Image: Shutterstock
Polycystic ovary syndrome (PCOS) is a common hormonal disorder affecting women of reproductive age. This post discusses PCOS in pregnancy and the causes, risk factors, symptoms, complications, diagnosis, and treatment of PCOS.
PCOS disrupts normal ovary function and results in irregular periods, excess androgen levels, and multiple enlarged ovarian follicles. These enlarged follicles do not release an egg (ovulation) as usual. Nearly 6-12% of women in the US are affected by PCOS, and it’s one of the common causes of female infertility. However, early treatment and lifestyle changes can help prevent PCOS complications in most women (1).
Key Pointers
- PCOS is a hormonal condition that can cause infertility in women, but it can be managed effectively.
- A woman’s age, medication use, and other fertility factors can affect her ability to conceive if she has PCOS.
- Women with PCOS may experience preterm birth, gestational diabetes, and miscarriages during pregnancy.
- Women with PCOS can increase their chances of having a healthy pregnancy by adopting healthy lifestyle habits such as regular exercise, a balanced diet, and stress reduction.
Can You Get Pregnant With PCOS?
Having PCOS does not mean a woman cannot get pregnant. If you are wondering, “Why am I not getting pregnant?”, know that it is not a lost cause. Infertility due to PCOS can be treated effectively in most women. Lack of ovulation due to hormonal imbalances causes infertility in PCOS. You should seek medical care if you cannot conceive after trying for several months. Doctors may recommend lifestyle changes and medications that can induce ovulation and increase the chance of pregnancy.
How To Increase Your Chances Of Getting Pregnant With PCOS?

Adopting a healthy lifestyle can increase the chance of conception in many women with PCOS. You may try the following ways to improve your fertility (2):
- Maintain healthy weight
- Avoid smoking
- Avoid alcohol
- Eat healthily
- Practice regular exercise
- Get enough sleep
Seeking a preconception health check-up from your physician and planning actions to improve fertility can help. Minimal weight loss can also improve the chance of conception in many women with PCOS and who are overweight. You may also track ovulation using an ovulation calculator and try intercourse in the fertile days (fertility window) to boost the chance of pregnancy.
A study has shown that weight loss or bariatric surgery can positively impact pregnancy and fertility outcomes in women with PCOS. Among the ones who underwent surgery, 53 had PCOS. As the graph below depicts, the pregnancy rate was higher (40.8 %) in women with PCOS than in the control group (women without PCOS). In addition, a higher fertility rate was observed in women with PCOS after bariatric surgery, particularly those seeking pregnancy.

Pregnancy and live birth rates in women with PCOS after bariatric surgery
Source: Fertility and Pregnancy Outcomes in Women with Polycystic Ovary Syndrome Following Bariatric Surgery; The Journal of Clinical Endocrinology & Metabolism Quick tip
Quick tipWhat Is The Success Rate Of Pregnancy With PCOS?
The pregnancy success rate in women with PCOS may vary depending on their age, type of medications used for ovulation induction, response to the medications, and other infertility factors present in the couple. The success rate for pregnancy is high in the first three to four months of treatment. However, the rates drop after this period.
According to the data published by the Advanced Fertility Center of Chicago, the average monthly success rate of pregnancy in women less than 35 years undergoing PCOS treatment and the partner has normal sperm are as follows (3):
- 1-2% in metformin alone
- 15% if ovulation occurs with Clomid (clomiphene citrate)
- 15% if ovulation occurs with Femara
- 20% with injectable gonadotropins
- 60% and above with IVF or in vitro fertilization

The success rate can be lower after 35 years of age or issues with sperm count or motility. Therefore, you may seek infertility treatment as early as possible when you fail to conceive naturally.
What Are The Possible Risks Of PCOS To The Mother And Baby?
PCOS can increase the risk of certain complications to the mother and the baby during pregnancy and delivery. These complications can increase the risk of spending more time in the neonatal intensive care unit (NICU) in many babies. Some complications may result in stillbirth or infant mortality.
Pregnancy and delivery complications related to PCOS may include (4):
- Miscarriage or early pregnancy loss is three times more likely in women with PCOS than in others.
