
Image: Shutterstock
Fungi are naturally present on soil, animals, plants, indoor items, and even human bodies (1). Despite being present everywhere, human beings do not easily get fungal infections due to multiple levels of immune defenses. However, it is also possible to see fungal infections in babies. These are more common in neonatesiA child under 28 days of age. and infants, especially premature babies, due to their underdeveloped immune systems. Fungi have several forms, but yeast, mold, and dimorphs are the three most prominent types. Read this post to know more about the prevalence, types, risk factors, causes, symptoms, diagnosis, treatment, home remedies, and prevention of fungal infections in babies.
Key Pointers
- Babies have weakly developed immune systems, making them more susceptible to fungal infections.
- Fungal infections can be acquired through direct exposure to an infected person or fungal species.
- Babies born in a humid environment or suffering from malnutrition are at higher risk of getting fungal infections.
- Keeping a clean environment, changing diapers daily, and regularly screening pets for infections can lower the chances of infection.
- Topical medication should only be used for treatment after consulting with a doctor.
Are Fungal Infections Common In Babies And Toddlers?
Infantile fungal infection is more common because infants’ immune system is still developing and not robust enough to fight the infections in general.
A majority of children, at least at one point, will obtain some form of fungal infection.
 Did you know?
Did you know?What Are The Risk Factors Associated With Fungal Infection?
The following are some of the risk factors for fungal infection in babies (2) (3) (4) (5) (6) (7) (8) (9):
- Malnourishment
- Warm or humid climate
- Close proximity to pets, farm animals, and stray animals
- Babies hospitalized for a prolonged period of time

Image: IStock
- Babies born with a birth weight of less than 1,500g
- Babies born prematurely
- Infected parents or caretakers
- HIV infection
- Excessive sweating
 Quick fact
Quick factThere are various types of fungal infections and several modes of transmission through which a baby can catch a fungus.
Types Of Fungal Infections
Fungal infections are distinguished based on their location on the body, severity, and the kind of fungus involved.
They can be broadly categorized under the following types (4).
- Superficial or cutaneous fungal infections affect the hair, nails, and upper layer of skin.
- Subcutaneous fungal infections affect the tissue under the skin.
- Systemic fungal infection is the most severe, as it affects multiple tissues in the body, usually in immunocompromised children.
Causes, Symptoms, And Treatment Of Fungal Infections In Babies
There are several types of fungal infections, each of them characterized with unique symptoms and treatment methods. We’ll explain the most common fungal infections that affect babies and toddlers.
1. Tinea or ringworm infections

Image: Shutterstock
It is a fungal skin infection common across all age groups (4). Tinea infections are caused by a group of fungi called dermatophytes. These infections are named based on the part of the body affected, namely tinea capitis for the scalp, tinea pedis for feet, and tinea corporis when the skin of any other part of the body is affected (10) (11) (5).
Causes
- Direct contact with an infected parent, caretaker, or another baby.
- Sharing items such as napkins, toys, combs, towels, clothing, etc., with an infected person.
- Coming in contact with an infected surface such as floors or playmats of the creche or by infected carpets or couches.
- Playing with an infected pet.
- Frequent nail trauma that may provide an opening for the fungus to enter.
- Presence of existing skin problems, like psoriasis.
- Immunocompromised babies and toddlers, like those with LeukemiaiA cancer of the blood cells where there is a rapid growth of abnormal blood cells. or HIV.
It can take days or up to two weeks after being in contact with the fungus and developing the infection.
Symptoms
- Initially, the lesion starts as a flat, red, and scaly spot on the skin.
- Gradually, the infection begins to spread outward in a circular direction.
- The outermost edge of a lesion appears red and swollen.
- As it spreads more towards outside, the center part of the lesion begins to look healthier.
- There might be one or multiple patches in different areas of the body. These lesions might be itchy.
Treatment
The topical application of antifungal agents should be prescribed by your doctor in a form of antifungal cream or antifungal oral medication.
A list of antifungal creams used in treating ringworm in babies is provided below (12):
- Clotrimazole
- Ketoconazole
- Miconazole
- Terbinafine
Tinea may be hard to cure and might come back, especially scalp and nail infection. The length of the treatment depends on the location of the infection.
2. Oropharyngeal candidiasis or thrush

Image: Shutterstock
Thrush in babies is an infection of the oral mucosaiMucous membrane that lines the inner surfaces of the mouth. . It can affect the throat, gums, palate, inner part of the lips, or tongue (7).
