whenever he is thirsty. Give them a healthy diet that is rich in fiber to relieve constipation.
- Avoid waking up the child in the middle of the night to go to the bathroom, for that may not help you in the long run. Also, this can make the child cranky due to sleeplessness.
- Talk to them – have an open discussion about the problem. Brainstorm together and ask them to come up with solutions that can work.
- Encourage any progress that the child makes, but do not punish them for not making any.
- Positive thoughts and reassuring themselves can be helpful for older children and teens dealing with bedwetting problems.
 Quick tip
Quick tipNote: These lifestyle changes take time to show effects, so have patience while trying them out. Also, it is best to consult your child’s doctor to know the underlying cause for bedwetting.
Next, we tell you about some home remedies that might help to stop bedwetting in your children.
Home Remedies For Bedwetting In Children
You might help your child address the problem with some effort made at home. Here are a few herbal home remedies and exercises you could try (9).
Most of these remedies are based on anecdotal evidence, so it is difficult to conclude about their effectiveness. Also, these home remedies take significant time to show effect.
1. Massage
Massaging the lower abdomen with olive oil might prevent involuntary flexing of the pelvic muscles that result in bedwetting.
- Warm the olive oil a little.
- Massage the lower abdomen with the warm oil
- Massage every day for the best results.
2. Bladder exercises
A few exercises might help in strengthening the muscles of the urinary tract and stretch them to prevent bladder contraction.
- Holding the pee for 10-20 minutes longer (while having the urge to pee) might help expand the bladder and improve control, but make sure the child does not do it to postpone peeing.
- Another Kegel exercise is to hold and squeeze a small ball (the size of a fist) between the thighs (just above the knees). It might strengthen the pelvic muscles.
Try these exercises at least twice a day to make the pelvic muscles stronger and improve bladder control.
3. Cinnamon
Cinnamon has antioxidant properties and also keeps away diabetes (10). So, if the bedwetting is caused due to a bacterial infection or diabetes, a dose of cinnamon every day might help.
- Give the child a piece of cinnamon to chew, every day.
- You could also use cinnamon powder as a topping on milk, desserts, or bread.
4. Cranberry juice
Cranberry might be useful to treat urinary tract infections, but further studies are needed to prove this. However, you might try giving cranberry juice to your child if the bedwetting is due to urinary tract infections (11).
5. Walnuts and raisins
Walnuts and raisins might help in reducing the symptoms of bedwetting. Give the child a light snack of three almonds and two raisins before he goes to bed. Repeat this every day for a few months until there is significant progress, and the dry spells are longer.
6. Apple cider vinegar
It is believed that apple cider vinegar can also help in bedwetting. It is said to reduce the acidic levels in the tummy, which could irritate the bowel and lead to bedwetting.
- Apple cider vinegar is acidic, so dilute two tablespoons of it with a glass of water.
- You can add honey to make it less bitter.
Give this to the child once or twice a day, preferably with a meal.
7. Indian gooseberry

Image: Shutterstock
Indian gooseberries are an effective Ayurvedic remedy that you can try for bedwetting prevention.
- De-seed the gooseberries and chop them into small pieces.
- Ground the chopped gooseberries and add honey to the mixture.
- Add a little bit of turmeric and mix it well.
Give one spoon of this once every morning.
8. Honey
Giving one small teaspoon of honey for a younger child and one tablespoon for a teen could help reduce the bedwetting.
9. Jaggery
Jaggery increases your child’s body heat and keeps it warm, thus might minimize the bedwetting problem.
- You could give the child a glass of warm milk and a piece of jaggery every morning.
- You can also prepare a treat with roasted sesame seeds and jaggery, combined with a pinch of salt.
10. Mustard seeds
Mustard seeds are recommended to help children with a urinary tract infection (UTI), which can cause bedwetting in young children.
- In half a cup of milk, add half a teaspoon of dry mustard powder (fine).
- Give it to the child to drink an hour before bed every day.
Frequently Asked Questions
1. Can drinking milk cause bedwetting in kids?
Hypercalciuria (excess calcium in the urine) may be linked to bedwetting in children. Calcium-containing foods such as dairy products may need to be regulated if the child is diagnosed with the condition (12). Drinking liquids, especially fizzy and caffeine-containing drinks (hot chocolate, tea, coffee, energy drinks, and cola) just before bedtime can make your child more likely to wet the bed (13).
