Image: iStock
Fetal alcohol syndrome (FAS) is a severe form of fetal alcohol spectrum disorder (FASD) seen in babies born to mothers who drink during pregnancy. This condition is caused by the consumption of any type and amount of alcohol. It may have teratogenic effects causing permanent brain damage and growth problems in babies. According to the US Centers for Disease Control and Prevention (CDC), 0.2 to 1.5 infants in every 1,000 live births are identified with FAS in certain areas of the US(1). Hence, the CDC recommends that all women planning to conceive should avoid alcohol consumption in any form when they stop using birth control methods to prevent alcohol-related health complications for the baby (2).
Learn more about the risk factors, symptoms, possible complications, diagnosis, treatment, and prevention of fetal alcohol syndrome.
Key Pointers
- Drinking alcohol during pregnancy could affect fetal development, causing fetal alcohol syndrome (FAS).
- Babies who come in contact with alcohol during pregnancy may be born with smaller heads and vision or hearing problems.
- Since FAS is permanent, consult a doctor if you have had alcohol, tobacco, or drugs during pregnancy.
- Medical professionals may suggest medications or behavioral therapy for babies with FAS.
Risk Factors And Causes Of Fetal Alcohol Syndrome
Consumption of alcohol during pregnancy causes fetal alcohol syndrome. Even small amounts of alcohol can reach the fetus through the placenta. Alcohol could damage an unborn baby’s brain and other organs and harm their growth since their liver is not completely developed to process alcohol (3).
Binge drinking, i.e., consuming three or more drinks at a time, can have teratogenic effects on the baby. This can cause high alcohol levels in pregnant mothers and their baby’s blood. The National Survey on Drug Use and Health (NSDUH) (2021) reported that about 4.3% of pregnant women indulged in binge drinking. Although you may not drink every day, binge drinking at once can cause FAS in babies (4).
Dr. Anne Schuchat, Former Rear Admiral And Assistant Surgeon General In The US Public Health Service Commissioned Corps And US CDC’s Principal Deputy Director, says, “Alcohol can permanently harm a developing baby before a woman knows she is pregnant” (2).
Drinking alcohol in the first trimester is more harmful since this is the time when the fetus begins to develop the brain and other organs. Birth defects are common among babies born to mothers who drink during the first three months of pregnancy. However, maternal drinking can harm the unborn baby (4).

Image: Shutterstock
Signs And Symptoms Of Fetal Alcohol Syndrome
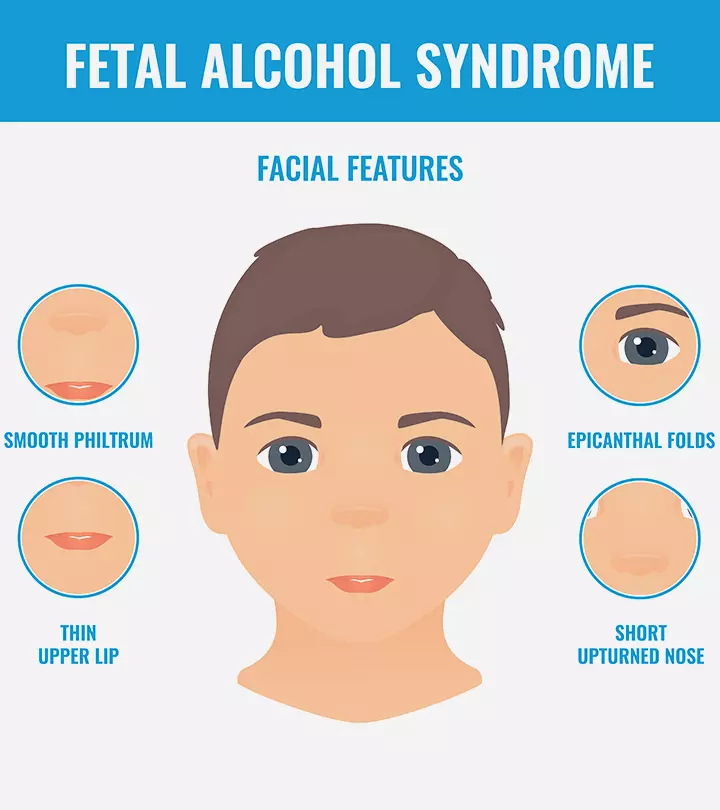
The following signs and symptoms may indicate fetal alcohol syndrome in babies (5):
- Smaller head than average
- Specific facial features such as thin upper lips, small eyes, the smooth area between the upper lip and nose may become less noticeable with age (indistinct philtrum)
- Vision problems
- Hearing problems
- Balance and movement issues
- Attention and concentration problems
- Hyperactivity
- Learning difficulties such as troubles with social skills, thinking, time management, mathematics, memory, and speech
- Damage to kidney, liver, heart, and other organs
The severity of symptoms may vary in each baby. However, all these problems are permanent. Treatment can help limit the impact of these conditions on a child’s life.
 Point to consider
Point to considerSigns To See A Doctor