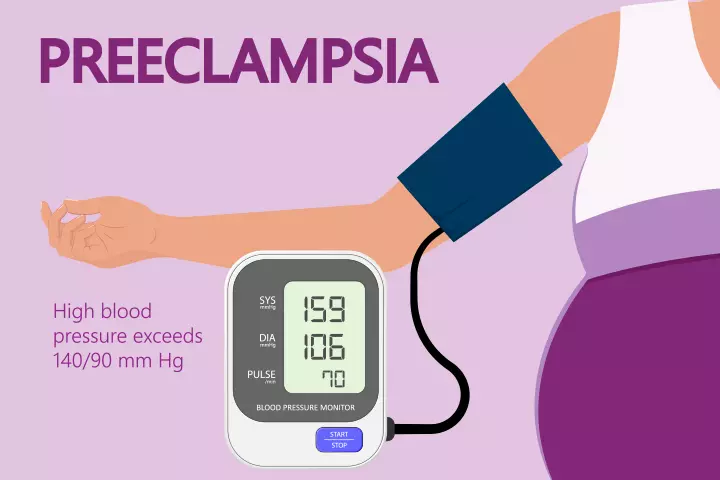
- Gestational diabetes may occur in mothers with PCOS. This can be controlled with treatment. Uncontrolled gestational diabetes may increase the risk of having a larger baby, low blood sugar, and breathing issues.
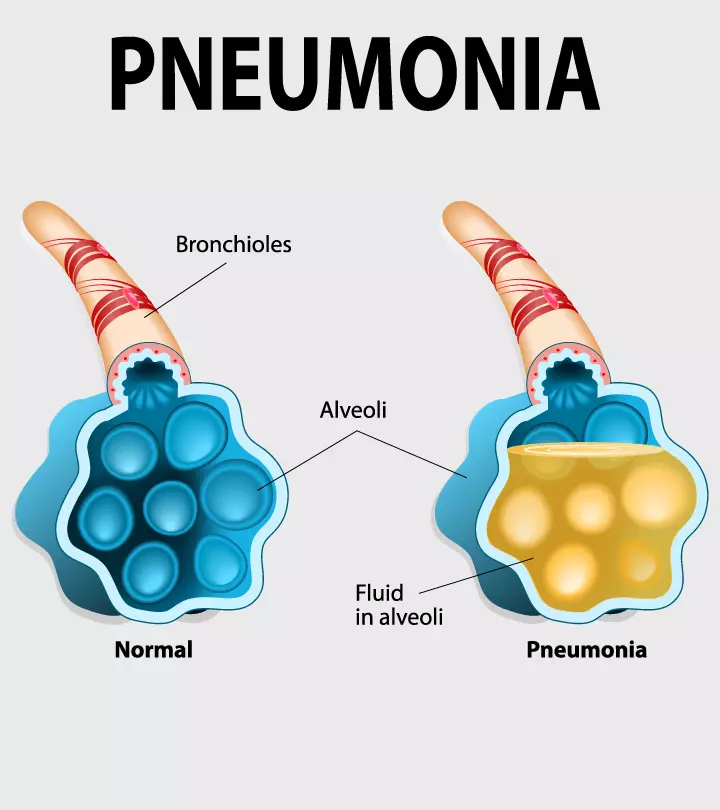
- Preeclampsia increases blood pressure with proteinuria after the 20th week of pregnancy. If not controlled, preeclampsia may damage major organs such as the brain, kidneys, liver, and heart.
- Eclampsia is organ damage and seizure with high blood pressure. This is a medical emergency and can be life-threatening if left untreated (5).
- Preterm labor may occur before 37 weeks, and the babies born early are at risk of various health issues and require a hospital stay for a longer time.
Some studies show that insulin-sensitizing drugs such as metformin can reduce the risk of pregnancy complications in women with PCOS. You may seek medical care and take the prescribed medications throughout pregnancy to help prevent PCOS complications.
What Are Delivery Complications In PCOS?
Delivery complications may occur in women with PCOS. Gestational diabetes may occur in many women with PCOS. This can lead to large sizes babies, requiring c-section deliveries. Larger babies can cause shoulder dystocia (shoulder stuck in the birth canal) during delivery.
