Preseptal cellulitis or periorbital cellulitis in children is characterized by inflammation and infection of the soft tissues around the eyes. It can be due to bacteria and may occur in one or both eyes. The risk for severe complications is rare if it is treated appropriately. Improper treatment or a delay in treatment may complicate and cause intracranial infections, such as meningitisiInflammation of the protective layers and fluid surrounding the brain and spinal cord , or cause infection posterior to the orbital septum called orbital cellulitis (1).
Redness and swelling in the eye should be evaluated and treated by a pediatrician to avoid these complications. You may also ensure that the recommended medications and home care measures are followed to avoid recurrence.
Read on to learn more about the causes, symptoms, diagnosis, complications, treatment, and prevention of periorbital cellulitis in children.
Key Pointers
- Periorbital cellulitis is a common infection in children that affects the tissues surrounding the eyes.
- The infection is mainly caused by bacteria, but in rare cases, it can also be caused by fungi.
- The typical symptoms of periorbital cellulitis include fever, tenderness, warm and sore eyes.
- Treatment options for periorbital cellulitis include antibiotics, painkillers, and surgery.
- Prompt treatment of eye infections, management of open wounds, and getting prescribed vaccinations can help prevent periorbital cellulitis.
Causes Of Periorbital Cellulitis In Children

The most common bacteria that cause periorbital cellulitis are:
- Staphylococcus aureusi Commonly found bacteria responsible for acute skin and food-borne infections and boils
- Streptococcus pneumoniaeiPathogenic bacteria which is the causative agent of pneumonia and certain skin conditions
- Streptococcus pyogenes
- AnaerobesiUsually pathogenic bacterial species that possess the ability to thrive in the absence of oxygen
These bacteria may enter soft tissues around the eye through infected sinuses or breaks in the skin. Certain bacteria and fungi may also enter the soft tissues through abnormal bone septa or the bloodstream. Once the bacteria enter, they may quickly multiply and cause inflammation in the periorbital area, causing redness, pain, and warmth, among other symptoms (1).
In rare cases, fungi such as aspergillusiFungal genus that may infect the lungs and sinuses, leading to breathing troubles, cough, and fatigue or mucorales can cause periorbital cellulitis. The chances of infection due to Haemophilus influenzaei Pathogenic bacteria that may cause serious infections in young children have reduced recently due to flu vaccinations. According to the US Centers for Disease Control and Prevention (US CDC) the burden of H. influenzae disease declined by more than 99% compared to the prevaccine era in the US(13). However, there have been increased instances of periorbital cellulitis infection caused by the antibiotic-resistant MRSA (methicillin-resistant staphylococcus aureusiA group of gram-positive bacteria that have evolved genetically to develop defense mechanisms against antibiotics ) (1).
Risk Factors For Periorbital Cellulitis

The following infections or trauma could trigger periorbital cellulitis around the eyes (2):
- SinusitisiInflammation in the sinuses typically caused due to allergies or infection An ethmoid sinus infection is the most common way that the bacteria responsible for periorbital cellulitis may enter the tissues. These sinuses may also provide suitable conditions for the bacteria to multiply, allowing the infection to spread.
- Upper respiratory infection-In case of infections, the upper respiratory tract is predominantly colonized by Streptococcus pyogenes or pneumoniae. These bacteria can spread to surrounding mucosal tissues such as the sinuses and, in turn, cause periorbital and orbital cellulitis (14).
- ImpetigoiA type of bacterial skin infection that causes red blisters on the face that can burst, ooze fluid, and leave yellow crusts – Children with this severe bacterial infection may present with blisters on the face, including the eyelids and other areas surrounding the eyes. The bacteria from these blisters may infect the skin surrounding the eyes, causing inflammation and other symptoms that resemble periorbital cellulitis (15).
- A styeiA bacterial infection inside the eyelids that cause painful, red bumps typically filled with pus (lump on the eyelid) – Stye contains bacterial strains that are similar to those causing periorbital cellulitis. Recurring and unresolved styes can cause the tissues around the eyes to scar and weaken, making it easier for bacteria to colonize the area and cause inflammation (16).
- Swelling of the lacrimal (tear)- gland Acute dacryoadenitis caused by streptococcus and other bacteria can cause pain and inflammation in the tear ducts, causing further complications such as periorbital and orbital cellulitis (17).
- Insect bite – Insect bites cause openings and breaks in the skin that may get infected with strep bacteria when scratched repeatedly. It may allow the bacteria to colonize the tissues, causing inflammation, pain, and redness (18).