Causes
- A variety of species of the genus Candida cause oral candidiasis including: Candida albicans (most common), C glabrata, and C tropicalis. Candida is a dimorphic fungus normally present in small amounts in the oropharyngeal region.
- At times, when the body’s immunity is compromised, the balance of microorganisms gets disrupted, and the body is invaded by the fungus that grows out of control.
- Babies and toddlers who have been given broad-spectrum antibiotics are at a higher risk of getting affected by thrush. It is due to the depletion of good bacteria, which usually compete with fungus and prevent infection.
- It is more common in immunocompromised babies.
Symptoms
- White or whitish-yellow plaques and erythemaiReddish discoloration of the skin due to an infection or certain medicines. are seen on cheeks, gums, palate, throat, tongue, or the inside of the lips in babies with oral candidiasis.
- These lesions might cause a burning sensation in the mouth.
- The babies may not eat or eat less food than usual and might get cranky.
- The presence of concomitant diaper rash may also aid in the diagnosis of an oral candidal infection.
Treatment
Oral candidiasis usually responds well to treatment with a topical antifungal agent such as nystatin suspension or clotrimazole. Gentian violet has been used as a treatment for oral candidiasis but is less effective than newer antifungal medications.
Treatment duration usually is two weeks, but medication should be continued two to three days beyond the resolution of symptoms.
Recurrent or persistent oral candidiasis:
- Oral candidiasis that persists or recurs soon after treatment in babies younger than age six months should consider a possible external fungal reservoir (tooth-brushes, vitamin droppers, and other objects that may have come in frequent contact with child’s mouth)
- Recurrent or persistent oral candidiasis in breastfeeding infants should raise the consideration of maternal breast colonization as a cause.
- Frequent relapses of oral candidiasis should lead to child’s immunological assessment.
3. Candida diaper rash

Image: IStock
According to the American Academy of Pediatrics (AAP), at least half of all babies develop diaper rash at some point. Generally, a baby’s diaper rash can be classified into different types. Candida diaper rash, also called diaper dermatitis, is a highly prevalent type in babies. The fungus grows rapidly in moist areas, such as the diaper area (8).
Causes
- Contact with urine and fecal matter raise the pH of the skin, which makes it easier for the fungus to multiply. An acidic skin surface is also essential for the maintenance of the normal microflora, and providing antimicrobial protection against invasion by pathogenic bacteria and yeasts.
- The main irritants are fecal proteases and lipasesiEnzymes that break down fats in the food, making it easier for them to be digested by the body. and ammonia.
- Direct usage of Broad-spectrum antibiotics usage in children or in breastfeeding mothers may increase the risk of developing diaper rash.
- Prolonged wetness leads to increased susceptibility to candida infection.
Symptoms
- It causes dark red patches on the buttocks, thighs, or around the genitals.
- The patches often appear inflamed.
- In some cases, areas of papules, vesicles, and small superficial erosions may be present.
- The babies might look uncomfortable and be fussier than usual.
- They might cry when the diapers are being changed or when they are being cleaned.
Treatment
Advise the parents to keep the skin in the diaper area as dry as possible
- More frequent diaper changes (as often as every 2 hours or every time it becomes wet)
- Use of breathable disposable diapers
- Use of barrier creams, such as zinc oxide paste or petroleum jelly, is recommended to minimize urine and fecal contact with the skin.
Topical application of antifungal agents such as Nystatin, Amphotericin B, Miconazole, and Clotrimazole is the most common treatment for candida or yeast diaper rash (12).
 Quick tip
Quick tipDiagnosis Of Fungal Infection
Fungal infections are usually diagnosed through clinical examination and medical history. If required, the doctor may scrape the lesion and send it for a microscopic examination or a culture test. At times, they may use ultraviolet light to see the lesion more clearly.
The doctor will prescribe the treatment based on the type of fungus causing the infection. Always seek a doctor’s suggestion before considering and administering any pediatric OTC ointments containing corticosteroids, gels, oral suspension, or medicines for your baby. Parents may also consider some home remedies for relief.
Home Remedies For Fungal Skin Infection In Babies
Several natural remedies have been in use to get relief from fungal infection. The evidence on their efficacy is mostly anecdotal.
- Tea tree oil is known for its antimicrobial properties. Some people use diluted tea tree oil for nappy rash.
- Oats tied in a muslin cloth and added to the baby’s bathing water may soothe the diaper rash.
- Aloe vera is known for its soothing effect on the skin. Fresh aloe vera pulp or gel from a bottle may be used to provide some relief.
- Some people apply breast milk directly to the lesion as breast milk is said to have natural healing properties.