Preeclampsia can also increase the chance of cesarean section delivery in women with PCOS. Close monitoring and treating pregnancy complications and managing PCOS may help reduce delivery complications (6).
What Are The Risk Factors And Causes Of PCOS?
The exact causes of PCOS are not known in several cases. However, most women with PCOS have androgen levels (male hormones) higher than normal, which may play a role. In addition, the following factors may increase the risk of developing PCOS (1) (7):
- Excess body weight: Weight gain or obesity might cause PCOS in some women. According to the American College of Obstetricians and Gynecologists (ACOG), about four in five women who suffer from PCOS also exhibit signs of obesity. However, many women with normal weight can also have PCOS, and many women with overweight may not have.
- Family history: Women with first-degree relatives (mother or sister) with PCOS or type 2 diabetes may have an increased risk for PCOS than others.
- Insulin resistance: Lifestyle-related factors, such as being overweight due to unhealthy eating and lack of exercise, may contribute to insulin resistance in many women. This may also run in families. Weight loss may improve insulin resistance regardless of cause.
- Epilepsy: Women with epilepsy have an increased risk for PCOS and other reproductive disorders. Antiepileptic drug valproic acid may contribute to features of the polycystic ovary syndrome, including weight gain, increased insulin levels in the blood, and increased testosterone levels (male hormone). This drug is also given for treating bipolar disorders and migraines.

- Diabetes mellitus: Type 1, type 2, and gestational diabetes may increase PCOS prevalence.
- Prenatal factors: High birth weight, congenital virilization (excess male hormone exposure in newborns), low birth weight, etc., can be associated with PCOS in later life.
- Childhood factors: Atypical central precocious puberty, premature pubarche (early appearance of pubic hair), acanthosis nigricans, obesity syndromes, and metabolic syndromes may contribute to PCOS in later life. A higher risk for PCOS is seen in adolescents with persistently irregular menstruation and the above risk factors.
What Are The Signs And Symptoms Of PCOS?
Signs and symptoms aren’t the same for every woman. Some may have more sets of symptoms, while a few may have only one or two symptoms of PCOS. The severity of PCOS symptoms can also vary from mild to severe. Most women with overweight or obesity may have severe symptoms compared to women with normal body mass index (BMI).
PCOS signs and symptoms may include (8) (9):
- Menstrual abnormalities, such as irregular periods, missed periods (amenorrhea), light periods, or heavy periods can occur in many women with PCOS. Less than nine periods in a year or more than 35 days between periods (cycle interval) can be seen in PCOS.
- Excess body hair, such as hair on the stomach, chest, and back (hirsutism)
- Weight gain, especially around the abdomen (belly)
- Oily skin or acne
- Infertility due to ovulation problems
- Male pattern hair loss on the scalp (baldness) or thinning of hair
- Skin tags on armpits and neck
- Dark or thick skin patches on the armpit, under breasts, or on the back of the neck
Lack of ovulation can be the reason for menstrual abnormalities in women with PCOS. In addition, some women may have mood changes, including depression and anxiety. However, the exact mechanism of mood changes in PCOS is not well understood. Obesity and sleep apnea can also be seen in some women.
How Is PCOS Diagnosed?