- Animal bite – Animal bites, especially those on the face, can disrupt the mucosal barrier and skin surrounding the eyes. It can cause openings for bacteria to enter and infect the region (19).
- Wound – Fresh and unhealed wounds offer the perfect openings for bacteria to enter. These may get into the veins and flow with the blood, reaching the periocular regions.
- Blood infection – In children with bacteremia and septicemia, the staphylococcus bacteria can enter the periocular region via the bloodstream, causing inflammation and discoloration.
- Weak immune system – Children who are immunocompromised or under five may be more susceptible to infectious diseases as their bodies struggle to prevent the bacteria causing periorbital cellulitis from entering or multiplying (10).
You may reduce the risk of periorbital cellulitis by following proper wound care and treating the skin or respiratory tract infections on time.
 Quick fact
Quick factSigns And Symptoms Of Periorbital Cellulitis In Children
The common signs and symptoms of periorbital cellulitis include (3):
- Erythema (redness of the skin). Skin is red and shiny.
- Swollen eye and eyelids
- Warmness over the eyes. Hot on touching
- Tender on touching
- Fever
- Eye pain
Seek medical attention if you notice these changes in and around your child’s eyes and the surrounding facial parts. Early diagnosis and treatment could increase the chances of cure and reduce the risk for complications.
 Do remember
Do rememberDiagnosis Of Periorbital Cellulitis In Children

An eye doctor may start the diagnosis by noting any recent infections or injuries and performing a physical examination. After examining your child’s eye, the doctor may recommend one of the following tests (4):
- Visual examination: The doctor may check your child’s visual acuity, eye muscle movements, and the intraocular pressure (pressure of the eye).
- Neurological examination: The pupil’s reaction to light and its accommodation is analyzed. Your doctor may also look for brain functions such as balance, coordination, etc., to ensure there are no intracranial complications.
- Blood tests: This may help to identify the bacteria and other inflammation and infection-related changes in the blood.
- Analysis of eye secretions: Secretion samples from the eye may help to identify the bacteria.
- Imaging: Magnetic resonance imaging (MRI) and computed tomography (CT) may be used to find a foreign object, rupture of the eye, or abscess in children.
In most cases, your doctor may recommend treatments after the clinical diagnosis. CT scans are usually ordered to rule out orbital cellulitis and identify intracranial complications. Blood tests are not always suggested since they can be negative in several cases.
 Experts say
Experts sayTreatment For Periorbital Cellulitis In Children

The treatment varies depending on the age of the child and the severity of the disease. However, two weeks of appropriate treatment can cure periorbital cellulitis.
In severe cases, children, especially those below one year of age, may require hospitalization. Hospitalization occurs to provide intravenous antibiotics and treat associated complications. Older children with mild infection can be treated with oral antibiotics in outpatient settings.
Barnaby Fry, a dad of two and blogger, shares how his son Joshua’s periorbital cellulitis was treated. He says, “Joshua was admitted and treated with intravenous antibiotics for three days. The poor mite kept having to be cannulated in almost every available vein as they were tiny, and the cannula kept coming out. This treatment killed all infections in his body and left him feeling much better, and the swelling around his eyes had reduced. Emma (my wife) stayed with him on Tuesday and Wednesday, and I stayed on Thursday. We returned home on Friday afternoon with a course of oral antibiotics, which Josh must take every eight hours. The last two days, he has laughed and smiled more than in the last two weeks (i).”
Your child’s pediatrician may recommend any of the medications listed below (1):
- Antibiotics: Antibiotics are given to inhibit the growth of bacteria. Usually, five to seven days of treatment with antibiotics such as clindamycin, TMP-SMX plus amoxicillin-clavulanic acid, or cefdinir is recommended. If cellulitis persists, an extended treatment is needed. Broad-spectrum antibiotics are given if your child is not vaccinated for the influenza virus.
- Acetaminophen: This is used to treat fever and pain. Although it is available over the counter, you may get a doctor’s prescription for exact dosing. An overdose of this drug could result in liver damage.
- NSAIDs (ibuprofen): This drug helps to reduce pain, swelling, and fever.
- Surgical drainage: If the cellulitis complicates into an abscess, your doctor may recommend surgery to drain the pus.
Most children show immediate responses to antibiotic treatment in outpatient settings. The condition is quite painful, and the child needs pain relievers and antibiotics to treat the infection and prevent complications. Follow-up care is essential for monitoring the child’s recovery. Parents should watch for any recurring symptoms and communicate with their healthcare provider. If no signs of improvement occur within one or two days, your child may need hospitalization and further treatments.
