
Image: ShutterStock
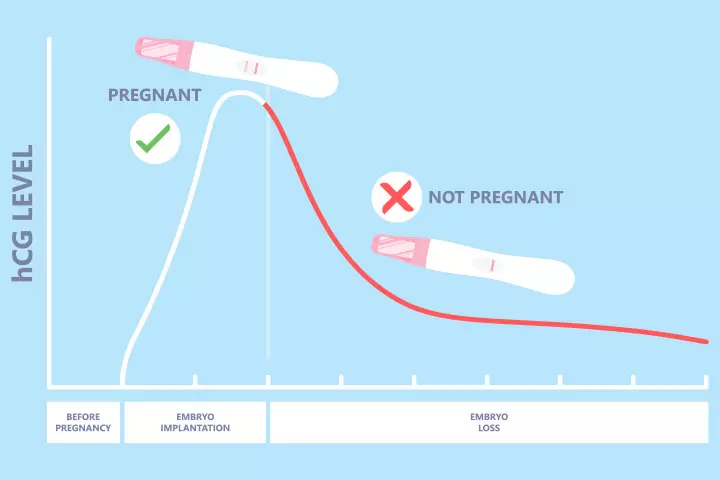
The placentaiA temporary organ formed in pregnancy that clings to the uterus and supplies nutrients and oxygen to the developing fetus produces the pregnancy hormone hCG (human chorionic gonadotrophin) to assist the growth of the fetus. During the first few weeks of a healthy pregnancy, it multiplies every 48 to 72 hours and can be determined through urine and blood testing (1). However, during a miscarriage, the hCG levels drop (medically referred to as a non-viable pregnancyiA pregnancy that cannot result in a live birth. ) and may soon reach hCG level after miscarriage.
Read this post to learn how long hCG levels last after a miscarriage, when they return to pre-pregnancy levels, and if you can ovulate with hCG in your system after a miscarriage.
Key Pointers
- The duration for hCG levels to reach zero after a miscarriage is influenced by multiple factors.
- A quick decrease in hCG levels could indicate a miscarriage or unsuccessful pregnancy.
- A slow decline in hCG levels may reveal remaining tissue or an ectopic pregnancy.
- Complete absence of hCG levels points to a miscarriage.
- A blood test can be conducted to analyze hCG levels for confirmation or monitoring of pregnancy.
How Long Does It Take For The hCG Levels To Fall To Zero After A Miscarriage?
La Toya Luces-Sampson, MD, FACOG, a board-certified obstetrician and gynecologist from Stockton, California, says, “hCG levels usually rapidly decline after a complete miscarriage, passing all of the pregnancy tissue, but can take several days to weeks to reach zero once the levels become very low.”
The duration varies from woman to woman. It is likely to depend on how high your hCG levels were during the miscarriage. Usually, test results of fewer than five mIU/mL are considered negative or zero (1).
The level of hCG increases with each passing day during the early pregnancy and peaks highest at about 8–10 weeks, suggesting a successful early pregnancy (12). If you had a miscarriage early in your pregnancy, your levels are usually low, and hCG levels return to zero in less time. On the other hand, if the levels are high at the time of the miscarriage or if you had a miscarriage late in your pregnancy, it might take several days or weeks to return to zero (2).
According to the American Association for Clinical Chemistry (AACC), urine hCG and serum hCG levels may take anywhere between nine and 35 days to disappear from your system (3).
Some studies done at the MUHC Reproductive Center at McGill University suggest that the higher the β-hCG levels in early pregnancy, the lower the risk of pregnancy loss (17). This correlation between serum β-hCG levels and pregnancy loss is depicted in the graph below. The study was conducted on a total of 1076 pregnancies, and the graph indicated that the risk of a biochemical pregnancy loss was lowest when the level of β-hCG increased up to 391-10,764 IU/L.

Association between biochemical pregnancy loss and serum β-hCG levels
Source: Revisiting serum β-hCG cut-off levels and pregnancy outcomes using single embryo transfer; Journal of assisted reproduction and geneticsWhy Do hCG Levels Keep Increasing After A Miscarriage?
The hCG level can increase after a miscarriage in the case of (16):
- Heterotropic pregnancy: Simultaneous occurrence of extra-uterine (ectopic pregnancy) and intrauterine pregnancy)
- Persistent trophoblastic disease: Molar tissue starts growing again after the removal of molar pregnancy
Dr. Luces-Sampson adds, “There may be a fetal death with no passage of fetal tissue, where the hCG levels continue to rise, stay the same, or slightly decrease over time. In this case, the diagnosis is confirmed by ultrasound.”
How Soon Can You Get Pregnant After A Miscarriage?
While some doctors may recommend waiting for three months, several experts opine that there is no need to delay pregnancy after an early pregnancy or embryo loss (4).
 Experts say
Experts sayCan You Get A Pregnancy False-Positive Reading After Miscarriage?