PCOS is clinically diagnosed based on symptoms, medical history, and physical examination. The following tests are recommended for clinically suspected cases to confirm the diagnosis (8):
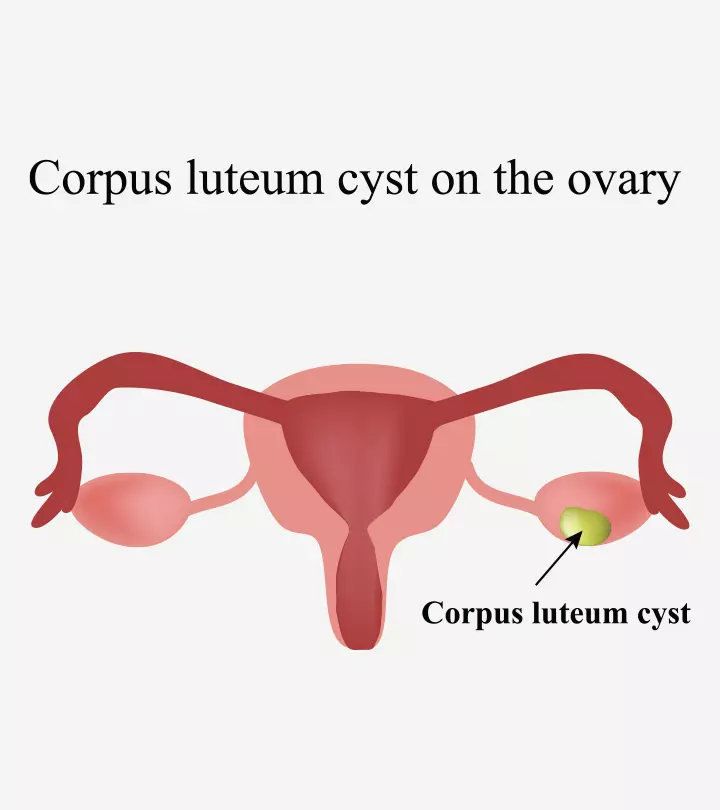
- Ultrasound imaging of the ovaries and uterus may help visualize the size of ovaries, ovarian cysts, and thickness of the endometrium (inner lining of the uterus). Ovaries can be enlarged, and follicles surround the eggs.

- Blood tests help to determine the levels of hormones and blood glucose. Cholesterol and triglyceride levels are also often checked.
Diagnosis of PCOS is made if a woman has two signs of PCOS, including irregular periods, excess androgen levels, or polycystic ovaries. PCOS can be diagnosed in puberty around the first menstruation in most women. However, some may develop it later due to substantial weight gain or other risk factors.
When To See A Doctor?
It is recommended to consult a doctor if you have any changes in menstrual periods or do not have periods. You may also seek medical care if you cannot conceive even after trying for several months. Signs of excess androgen such as hirsutism, acne, or male-pattern baldness require medical attention (10).
What Are The Treatment Options For PCOS?
Polycystic ovary syndrome is not curable, but the symptoms are manageable. The treatment options may vary for each woman, depending on their symptoms. Hysterosalpingography and sperm analysis are done before fertility treatments to optimize tubal patency and exclude other reasons for infertility.
The following treatments are recommended to manage PCOS symptoms (11) (12):
1. Lifestyle changes
Lifestyle changes can help prevent the risk of long-term health problems. For example, doctors may recommend a healthy diet to prevent insulin resistance and weight gain. Adequate physical activity is essential to promote well-being. Weight loss is one of the initial recommendations for women with PCOS and overweight or obesity.
Significant improvement of symptoms can be noticed on even 5% of weight loss. Eating small portions at least five times a day, including vegetables, fruits, whole grains, lean meat, and fish, is recommended. High glycemic index foods should be avoided. Most women can get symptomatic improvement and have normal ovulation reaching normal BMI (between 18.5 to 24.9).
 Did you know?
Did you know?2. Medications for menstrual irregularities
Hormonal contraceptive pills
are prescribed for irregular or absent periods to regulate or induce menstruation. Progestogen tablets are also suggested monthly or every three to four months to induce menstruation.
Other hormonal methods of contraception, such as the intrauterine system (IUS), can keep the endometrial lining thin. These medications also lower the risk of endometrial cancers associated with irregular periods.
3. Medications for fertility problems
Most women with PCOS can conceive and have a successful pregnancy with adequate treatment. Short-term courses of medications at the beginning of cycles for several cycles are prescribed to induce ovulation. Fertility treatments in women with PCOS may include:
- Clomiphene citrate is the first medication used to treat infertility in women with PCOS. This medication stimulates the release of eggs from the ovaries (ovulation). Sometimes this can be combined with metformin, a medication that lowers insulin levels in the blood. However, it is approved for treating women with insulin resistance, sometimes prescribed for others to promote fertility and to control PCOS symptoms.
- Letrozole is a medication prescribed to stimulate This is also a medication approved for treating breast cancer, not PCOS. However, some off-label use is permitted if the benefits outweigh the risks.
