Image: iStock
FPIES, or Food Protein-Induced Enterocolitis Syndrome, is a rare and potentially severe food allergy. It primarily affects infants and generally starts after four months and within the first year of life (1) (2). While the exact causes of FPIES in babies are not well understood, it may be due to an immune reaction to specific proteins in food and can lead to gastrointestinal symptomsiSymptoms related to health problems affecting the gastrointestinal tract that runs from the mouth to the rectum (3) (4). This post discusses the causes, symptoms, and treatment options for FPIES in babies, including strategies to help parents and caregivers better understand and manage this condition.
Key Pointers
- FPIES is a non-IgE-induced allergic reaction in infants within the first year of life that causes the body to react to a food protein.
- The typical food triggers are cow’s milk, soy, oats, and rice, but they may also include chicken, barley, potatoes, and fruits.
- The most effective treatment is completely removing the trigger foods until the baby is no longer sensitive to them.
- The child may outgrow the condition, but it is essential to be mindful of the symptoms to help prevent shock.
How Common Is FPIES?
FPIES is not among the common food allergies in babies, with an occurrence rate of only 0.51% in infants in the US
(5). Thus, given its rarity, you should learn how to spot the signs and care for children with this condition.
What Are The Symptoms Of FPIES In Babies?

The symptoms of FPIES allergy typically present two to four hours after ingestion of the trigger food (6). These symptoms may differ in severity and from child to child (7) (6):
- Severe or projectile vomitingiA forceful vomiting where the stomach contents eject at a distance from the body
- Dehydration
- Diarrhea
- Pale appearance
- Lack of energy
- Excessive drop in blood pressure (rare)
Children with chronic or multiple FPIES episodes may experience (4):
- Failure to gain age-appropriate weight
- Weight loss
Parents should monitor symptoms for a few hours after exposure to trigger foods to identify allergens and better manage the child’s diet.
 Be watchful
Be watchfulWhat Causes FPIES In Babies?
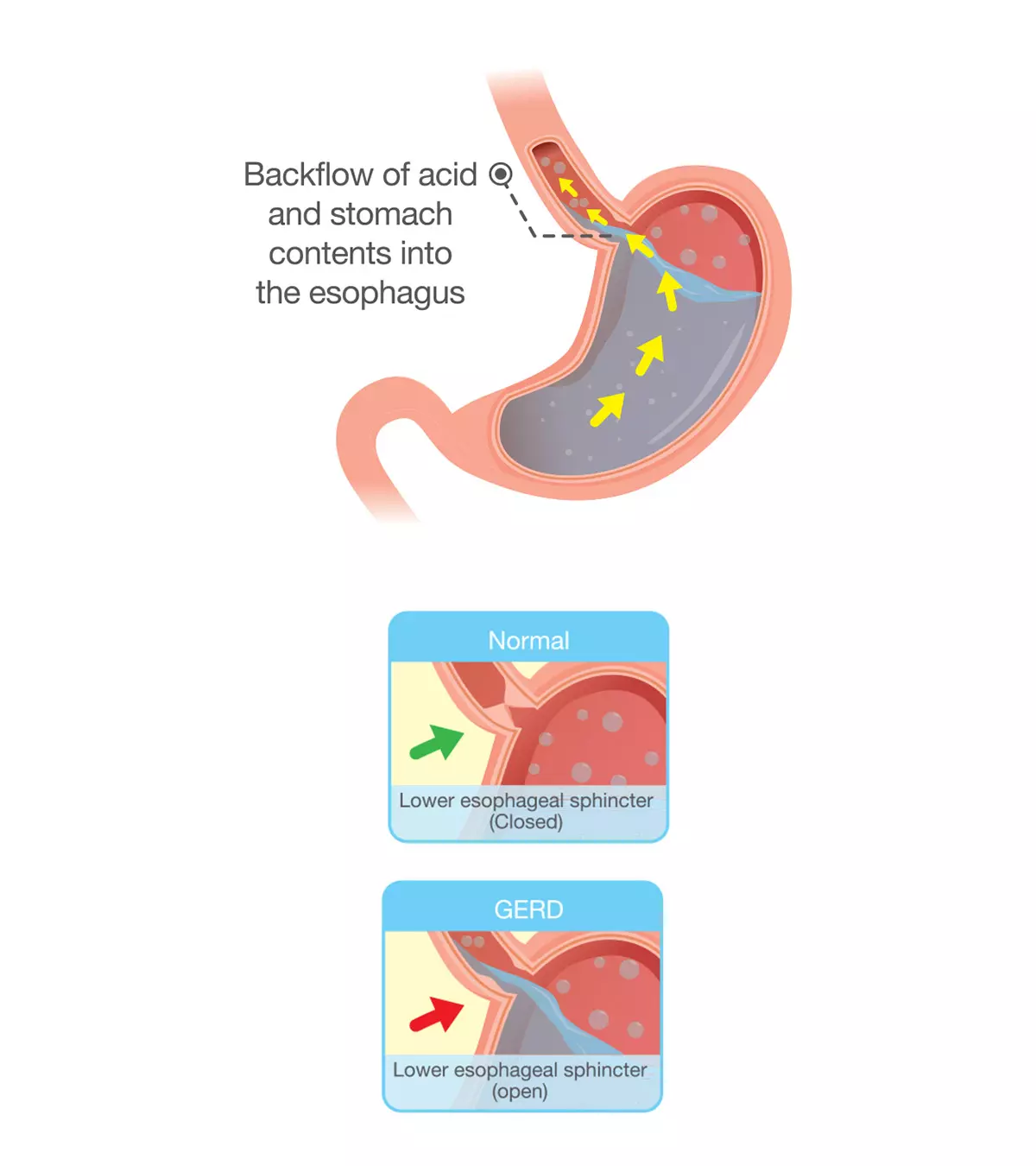
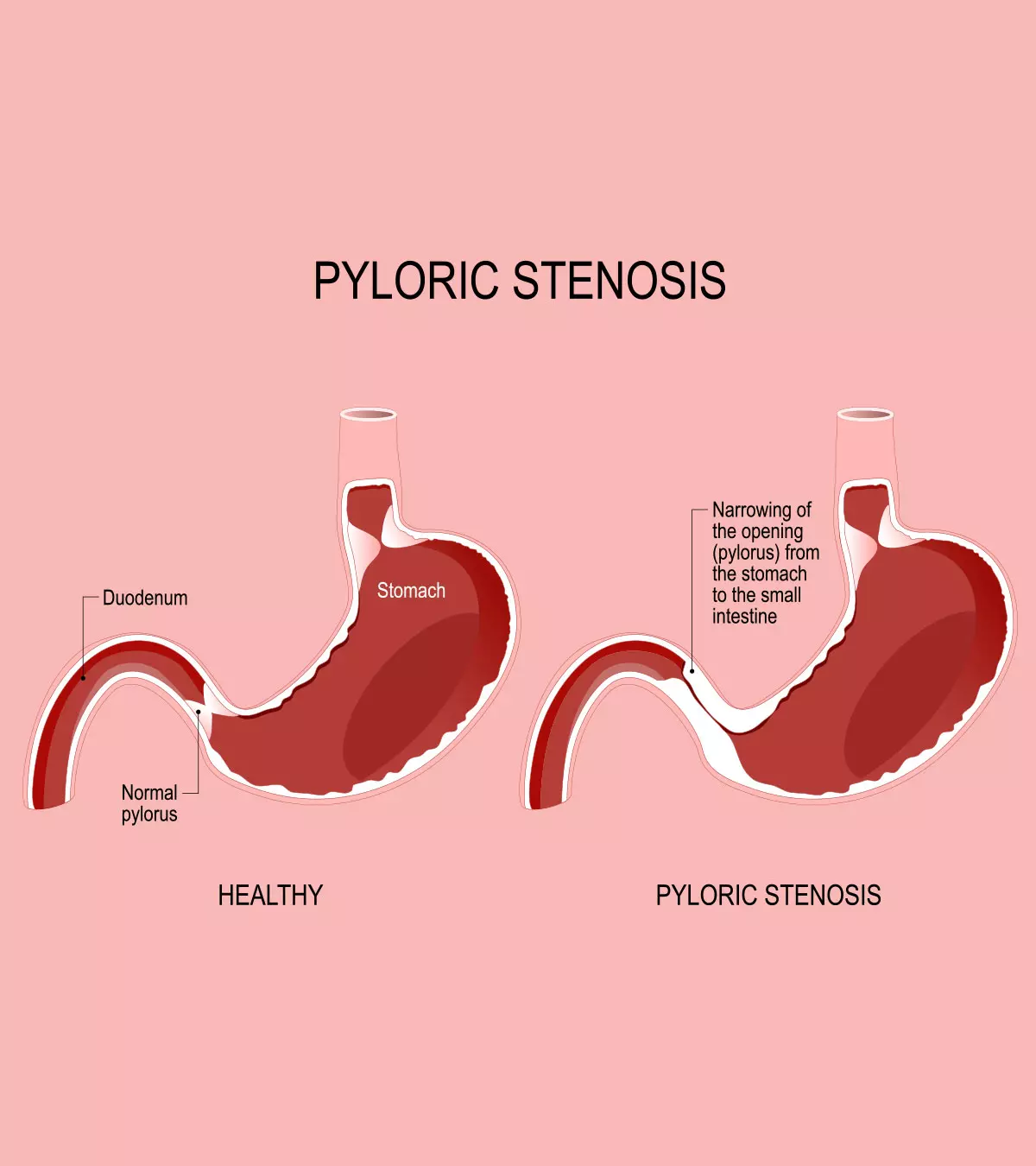
The exact mechanism behind FPIES is not well-understood. However, it is believed to be a non-IgEiImmunoglobulin E is a type of antibody that causes an allergic reaction when a foreign particle enters the body -induced allergic reaction, making the body react to a specific protein in food. This improper immune reaction causes inflammation in the small and large intestines allowing fluid to pass through the intestinal wall into the gut lumen. This fluid shift can lead to symptoms such as vomiting and diarrhea (2) (3).