- Some scientific evidence is available to establish the role of oregano oil in helping the healing of fungal infections. But the studies were not done on humans and are not conclusive. More research is needed to establish its efficacy (13).
- Traditionally, chamomile has been in use to treat diaper rash. However, there is a lack of scientific evidence to confirm its efficacy (14).
- Some researchers have proven the efficacy of honey in curing various skin problems and infections. However, this needs to be studied further (15).
There is no conclusive scientific evidence to prove the efficacy of home remedies for fighting fungal infections. Also, babies and toddlers have delicate skin, which could be sensitive. Therefore, it is best to consult a doctor even if you plan to use home remedies against fungal infections.
Can You Prevent Fungal Infection In Babies?
It may not be possible to prevent all fungal infections. But taking precautionary measures may minimize the risk of infections. Here are some such measures.
- Dress the baby in a fresh diaper each day. Change the baby to a fresh diaper for the night, even if the baby has not soiled the diaper they are wearing.

Image: Shutterstock
- Always keep your baby and their surroundings clean.
- As fungus tends to grow in moist areas, always towel dry your baby and give some cloth-free time to babies after bathing.
- Wipe the baby’s buttocks and surrounding areas with warm soapy water after they soil a diaper. Let the baby dry thoroughly before putting on a fresh diaper.
- If your baby has a rash, then use the rash cream recommended by your doctor in the prescribed amount and frequency.
- Try and avoid sharing combs, linen, towels, hats, etc.
- Avoid any contact of the baby with persons who have an infection.
- If the baby has a fungal infection in one part of the body, avoid using the same towel to dry the other parts of the body.
- Discourage the baby from touching the infected part or scratch it as it might lead to further spread of the infection.
- Make them wear shoes in public places.
- Have your pets regularly screened for fungal infections and get them treated when needed.
Frequently Asked Questions
1. Is fungal infection contagious in babies?
Yes, fungal infections are highly contagious. They can spread from one person to the other and also from one infected part of the body to the other. Therefore, babies need to avoid contact with pets and family members who have a fungal infection.
2. Can babies be born with fungal infections?
Babies are not born with a fungal infection but can develop one within a few days of birth. For instance, babies who are born with very low birth weight or prematurely may be prone to fungal infection (7) (12). Prolonged hospital stay post-birth might also increase the chances of fungal infections in babies.
3. How long does fungal infection last in babies?
While fungal infections usually heal in two weeks, more severe infections in babies with catheters or immunocompromised babies may take months to heal (16).
4. Do fungal infections go away permanently?
Fungal infections are treatable. However, it is not uncommon for babies to experience a recurrent infection (16).
Tinea infections and Candida diaper rash are two frequent fungal diseases in infants that can be superficial, subcutaneous, or systemic. Although fungus infections in babies are common, factors such as prematurity, malnutrition, low birth weight, hot and humid conditions, and close contact with pets and farm animals might increase the risk of infection. However, all these infections are treatable. So, keep a watch on your baby’s skin and oral cavity for any sores, and contact your child’s pediatrician immediately if you suspect an infection. Maintaining good hygiene, using clean towels, frequent diaper changes, and other home care tips can also be helpful.
Infographic: How To Treat A Baby’s Fungal Skin Infection At Home?
Due to various factors, including their immature immune systems, babies are more likely than adults to acquire fungal skin infections. While several topical drugs, creams, and lotions are available to treat these infections effectively, if you’re looking for some natural treatment options, check out the infographic below. Illustration: Momjunction Design Team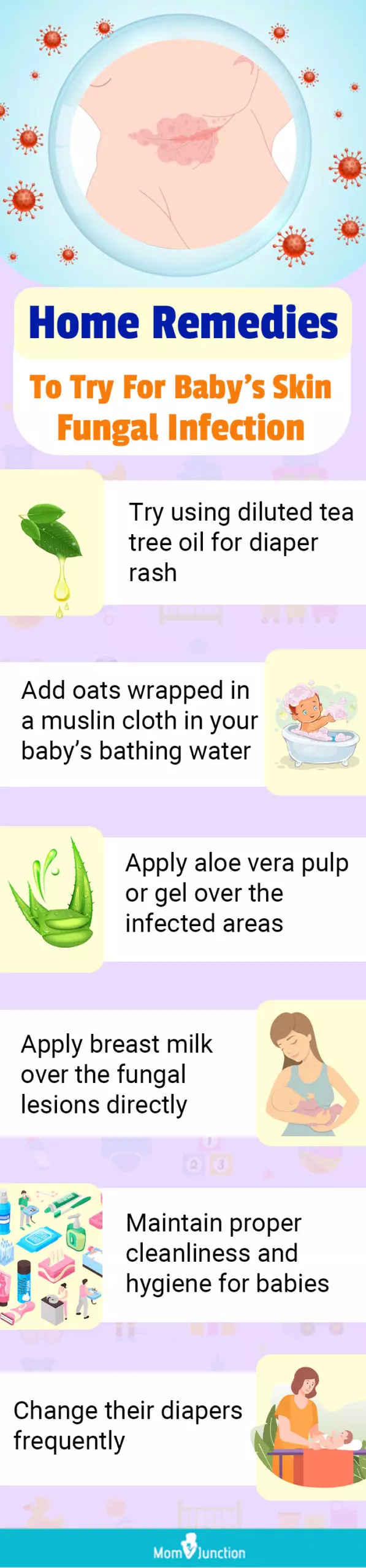
Illustration: Fungal Infection In Babies: Risks Treatment And Remedies

Image: Stable Diffusion/MomJunction Design Team
In the video below, you may explore Candida Fungal Infections and their possible treatments. This video also helps you uncover the symptoms, causes, and remedies for this prevalent ailment.