2. Can childhood trauma cause bedwetting?
Bedwetting in previously “dry” children may be caused due to stress or trauma. The bedwetting may stop once the underlying problem is resolved (14).
3. At what age is enuresis considered a problem?
Most children gain bladder control by the time they reach four years of age. About 10% of them may be unable to stay dry till six or seven years of age and may have day or nighttime “accidents.” Poor bladder control and frequent urination in kids beyond seven years may be considered a problem, and you should seek medical help (15).
4. Will enuresis in children go away?
Nighttime bedwetting in children above five years and even in some teens may not be a serious health issue, and children may outgrow it (16).
5. What are the four types of enuresis?
Enuresis may be classified into four types (17):
- Nocturnal enuresis: It is the most common type that occurs at night
- Diurnal enuresis: Wetting during the day
- Primary enuresis: When a child is yet to fully learn toilet training
- Secondary enuresis: When an otherwise “dry” child reverts to wetting
6. What is the difference between enuresis and incontinence?
Urinary incontinence is the same as enuresis and are the medical terms for bedwetting (18).
Bedwetting is a common condition in growing children that causes embarrassment, so they need all the help they can receive. While maturational delays are the most prevalent cause of primary bedwetting in children, other causes include urinary tract dysfunction, an underlying medical disease, or a psychiatric disorder. The condition could also affect a child’s self-esteem. Therefore, the child may also need behavioral and pharmacological therapy to manage the psychological effects or causes of bedwetting. Encouraging open communication and offering support and reassurance can ease the child’s emotional burden. In addition, various lifestyle changes and certain home remedies could also help.
Infographic: Lifestyle Changes That Might Reduce Bedwetting In Children
Bedwetting, or nocturnal enuresis, is a common issue among children. While it can be a normal part of growing up, it can also be stressful and embarrassing for some children. Fortunately, parents can make several lifestyle changes to help reduce the frequency of bedwetting in their children. The infographic below lists a few strategies for you to consider. Illustration: Momjunction Design Team
Learn from the experts why children wet the bed even after five years of age and get tips to help stop bedwetting. Explore the answers you need to help your child stay dry at night.
References
1. Colleen Moriarty; Bedwetting and ‘Accidents’: Solutions for Children; Yale Medicine
2. T Gersa, A Seth and J Mathew; Nocturnal Enuresis In Children; The Internet Journal of Urology
3. Symptoms & Causes of Bladder Control Problems & Bedwetting in Children; National Institute of Diabetes and Digestive and Kidney Disease
4. Lower Urinary Tract Dysfunction; St. Louis Children’s Hospital
5. Rajiv Sinha and Sumantra Raut; Management of nocturnal enuresis – myths and facts; NCBI(2016)
6. Avinash De Sousa, Hema Kapoor, Jyoti Jagtap, and Mercilina Sen; Prevalence and factors affecting enuresis amongst primary school children; NCBI(2007)
7. Bedwetting; Cleveland Clinic
8. Enuresis in Children: A Case-Based Approach; AFP
9. Enuresis and Natural Treatment; International Medical University of Natural Education Offering Evidence Based Education and Int Licenses for Natural Minded Professionals
10. Ahmed Salih Sahib; Anti-diabetic and antioxidant effect of cinnamon in poorly controlled type-2 diabetic Iraqi patients: A randomized, placebo-controlled clinical trial; NCBI(2016)
11. Duane R Hickling, and Victor W Nitti; Management of Recurrent Urinary Tract Infections in Healthy Adult Women; NCBI(2013)
12. Hypercalciuria; Cincinnati Children’s Hospital
13. Talk about bedwetting; Bladder & Bowel, UK
14. Bedwetting: 3 Common Reasons & What Families Can Do; American Academy of Pediatrics
15. What Is Nocturnal Enuresis (Bedwetting)?; American Urological Foundation
16. Bedwetting in Children & Teens: Nocturnal Enuresis; American Academy of Pediatrics
17. Urinary Incontinence (Enuresis) in Children; University of Rochester Medical Center
18. Bedwetting (Enuresis); Johns Hopkins Medicine
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Atiqur Rahman Khan
Read full bio of Sagari Gongala
Read full bio of Swati Patwal
Read full bio of Apoorva K