What Are The Risk Factors For FPIES In Babies?
FPIES may affect anyone, and some factors put babies at an increased risk (8) (3):
- The incidence of FPIES is more in males than in females.
- 40 to 80% of the FPIES cases appear in infants with a family history of atopic diseasesiA genetic condition where the body reacts to environmental substances and produces an allergic reaction .
- FPIES may be more prolonged in infants if it develops with an IgE-mediated food allergy. Such cases are called “atypical FPIES.”
Which Foods Can Trigger FPIES in Babies?

Although any food may cause FPIES, the common triggers are cow’s milk, oats, soy, and rice. Since the child must directly consume the allergen for a reaction to occur, formula-fed infants are more likely to experience the symptoms than breastfed babies. However, breastfed babies may sometimes show mild sensitivity to certain foods in the maternal diet (7).
Jess, a mother of three, shares her baby Emma’s struggle with FPIES. She says, “I mixed oatmeal and pumped breast milk, and gave a couple of spoonfuls of the mixture to Emma… Exactly two hours later, Emma was a wreck. She vomited every five minutes for the next two hours and was quite lethargic. I had a hard time arousing her, but figured that vomiting was pretty exhausting, especially for a 5 1/2-month-old… Fast forward to two weeks later, we tried again. This time, I told myself I would be super smart and only give her a teaspoon since I had overfed her last time. Exactly two hours later, she had an even worse reaction… One lengthy Google search for me, and another Google search for my super experienced pediatrician, and he came up with a diagnosis of FPIES (i).”
Other food intolerance triggers include (5):
- Barley
- Chicken, turkey, and egg white
- Sweet or white potato and green pea
- Fruits
- Fish and mollusks
- Peanuts
- Shellfish
- Wheat
- Corn
How Is FPIES Diagnosed?

The standard IgE-targeted skin prick and blood tests are usually negative for FPIES. Thus, the doctor may thoroughly assess the child’s medical history, evaluate the symptoms, and exclude all the potential causes of other allergic reactions to learn the exact reason behind the condition (1) (7).
Additionally, a “supervised oral food challenge test” may be conducted with common trigger foods while monitoring the child’s response (7).
Given the nature of FPIES, parents may need to keep a detailed food diary to identify triggers and assist in the diagnostic process.
How Is FPIES Treated And Managed?
After diagnosis, based on the symptoms, their severity, and the causative agents, FPIES may be treated or managed in the following ways (7):
1. Changes in the eating habits
- Completely avoiding the foods causing triggers.
- Replacing ingredients in case of sensitivity to soy and dairy-based infant formulas.
- Switching to exclusive breastfeeding in case of cow’s milk sensitivity in babies less than six months.
2. Medical treatment

- Steroids to reduce the intensity of immune reactions. They will bring down the response but will not treat the condition completely.
- Administration of intravenous fluids to replenish the water lost during vomiting and dehydration in case of severe condition.
The child may be monitored for improvement throughout the treatment, and the doctor may instruct to reintroduce the trigger foods or introduce new foods if they feel the child has outgrown the condition (9).
 Point to consider
Point to considerWhat Is The Outlook For A Child With FPIES?
FPIES is not permanent; about 60 to 90% of children outgrow it by three years(5)
. However, some may experience symptoms past their adolescent stage. Nevertheless, the prognosis for FPIES in babies looks good, with children achieving stable and healthy growth with proper nutrition and timely management (7).
 Quick fact
Quick factWhen To See A Doctor For FPIES In Babies?
Besides being mindful of the other symptoms of FPIES, if the child experiences changes in their body temperature, or decreased urine output, you should take them to the hospital promptly to help prevent the risk of shock (7).
Frequently Asked Questions
1. Is it possible to have FPIES to more than one food?
Yes. Babies with FPIES may react to one, two, or multiple foods (10).