Yes, you might get a false-positive test reading after a miscarriage because hCG may still remain in your bloodstream for weeks following a pregnancy loss or at the end of pregnancy. Thus, the test readings might show that you are pregnant even when you are not (5).
Can You Ovulate With hCG In Your System After A Miscarriage?
hCG hormone levels are likely to suppress your normal ovulation process. Your next cycle may start only when the hCG levels drop below 5mIU/mL (6).
 Quick fact
Quick factSeeking medical advice is particularly important when monitoring the hCG level after miscarriage, as these levels need to return to pre-pregnancy levels before ovulation can resume. A healthcare provider can help track this and confirm if your body has fully healed. If you experience irregular bleeding, signs of infection, or prolonged emotional distress, prompt medical consultation is essential for your well-being.
Frequently Asked Questions
1. Why won’t my HCG levels go down even after a miscarriage?
It may take about four to six weeks for HCG levels to return to normal after a miscarriage, so you get a positive hCG report if tested. Moreover, some women may immediately have pregnancy after a miscarriage, and the new pregnancy may be responsible for the presence of hCG in the blood (7).
2. How can I check my hCG levels at home?
Home pregnancy test kits detect the presence or absence of hCG levels. However, they cannot detect hCG quantitatively. HCG blood pregnancy test in the clinic is the only way of detecting hCG levels in the blood and determining the gestational age.
3. Does hCG have to be zero to get a period?
hCG levels need to be near zero for ovulation to occur. Once ovulation occurs, you get a period after about two weeks (8). Therefore, you will get your first period after miscarriage once your hCG levels reach near zero.
4. Do low hCG levels mean a miscarriage?
Dr. Luces-Sampson observes, “A ‘low’ hCG should be taken with a grain of salt because one number in isolation gives very little information. Serial (usually every 48 hours) hCG tests are needed to accurately predict pregnancy loss. The hCG levels usually double every 48 hours, but the increase can be as low as a 50% increase and still indicate a normal pregnancy.”
5. Can hCG levels be used to detect a blighted ovum?
During weeks 6-8, hCG and gestational sac diameter are usually normal in blighted ovum cases. After week 9, sac diameters are below normal, but hCG can still be normal until week 14. Thus, hCG alone cannot detect blighted ovum (12).
6. How do hCG levels change during a chemical pregnancy?
In a chemical pregnancy, if the embryo ceases to develop, hCG levels decrease since it’s the primary source. A decrease or absence of hCG results from embryo cessation, resulting in lower hCG levels (13).
7. Can hCG levels be used to diagnose a missed miscarriage?
In missed miscarriage cases, hCG levels are usually normal in weeks six to eight. Normal hCG levels occasionally remain until week 14. Therefore, hCG levels alone cannot diagnose missed miscarriage (12).
8. Can hCG levels be used to diagnose a recurrent miscarriage?
No, hCG levels alone cannot diagnose recurrent miscarriage. Doctors use various tests, such as genetic screening, hormone level checks, ultrasound, and endometrial biopsy, to diagnose the condition (14).
9. How do hCG levels change during a partial molar pregnancy?
Beta hCG levels increase quickly during regular pregnancies. In a partial molar pregnancy, beta hCG levels rise even faster and can reach higher levels than in normal pregnancy (15).
The hCG level after miscarriage may decline in most women. However, it may give positive results for a few weeks. When the pregnancy is lost, the HCG production ceases from the placenta. Heterotopic pregnancy, which is two pregnancies with different implantation sites and gestational trophoblastic diseases, can cause increasing HCG levels in the blood after miscarriage. Lower HCG hormones are less likely to impact ovulation, so it is possible to start the next cycle when the HCG levels fall below certain levels. You may seek medical care and do HCG blood tests during follow-ups after miscarriage.
Infographic: Does HCG Level Predict Risks For Miscarriage?