Image: Shutterstock
Contact your doctor if you suspect FAS in your baby. Early diagnosis and interventions help improve the quality of life in children. Seek medical care if you are pregnant or planning pregnancy and cannot stop drinking.
You may inform the pediatrician if you were consuming alcohol during pregnancy for early diagnosis. Do not wait for the onset of symptoms to seek medical help (6).
Complications Of Fetal Alcohol Syndrome
The severity of FAS complications in babies may range from mild to severe disabilities.
For example, some babies may develop mild learning disabilities, while others may have severe mental and behavioral problems (3).
Long-term complications or secondary disabilities of fetal alcohol syndrome that are latent at birth may include (6):
- Mental health disorders such as eating disorders, anxiety disorders, and depression
- Attention deficit hyperactivity disorder (ADHDiA neurodevelopmental condition characterized by the inability to focus, hyperactivity, and impulsiveness. )
- Drug and alcohol misuse
- Inappropriate social conduct such as breaking the rules and laws (criminal behavior)
- Aggression
- Unable to live independently
- Not completing school or a decline in academic performance

Image: Shutterstock
- Unemployment
- Poor social skills
- Problematic sexual behaviors
- Increased risk of suicide, homicide, and accidents
These complications can be due to underlying neurodevelopmental disorders. However, many children who receive the right support and therapies can overcome these defects and have a better quality of life.
Diagnosis Of Fetal Alcohol Syndrome
FAS is diagnosed based on the symptoms present and does not require documentation of prenatal exposure to alcohol. Pediatricians may refer the child to specialists such as pediatric neurologists for definite diagnosis since drugs, tobacco, and other substances can also cause symptoms similar to fetal alcohol spectrum disorders (FASD)
(7).
The presence of all the following conditions can help diagnose fetal alcohol syndrome (7):
- Facial features including smooth philtrum, short palpebral fissure (distance between the inner and outer corner of the eye), thin vermillion border (demarcation between lip and skin)
- Prenatal or postnatal growth retardation
- Developmental delays, including poor motor coordination, difficulties with self-regulation, daily living skills, and relationships.
- Central nervous system defects
If only two features are met, partial fetal alcohol syndrome (pFAS) is confirmed. Some babies can have alcohol-related birth defects (ARBD), which are birth defects secondary to fetal alcohol exposure without neurobehavioral or cognitive impairments. Some may have the alcohol-related neurodevelopmental disorder (ARND) with neurodevelopmental issues and no physical defects.
Treatment For Fetal Alcohol Syndrome
There is no cure for FAS. Central nervous system damages due to prenatal alcohol exposure are permanent. The treatment strategies are tailored to address alcohol-related birth defects and developmental disabilities in each child with specific therapies (7).
The following treatments are generally given for children with alcohol spectrum disorders (8):
- Medical care for babies with alcohol disorders is the same as for other babies. They also need well-baby visits, childhood vaccinations, nutrition, and other basic medical care.
- Behavioral and educational therapy, including good buddies (friendship training) to teach social skills, math interactive learning experience (MILE) to tackle mathematic troubles, families moving forward (FMF) training to support families together (PACT) training to enhance executive function and self-regulation are usually recommended for children with FASDs.
- Alternative approaches such as massages, yoga, exercises, relaxation therapies, auditory therapy, and vitamin supplements are often used. However, it is recommended to seek a doctor’s advice before taking alternative treatments.

Image: Shutterstock
- Medications such as antidepressants, neurolepticsiMedication used to treat mental ailments that works by stopping dopamine receptors in the nervous system. , stimulants, and anti-anxiety drugs are often prescribed based on the symptoms. Some children may respond well to medications, while a few may not.
- Parent training is often required for children with FAS since the child may not respond to usual parenting strategies. This training helps the parent teach the child to cope with their problems and improve skills.
Neurocognitive therapiesiTherapeutic training addressing neurological disorders to promote the development of higher cognitive abilities. and other therapies help improve the quality of a child’s life. However, as for many other diseases, prevention is the only cure for FAS.
Prevention Of Fetal Alcohol Syndrome