References
- Fungal Infections – Protect Your Health; Centers for Disease Control and Prevention.
https://stacks.cdc.gov/view/cdc/126879/cdc_126879_DS1.pdf - Mamdouh R. Sakr Fungal and Bacterial Infection in Malnourished Children and its Relation to Severity of the Disease; Journal of Medical Sciences
https://scialert.net/fulltext/?doi=jms.2006.432.438 - Alok Kumar Sahoo and Rahul Mahajan Management of tinea corporis tinea cruris and tinea pedis: A comprehensive review; Indian Journal of Dermatology
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4804599/ - Akansha Jain Shubham Jain and Swati Rawat Emerging fungal infections among children: A review on its clinical manifestations diagnosis and prevention; Journal of Pharmacy and Bioallied Sciences
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2996076/ - Nourchene Toukabri et al. Prevalence Etiology and Risk Factors of Tinea Pedis and Tinea Unguium in Tunisia; Canadian Journal of Infectious Disease and Medical Microbiology.
https://www.hindawi.com/journals/cjidmm/2017/6835725/ - Pet-Related Infections; American Family Physician
https://www.aafp.org/pubs/afp/issues/2007/1101/p1314.html - Jose Endrigo Tinoco-Araujo et al. Invasive Candidiasis and oral manifestations in premature newborns; Journal of Einstein (Sao Paulo)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4872971/ - Jan Hau Lee et al. Risk Factors for Invasive Candidiasis in Infants >1500 g Birth Weight; National Center for Biotechnology Information.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3578110/ - Shyam Verma and R Madhu. The Great Indian Epidemic of Superficial Dermatophytosis: An Appraisal; Indian Journal of Dermatology
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5448256/ - Narcisa Mandras et al A case report of tinea capitis in infant in first year of life; Biomed Central Pediatrics
https://bmcpediatr.biomedcentral.com/articles/10.1186/s12887-019-1433-7 - Antoni Bennassar and Ramon Grimalt Management of tinea capitis in childhood; Journal of Clinical Cosmetic and Investigational Dermatology
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3047946/ - Antifungal agents for common paediatric infections; Journal of Pediatrics Child Health
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2819966/ - Manohar V et al. Antifungal activities of origanum oil against Candida albicans; National Center for Biotechnology Information
https://www.ncbi.nlm.nih.gov/pubmed/11855736 - Janmejai K Srivastava Eswar Shankar and Sanjay Gupta Chamomile: A herbal medicine of the past with bright future; National Center for Biotechnology Information.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2995283/ - N.S Al-Waili An alternative treatment for pityriasis versicolor tinea cruris tinea corporis and tinea faciei with topical application of honey olive oil and beeswax mixture: an open pilot study; Journal of Complementary therapies in medicine
https://www.sciencedirect.com/science/article/abs/pii/S0965229904000056 - Thrush and Other Candida Infections.
https://www.healthychildren.org/English/health-issues/conditions/infections/Pages/Thrush-and-Other-Candida-Infections.aspx - Emily Hsieh et al.; (2012); Neonatal fungal infections: when to treat?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3512570/ - Diaper rash.
https://kidshealth.org/en/parents/diaper-rash.html
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Nikolina Zdraveska
Read full bio of Dr. Ritika Shah
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny



