Tips To Prevent Periorbital Cellulitis In Children

The following tips may help to prevent periorbital or preseptal cellulitis in children (5):
- Follow good hygiene practices.
- Protect your child with safety equipment while playing sports, skating, and gardening.
- Dress the child in full-sleeved shirts and long pants to prevent insect bites when they go out to play.
- If they have any wounds, keep them clean.
- You may use antibiotic ointments on injuries to prevent contamination.
- Do not let them swim if they have a wound.
- Give the recommended vaccinations on time.
- Get the early eye infections treated.
- Instruct your child not to rub infected eyes.
- Cut the nails of the child regularly, so that they do not scratch infected boils on skin and then rub the eye.
- Treat insect bites urgently.
- Seek immediate medical care in case of animal bites and deep puncture wounds.
The Hib and pneumococcal vaccines may help to prevent periorbital cellulitis in children. You may also take care of any injuries on your child’s skin. Recurrence and complications of periorbital cellulitis can be restricted by following the prescribed course of medications.
When To See A Doctor
You should contact your child’s healthcare provider if you have any concerns about the condition or if you notice the following (6):
- Red and swollen eyes
- Pus draining from the eyes
- Fever
- Chills
- Red streaks on the infected area of the skin
Sometimes, periorbital cellulitis may lead to emergencies. You may call emergency if you notice any of the following in your child:
- Difficulty in breathing
- Seizure
- Drowsiness
- Trouble waking up from sleep
You may seek an immediate medical consultation if your child has:
- Stiff neck
- Headache
- Vomiting
- Blurred vision
- Diplopia (double vision)
- Sensitivity to bright light
- Bulging of the eye
The above indicate intracranial complications. Although it is not a severe condition, following a proper treatment plan could prevent intracranial complications, which may be fatal. Untreated periorbital cellulitis can also lead to vision loss. Give the full course of antibiotics.
Frequently Asked Questions
1. How serious is periorbital cellulitis?
Periorbital cellulitis usually improves with treatment. Rarely, especially if left untreated, the infection around the eye can spread to the eye, resulting in orbital cellulitis and potentially causing vision problems (7).
2. Can periorbital cellulitis spread to the brain?
If periorbital cellulitis develops into orbital cellulitis, there is an increased risk of spread to the brain. Since the eyes are connected to the brain through optic nerves, orbital cellulitis can cause brain abscess and vision loss and be severe in some cases (8).
3. Does poor hygiene cause periorbital cellulitis?
Periorbital cellulitis is not caused by poor hygiene in children. It may spread through the venous system of the eye during sinusitis or other upper airway infections (9).
4. How long does periorbital cellulitis take to heal?
The exact healing time for periorbital cellulitis may vary in children. Usually, most children feel better within 24 to 48 hours after taking antibiotics, and it usually resolves within five to seven days of antibiotic therapy (9).
5. Will periorbital cellulitis go away without antibiotics?
Antibiotics are the principal treatment for periorbital cellulitis and are recommended to prevent complications. Early diagnosis and treatments can improve outcomes in most cases (9). Mild cases can be treated at home with oral antibiotics, and severe cases may require hospitalization and intravenous (IV) antibiotic therapies.
6. What is the difference between periorbital and orbital cellulitis?
Orbital cellulitis is a bacterial infection that affects muscle and fat. However, periorbital cellulitis is the infection of the eyelids or the area surrounding the eyes and does not affect the orbit. In addition, unlike periorbital cellulitis, orbital cellulitis is rare and affects the deeper tissues of the eyes, potentially causing long-term visual damage (10).
7. Why does my child keep getting periorbital cellulitis?
Recurrent periorbital cellulitis is rare and may develop as a side effect of paranasal sinus infection, tooth infection, eyelid trauma, or external ocular infection (11).
8. What mimics periorbital cellulitis?
Conditions such as hordeolum (bacterial infection on the eyelid), dacryocystitis (tear sac inflammation), and pink eye(conjunctivitis) in kids may mimic the symptoms of periorbital cellulitis(12).
Periorbital cellulitis in children can be managed with proper care, timely diagnosis, and treatment. It is crucial you are aware of the common symptoms such as skin redness, fever, warm eyes, and swollen eyelids in children. Although most of the time, a course of antibiotics is suggested as the first form of treatment depending upon the severity and age of the child, surgical intervention or other treatments may be adopted in case of complications. So, it is recommended to stay alert and follow preventive measures to minimize the risks of periorbital cellulitis in children.
Infographic: What Happens If Periorbital Cellulitis In Children Goes Untreated?