Image: Shutterstock
FAS is completely preventable if pregnant mothers abstain from alcohol (9). You should stop alcohol consumption before becoming pregnant and throughout pregnancy. It is advised to avoid all alcoholic beverages, including wine, beer, and low alcohol drinks, during pregnancy.
“About half of all pregnancies in the United States are unplanned, and even if planned, most women won’t know they are pregnant for the first month or so when they might still be drinking. The risk is real. Why take the chance? (2)” says Dr. Schuchat.
All sexually active women are advised to abstain from alcohol if they are not using effective contraception (birth control) measures. Usually, it may take four to six weeks for a mother to know about her pregnancy, and exposure to alcohol during this time can cause FASDs. Learning about the risks of alcohol before conception can help reduce FAS incidence. However, it is never too late for a pregnant mom to stop drinking since brain development happens throughout the pregnancy. The earlier you stop, the better the outcomes (3).
 Point to consider
Point to considerFrequently Asked Questions
1. Can one see fetal alcohol syndrome in an ultrasound?
Yes, ultrasound may help detect certain facial anomalies and neurobehavioral factors associated with fetal alcohol syndrome. However, ultrasound may not be taken as the sole diagnosis for measurement of the fetal effects and can be paired with other tests and scans, such as an anomaly scan, for better diagnosis (10).
2. How long does alcohol stay in a fetus’s system?
The exact lasting period of alcohol in the fetal system may not be possible to state since its elimination from the baby’s body depends on the metabolizing capacity of the mother. It has been shown that alcohol may remain for longer periods in the fetal body even after its elimination from the mother’s system, and it may only be eliminated from the baby’s body by diffusing it back to the mother’s system through the placenta (11) (12).
3. Which organ of the fetus usually suffers most from alcohol abuse?
The fetus’s brain is the most impacted during fetal alcohol exposure (13). According to studies, the hippocampusiA brain structure within the temporal lobe related to learning and memory functions. and prefrontal cortexiA region of the brain in the frontal lobe that influences attention, manages emotions, and coordinates complex behaviors. of the brain may be most affected by FAS and can reduce the ability of the brain to process information and affect the overall functioning of the brain (14).
Consumption of alcohol during pregnancy may cause fetal alcohol syndrome (FAS). Further, the severity of the symptoms of FAS may vary with each baby. Hence, to prevent complications, alcohol consumption should be avoided during pregnancy and immediately after stopping any birth control methods. If you have consumed alcohol during pregnancy, inform your doctor. The treatment may vary based on the baby’s symptoms. Fortunately, early diagnosis and treatment of FAS may alleviate any complications. If you are trying to conceive but unable to abstain from drinking, consider seeking the help of a therapist.
Infographic: How Does Fetal Alcohol Syndrome Affect The Child?
Fetal alcohol syndrome is one of the major complications of maternal alcohol consumption during pregnancy. The syndrome can cause long-term problems in the child, including facial abnormalities to hearing and speech problems. The infographic below enlists some long-term effects of this condition among children.

Illustration: Momjunction Design Team
Illustration: Fetal Alcohol Syndrome (FAS) Causes Symptoms And Treatment

Image: Dall·E/MomJunction Design Team
Fetal alcohol syndrome is a fetal condition caused when pregnant women take alcohol during pregnancy. This informative video provides valuable insights into its causes, signs, diagnosis, and treatment.
References
- Data and Statistics on FASDs.
https://www.cdc.gov/fasd/data/?CDC_AAref_Val=https://www.cdc.gov/fasd/data/?CDC_AAref_Val=https://www.cdc.gov/ncbddd/fasd/data.html - More than 3 million US women at risk for alcohol-exposed pregnancy.
https://archive.cdc.gov/#/details?url=https://archive.cdc.gov/#/details?url=https://www.cdc.gov/media/releases/2016/p0202-alcohol-exposed-pregnancy.html - Fetal Alcohol Spectrum Disorders (FASD).
https://www.cedars-sinai.org/health-library/diseases-and-conditions—pediatrics/f/fetal-alcohol-spectrum-disorder-fasd.html - Fetal Alcohol Syndrome.
https://familydoctor.org/condition/fetal-alcohol-spectrum-disorders-fasd - Fetal Alcohol Syndrome.
https://www.nhs.uk/conditions/fetal-alcohol-spectrum-disorder/ - Fetal Alcohol Syndrome.
https://www.stclair.org/services/mayo-clinic-health-information/diseases-and-conditions/CON-20306118/ - Demetrios Vorgias and Bettina Bernstein; Fetal Alcohol Syndrome.
https://www.ncbi.nlm.nih.gov/books/NBK448178/ - Types of Treatment for FASDs.
https://www.cdc.gov/fasd/treatment/types.html - Fetal Alcohol Syndrome (FAS).
https://childrenswi.org/medical-care/genetics-and-genomics-program/medical-genetics/teratogens/fetal-alcohol-syndrome-fas - Annika C Montag et al. (2016); Second Trimester Ultrasound as a Tool for Early Detection of Fetal Alcohol Spectrum Disorders (FASD).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5104277/ - L Burd et al. (2012); Prenatal alcohol exposure blood alcohol concentrations and alcohol elimination rates for the mother fetus and newborn.
https://pubmed.ncbi.nlm.nih.gov/22595965/ - Content: How Does Alcohol Get to the Fetus?
https://sites.duke.edu/apep/module-5-alcohol-and-babies/content-how-does-alcohol-get-to-the-fetus/ - Courtney Caputo et al. (2016); Impact of fetal alcohol exposure on body systems: A systematic review.
https://pubmed.ncbi.nlm.nih.gov/27297122/ - Peter G Hepper et al. (2012); Fetal brain function in response to maternal alcohol consumption: Early evidence of damage.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3521078/ - Fetal Alcohol Syndrome (FAS): Symptom, Causes, Treatment.
https://my.clevelandclinic.org/health/diseases/15677-fetal-alcohol-syndrome#symptoms-and-causes
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Mona Hardas
Read full bio of Dr Bisny T. Joseph
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das