- Gonadotropin injections or in vitro fertilization (IVF) methods are recommended if a woman fails to conceive after a course of tablets. This may increase the risk of multiple pregnancies, such as twin pregnancies or more.
4. Medications for hair loss and unwanted hair growth
Hirsutism and male pattern hair loss (alopecia) in women with PCOS can be controlled with the following medications:
- Some combined oral contraceptive tablets, such as Yasmin, co-cyprindiol, Dianette, or Marvelon
- Flutamide
- Spironolactone
- Cryptorone acetate
- Finasteride
- Eflornithine cream
These medications block the effects of androgen (male hormones) or suppress androgen production by the ovaries. You may use eflornithine cream to slow down unwanted hair growth, such as unwanted facial hair. You may use it with other hair removal products or hair removal methods such as plucking, threading, shaving, or laser removal. Usually, four to eight months of treatment is required to slow down hair growth with eflornithine.
5. Medications for other PCOS symptoms
The following medications are also often used to manage some PCOS symptoms or their effects:
- Orlistat is a weight loss medication prescribed to treat obesity and overweight
- Statins are cholesterol-lowering medications prescribed for high cholesterol levels
- Acne treatments with topical medications, systemic antibiotics, or hormone therapies.
6. Surgery for PCOS
Some women with PCOS may require a minor surgical procedure called laparoscopic ovarian drilling (LOD). This procedure was mostly recommended for women who did not respond to other fertility medications, and lifestyle changes. Under general anesthesia, doctors will insert instruments through small incisions in the abdomen.
Androgen-producing cells of ovaries are destroyed by heat or laser in this procedure. It may help lower the male hormones, stimulate follicular stimulating hormone (FSH) production, and aid hormonal changes and repairs. However, LOD is not routinely used in fertility medications to help achieve pregnancy.
What Are The Complications Associated With PCOS?
PCOS can be associated with long-term health risks in many women (1) (9):
- Infertility
- Insulin resistance
- Increased risk for diabetes mellitus if overweight or obese
- Cholesterol and other blood fat(lipid) level abnormalities such as high LDL (bad) cholesterol levels and low HDL (good) cholesterol levels
- Increased risk for cardiovascular diseases, including stroke and heart attack
- Endometrial cancer if the endometrial lining thickness is long-standing
- Gestational hypertension (or high blood pressure) may damage the brain, heart, and kidneys.
- Sleep apnea is a pause of breathing during sleep.
- Anxiety and depression
Approximately 70-80% of women with PCOS can have infertility. Therefore, the American Society for Reproductive Medicine recommends women with PCOS and other infertility issues seek medical evaluation if they fail even after attempting six months of regular sex for pregnancy without using any contraceptive methods (11).
Can You Prevent PCOS Or Its Effects?
PCOS cannot be prevented. Although there are no proven ways to prevent it, small changes in lifestyle, such as regular physical activity, a healthy diet including nutritious foods, and keeping weight under normal levels help prevent any effects of PCOS. You may follow these changes lifelong to prevent PCOS complications. Some symptoms can also be seen in or after menopause (13).
Frequently Asked Questions
1. Why is miscarriage common in PCOS?
There are certain proposed mechanisms that may be responsible for early pregnancy loss in women with PCOS. They are (4):
- Elevated levels of luteinizing hormone (LH)
- High androgen levels that may counter the effects of estrogen
- Increased blood clotting tendencies
- Insulin resistance and high blood sugar levels that may affect maturation of ovum, implantation and further fetal growth.
- Endometrium is found to be less capable of supporting implantation
- Obesity which is more prevalent among women with PCOS is also associated with miscarriage risk
2. How can I prevent miscarriage with PCOS?
No particular therapy is applicable to all women with PCOS. Maintaining a healthy lifestyle with proper diet and exercise during pregnancy is advisable. Your doctor may prescribe certain medications after examining your condition.
3. Can women with PCOS have normal delivery?
Yes, women with PCOS can have vaginal delivery. However, a C-section may be required depending on the complications (14)
4. Will PCOS go away after delivery?
No. PCOS does not resolve after childbirth but the symptoms may vary (15).
5. What are the chances of conceiving naturally with PCOS?
Women with PCOS have a lower rate of natural conception, but it is not impossible (16). However, the rates may vary widely.