Untreated or inadequately treated periorbital cellulitis can spread to the orbit and other structures. This may lead to loss of function and other complications depending on the affected eye or brain area. Go through the infographic to know the common complications of periorbital cellulitis. Illustration: Momjunction Design Team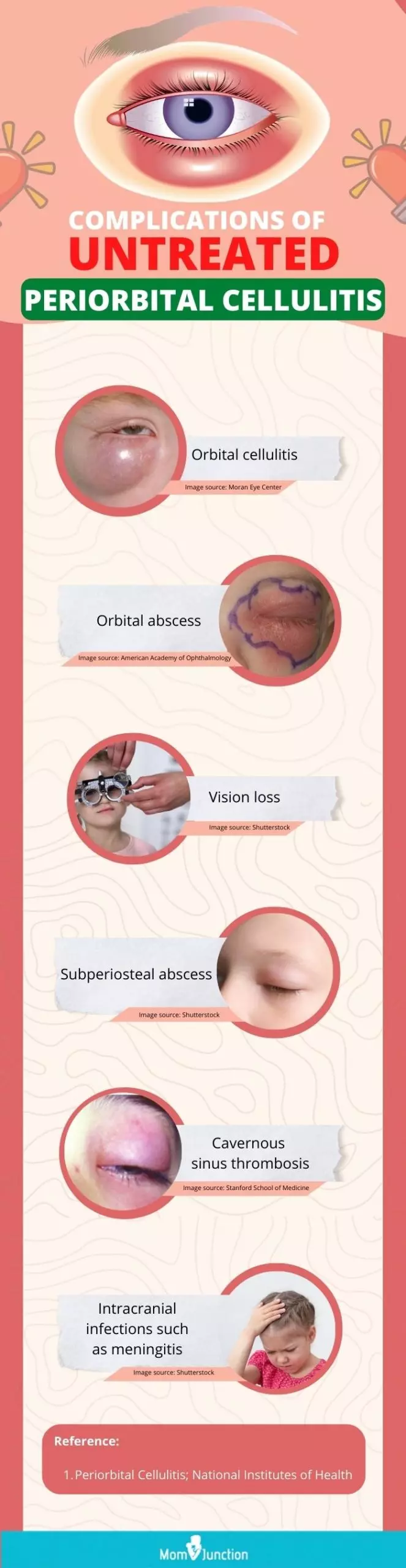
Watch this informative video to learn how to recognize and treat periorbital cellulitis quickly to avoid serious complications.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Little wounded soldier;https://barnabyfry.wordpress.com/2006/11/
References
1. Crystal Bae and Daniele Bourget.; Periorbital cellulitis; StatPearls Publishing (2020).
2. Seongmu Lee and Michael T. Yen; Management of preseptal and orbital cellulitis; Saudi Journal of Ophthalmology (2011).
3. Periorbital cellulitis; The United States National Library of Medicine
4. Robert Thomas Carlisle and John Digovanni; Differential Diagnosis Of The Swollen Red Eyelid; American Family Physician (2015).
5. Cellulitis; Harvard Health Publishing; Harvard School of Medicine
6. Cellulitis of the eye in children; University of Rochester Medical Center (URMC)
7. Periorbital Cellulitis; Mount Sinai
8. Periorbital And Orbital Cellulitis; JAMA Network
9. Crystal Ba And Daniele Bourget; Periorbital Cellulitis; National Library of Medicine (2021)
10. Periorbital Cellulitis; Cleveland Clinic
11. J A Gomez Campdera et al.; Orbital and periorbital cellulitis in childhood. A review of 116 cases; NIH (1996)
12. Ellan R Wald; Periorbital (preseptal) cellulitis in children; Taylor and Francis Online (2014) 13. Chapter 8: Haemophilus influenzae; Centers for Disease Control and Prevention
14. Orbital Cellulitis; American Academy of Opthamology
15. Philumena Chen e al.; Preseptal Cellulitis Due To Impetigo – A Case Report Of Uncommon Presentation In Pakistan; Journal Of Ayub Medical College Abbottabad (2023)
16. Davis Willmann et al.; Hordeolum (Stye); StatPearls Publishing 17. Dacryoadenitis; CMount Sinai
18. Cellulitis From a Bug Bite; Cleveland Clinic
19. 20: Orbital and Periorbital Cellulitis; American Academy of Pediatrics
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Mubina Agboatwalla
Read full bio of Dr Bisny T. Joseph
Read full bio of Swati Patwal
Read full bio of Anindita Ghatak