HCG levels can be low or abnormally high for various reasons in viable and nonviable pregnancies. Clinical symptoms and prenatal ultrasound help to establish a better diagnosis than HCG levels alone. Go through the infographic to learn about HCG level changes and miscarriage risks in pregnancy. Illustration: Momjunction Design Team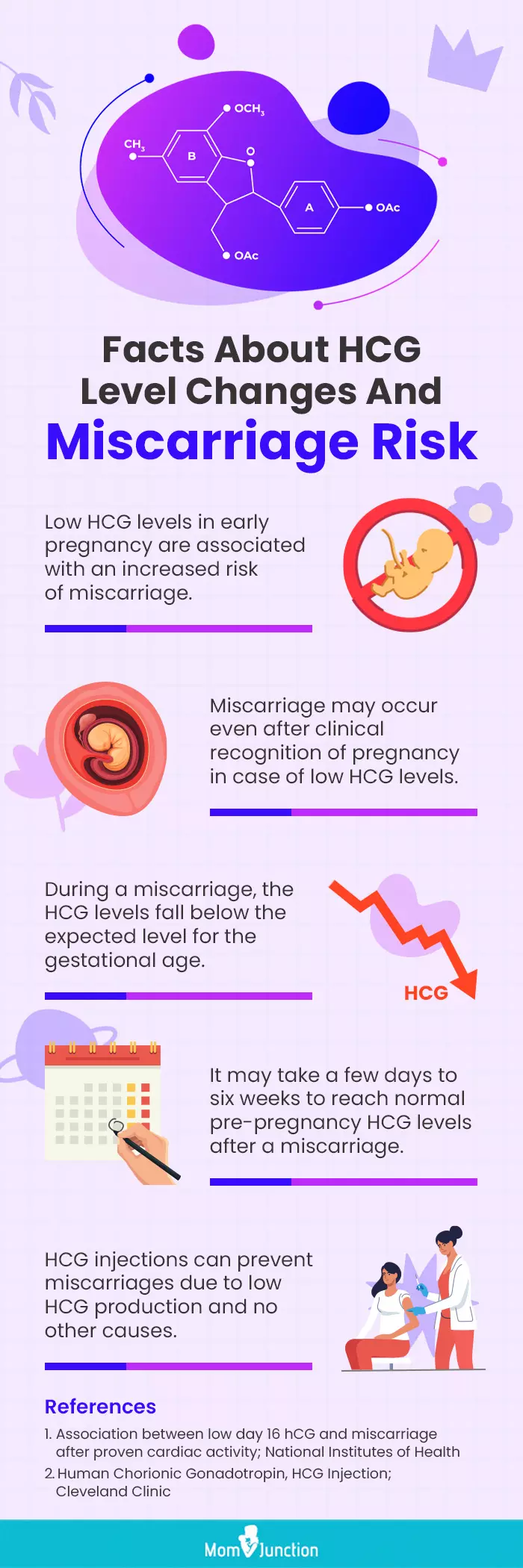
It’s a common question – how long does it take for HCG to leave a woman’s system after pregnancy? Let’s find out in this video!
References
1. HCG (Urine); University of Rochester Medical Center
2. Danielle Betz and Kathleen Fane; Human Chorionic Gonadotropin (HCG); : StatPearls Publishing; (2020)
3. Pregnancy Test (hCG); American Association for Clinical Chemistry
4. Karen C. Schliep, et al.; Trying to Conceive After an Early Pregnancy Loss: An Assessment on How Long Couples Should Wait; Obstet Gynecol (2017).
5. 1st Trimester Bleeding and Pregnancy Loss; OB-GYN 101: Introductory Obstetrics & Gynecology
6. Beata E. Seeber; What serial hCG can tell you, and cannot tell you, about an early pregnancy; Fertility and Sterility; American Society for Reproductive Medicine – Elsevier Inc (2012).
7. What is HCG?; American Pregnancy Association.
8. Leading Fertility Expert’s Guide To Getting Pregnant Again After A Miscarriage; Harley Street Fertility Clinic.
9. How to Be Reasonably Certain That a Patient is Not Pregnant; CDC
10. Pregnancy intentions and contraceptive uptake after miscarriage;NCBI
11. Getting Pregnant Again After A Miscarriage; Harley Street Fertility Clinic
12. Correlation of human chorionic gonadotropin secretion in early pregnancy failure with size of gestational sac and placental histology; PubMed
13. Chemical Pregnancy: Causes, Symptoms & Treatment; Cleveland Clinic
14. Diagnosing Recurrent Miscarriage; NYU Langone Health
15. Partial Molar Pregnancy: Causes, Symptoms, Diagnosis & Treatment; Cleveland Clinic
16. Jianing Chen et al.; Persistent mild increase of human chorionic gonadotropin levels in a 31-year-old woman after spontaneous abortion; Canadian Medical Association Journal (2016)
17. Naama Al Mamari et al.; Revisiting serum β-hCG cut-off levels and pregnancy outcomes using single embryo transfer; Journal of Assisted Reproduction and Genetics (2019)
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sangeeta Agrawal
- Dr. Latoya Asha Luces is a healthcare provider with a specialty in Obstetrics & Gynecology. She works primarily from Stockton, CA, with other offices in Modesto, CA, and Patterson, CA. Dr. Luces did her education at Howard University and has seven years of work experience.
 Dr. Latoya Asha Luces is a healthcare provider with a specialty in Obstetrics & Gynecology. She works primarily from Stockton, CA, with other offices in Modesto, CA, and Patterson, CA. Dr. Luces did her education at Howard University and has seven years of work experience.
Dr. Latoya Asha Luces is a healthcare provider with a specialty in Obstetrics & Gynecology. She works primarily from Stockton, CA, with other offices in Modesto, CA, and Patterson, CA. Dr. Luces did her education at Howard University and has seven years of work experience.
Read full bio of Rebecca Malachi
Read full bio of Dr. Ritika Shah
Read full bio of Reshmi Das






