Women with PCOS need to follow lifestyle changes and prescribed medications to prevent complications. Keeping the hormones in balance before and during pregnancy can prevent related pregnancy and delivery complications in many cases. You may seek a healthcare provider’s advice before any PCOS treatment since the symptoms and severity may vary among women.
Infographic: Effective Ways To Improve Chances Of Pregnancy With PCOS
An unhealthy lifestyle and stress can increase the chances of developing PCOS. Although infertility is one of the complications of PCOS, it can be avoided, and the chances of getting pregnant can be increased through the right measures. The following infographic includes some useful tips and medication that can help increase the chances of pregnancy.

Illustration: Momjunction Design Team
Illustration: Tips To Increase Your Chances To Get Pregnant With PCOS

Image: Stable Diffusion/MomJunction Design Team
Get the expert’s advise on how to get pregnant with PCOS. Learn the tips and tricks to increase your chances of conceiving. Get the answers you need to start your journey to parenthood.
References
- Diabetes and Polycystic Ovary Syndrome (PCOS).
https://www.cdc.gov/diabetes/risk-factors/pcos-polycystic-ovary-syndrome.html?CDC_AAref_Val=https://www.cdc.gov/diabetes/basics/pcos.html - I have PCOS and I want to have a baby what do I need to know?
https://www.yourfertility.org.au/i-have-pcos-and-i-want-have-baby-what-do-i-need-know - PCOS Treatment for Pregnancy – Fertility Success Rates.
https://www.advancedfertility.com/2020/09/17/pcos-treatment-for-pregnancy-fertility-success-rates/ - PCOS and pregnancy.
https://www.pregnancybirthbaby.org.au/pcos-and-pregnancy#complications - Eclampsia
https://www.yalemedicine.org/conditions/eclampsia#:~:text=Eclampsia%20typically%20occurs%20when%20a,normal%20throughout%20pregnancy%20and%20postpartum. - Leslie V Farland, et al.; (2022); Polycystic ovary syndrome and risk of adverse pregnancy outcomes: a registry linkage study from Massachusetts
https://pmc.ncbi.nlm.nih.gov/articles/PMC9627555/ - Susan M Sirmans, Kristen A Pate; (2013); Epidemiology, diagnosis, and management of polycystic ovary syndrome
https://pmc.ncbi.nlm.nih.gov/articles/PMC3872139/ - Polycystic Ovary Syndrome (PCOS).
https://www.hopkinsmedicine.org/health/conditions-and-diseases/polycystic-ovary-syndrome-pcos - Polycystic ovarian syndrome (PCOS).
https://www.betterhealth.vic.gov.au/health/conditionsandtreatments/polycystic-ovarian-syndrome-pcos#long-term-health-risks-of-pcos - Polycystic ovary syndrome (PCOS).
https://www.stclair.org/services/mayo-clinic-health-information/diseases-and-conditions/CON-20314571/ - Anderson Sanches Melo et al; Treatment of infertility in women with polycystic ovary syndrome: approach to clinical practice.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4642490/ - Polycystic Ovary Syndrome.
https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/treatment/ - Polycystic Ovary Syndrome (PCOS)
https://my.clevelandclinic.org/health/diseases/8316-polycystic-ovary-syndrome-pcos - Anne Engtrø Husby, et al.; Childbirth experiences in women with polycystic ovary syndrome: A cohort study
https://obgyn.onlinelibrary.wiley.com/doi/10.1111/aogs.14800 - PCOS Pregnancy and Delivery Complications.
https://www.pcosaa.org/pcos-pregnancy-and-delivery-complications - Amandeep Mann et al.; (2020); Pregnancy Outcome in Women with Polycystic Ovary Syndrome.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7515985/ - Polycystic ovary syndrome.
https://womenshealth.gov/a-z-topics/polycystic-ovary-syndrome - Deepshikha Thakur et al.; (2021); Effect of yoga on polycystic ovarian syndrome: A systematic review.
https://www.sciencedirect.com/science/article/abs/pii/S1360859221000413
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Karla S. Sanchez-Banos
Read full bio of Dr Bisny T. Joseph
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das