2. How is FPIES different from many common food allergies?
The difference between FPIES and common food allergies are (10):
- A typical food allergy reaction occurs within minutes of ingesting the trigger food, whereas an FPIES reaction takes hours.
- A food allergic reaction is caused by IgE antibodies, whereas FPIES is a non-IgE-mediated response.
3. What are low-risk foods for FPIES?
Children with FPIES may be fed low-risk foods, such as lamb, prunes, broccoli, fortifiediA food with added nutrients that are not typically present in it quinoa, and millet (11).
The delayed onset of FPIES symptoms, such as vomiting, diarrhea, and dehydration, makes it challenging. It is essential for parents and caregivers to be aware of the signs and symptoms of FPIES in babies and to work closely with a healthcare provider to determine the best course of treatment. This may include an elimination diet and carefully monitoring the child’s response to reintroduced foods. With proper management, children affected with FPIES can have a healthy and stable life.
Infographic: What You Should Know About FPIES In Babies
FPIES is not a typical food allergy and may often be misdiagnosed. Hence, parents and caregivers should be aware of the symptoms and understand its diagnosis and treatment methods. This infographic gives an overview of all the essential information about the condition. So, save it for easy access.

Illustration: Momjunction Design Team
Illustration: FPIES in Babies: Symptoms Causes And Treatment

Image: Stable Diffusion/MomJunction Design Team
FPIES is a rare food allergy that requires proper care. Learn about the symptoms, diagnosis, and treatment options available with this informative video.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. An adventure in FPIES.https://thatmillennialmommablog.com/motherhood/2018/8/14/an-adventure-in-fpies
References
- Food Protein-Induced Enterocolitis Syndrome (FPIES).
https://acaai.org/allergies/allergic-conditions/food/food-protein-induced-enterocolitis-syndrome-fpies/ - Francesco Baldo et al.; (2020); FPIES in exclusively breastfed infants: two case reports and review of the literature.
https://ijponline.biomedcentral.com/articles/10.1186/s13052-020-00910-8 - Food Protein-Induced Enterocolitis Syndrome; Causes.
https://rarediseases.org/rare-diseases/food-protein-induced-enterocolitis-syndrome/ - Food Protein-Induced Enterocolitis Syndrome; Signs & Symptoms.
https://rarediseases.org/rare-diseases/food-protein-induced-enterocolitis-syndrome/?filter=Signs+%26+Symptoms - Food Allergies and Intolerances in Newborns and Infants.
https://www.aap.org/en/patient-care/newborn-and-infant-nutrition/food-allergies-and-intolerances-in-newborns-and-infants/ - INTRODUCING FOOD TO THE INFANT WITH FPIES.
https://www.chla.org/sites/default/files/atoms/files/CHLA-FPIES-Infant-Food-Introduction.pdf - Food Protein-Induced Enterocolitis Syndrome (FPIES).
https://www.chop.edu/conditions-diseases/food-protein-induced-enterocolitis-syndrome-fpies#:~:text=If%20a%20child%20experiences%20ais%20intravenous%20fluids%20for%20rehydration. - Food Protein-Induced Enterocolitis Syndrome; Affected Populations.
https://rarediseases.org/rare-diseases/food-protein-induced-enterocolitis-syndrome/?filter=Affected+Populations - Food Protein-Induced Enterocolitis Syndrome; Standard Therapies.
https://rarediseases.org/rare-diseases/food-protein-induced-enterocolitis-syndrome/?filter=Standard+Therapies - Food Protein-Induced Enterocolitis Syndrome (FPIES).
https://www.aaaai.org/tools-for-the-public/conditions-library/allergies/food-protein-induced-enterocolitis-syndrome-fpies - Marion Groetch et al.; (2020); Dietary management of food protein–induced enterocolitis syndrome during the coronavirus disease 2019 pandemic.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7202833/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Anuradha Bansal
- Julianna Coughlin did her graduation in Nutrition and Dietetics at Framingham State University and post graduation at the University of Nebraska Lincoln. Julianna has five years of experience as a dietitian in long-term care and strives to provide the best nutrition care to her clients.
 Julianna Coughlin did her graduation in Nutrition and Dietetics at Framingham State University and post graduation at the University of Nebraska Lincoln. Julianna has five years of experience as a dietitian in long-term care and strives to provide the best nutrition care to her clients.
Julianna Coughlin did her graduation in Nutrition and Dietetics at Framingham State University and post graduation at the University of Nebraska Lincoln. Julianna has five years of experience as a dietitian in long-term care and strives to provide the best nutrition care to her clients.
Read full bio of Aneesha Amonz
Read full bio of Rohit Garoo
Read full bio of Anindita Ghatak