Image: iStock
Human papillomavirus (HPV) is a causative agent of sexually transmitted infections. Genital HPV infection is common, with 75% of sexually active adults being exposed to the infection at least once in their lifetime (1).
Most HPV infections are asymptomatic (2). However, the mild immunosuppressed stateiA state in which the body has weak immunity or the ability to fight against infections mainly due to the effect of medications and hormonal shifts during pregnancy may cause a woman to develop symptoms of HPV infection in pregnancy (3). Read on to know more about the symptoms, risk factors, treatments, and preventive measures for HPV infection during pregnancy.
Key Pointers
- Human papillomavirus (HPV) is a sexually transmitted disease (STD) in pregnant women.
- Most women are asymptomatic; however, you must report to your doctor if you notice lesions, bumps in the privates, or vaginal bleeding and itching.
- History of STDs, having multiple sex partners, and a weakened immune system during pregnancy might increase the risk of developing HPV.
- Practicing safe sex, monogamy, and getting vaccinated against HPV are effective measures to prevent this infection during pregnancy.
Symptoms Of HPV Infection
HPV infections are mostly asymptomatic. The most common symptoms of the infection are wartsiA small, painless bump on the skin caused by viruses and can spread from one part of the body to the other , which may appear on any part of the body. Warts that appear inside or outside the genitals or anus usually indicate a sexual transmission of HPV.
- Other common symptoms of HPV infection are (4) (5):
- Flat lesions that appear like spots
- Bump-like projections with abnormal appearance
- Itching or burning sensation in the genital region
- Vaginal bleeding during or after a sexual intercourse
 Things to know
Things to know
These symptoms may be present in other conditions, such as other sexually transmitted infections. Certain types of HPV may increase the risk of cancer of the cervix, vagina, anus, throat, and mouth. Therefore, see a doctor to determine the underlying cause.
Mode Of Transmission Of HPV Infection
HPV infection occurs due to any of the more than 100 types of human papillomaviruses
(5). The HPV virus can pass from the infected person through the following ways (6) (7).
- Vaginal, oral, or anal sex
- Touching warts of an infected person
- Touching contaminated objects, such as a doorknob
HPV transmission can occur even when the person with the virus has no symptoms. The most common symptoms of HPV infection are warts, which may not appear for weeks to months after infection (5).
 Things to know
Things to knowRisk Factors Of HPV Infection In Pregnancy
The following factors may increase the risk of developing HPV infection during pregnancy.
- Sexual activity: Women who are sexually active during pregnancy may have a higher risk of contracting the virus.
- Multiple sex partners: Women with multiple sex partners are at an increased risk of developing sexually transmitted infections, such as HPV infection.

- Weakened immunity: Stress, diabetes, and certain medicines may weaken your immunity and affect maternal health, making you susceptible to infections, such as an HPV infection.
- Past infections: You may be at a higher risk of developing HPV infection if you have had previous viral infections, such as HSV (herpesi A group of viruses that cause painful blisters or sores around the genitals, mouth, or rectum ) infection.
- Age: A study noted that women younger than 25 years might be at a higher risk of contracting HPV infection during pregnancy (8). More research is needed to establish the link between age and the risk of infection.
Diagnosis Of HPV Infection During Pregnancy
Testing for HPV infections is usually not done during pregnancy. However, if your doctor suspects any signs of infection in you or detects any presence of warts during a routine screening, they may screen you for HPV infection with the following tests (5) (9).
- Pelvic examination: Your OB/GYN will perform a pelvic (cervical) exam to visualize the presence of warts externally.
- PAP test: Pap smear test is useful to determine abnormalities in cervical cells. The sample is taken from your cervix and examined for infection. The test is widely used to detect cervical cancers.

- Colposcopy: This test is used to visualize genital warts or abnormal cervical cells. Your gynecologist may suggest a biopsy to check for cervical abnormalities.
- Molecular testing (HPV DNA test): A HPV DNA test is done after your doctor detects an abnormal pap test and confirms the presence of genital warts. It is an additional test to evaluate high-risk HPV infections that may lead to cancers.
Treatment For HPV Infection During Pregnancy
There is no cure known for HPV infection, and the virus stays in the body forever (10). Nevertheless, in most cases, the immune system subdues the effects of the virus, relieving the symptoms of the infection.
HPV treatments are usually directed towards managing symptoms or excision of warts and may include the following (11)
- Cryotherapy: A technique used to freeze warts or abnormal cervical cells, usually with liquid nitrogen.
- Laser removal: This method uses high-intensity light to destroy abnormal cells or tissues.
- Electrical removal(electrocautery): This is a procedure to burn off the infected tissues and warts with the heat of an electric cutter.

- Surgery: Surgical procedures, such as small excisions, cold knife cones (CKC)i A surgery in which an abnormal cone-shaped tissue is removed from the cervix with a laser knife. , and loop electrosurgical excision (LEEP)iA surgery in which a heated wire loop is used to remove abnormal cells from the tissue of the cervix , may be used to remove harmful tissues and prevent the development of malignancies.
- Topical medications: Your doctor may prescribe certain medicated creams to apply on warts. You may note that the use of certain medications is contraindicated in pregnancy. Therefore, do not use any over-the-counter medicines for warts.
Your doctor may choose suitable treatment modalities based on the severity of infection’s symptoms and stage of pregnancy and after considering possible risks and complications.
Prevention Of HPV Infection In Pregnancy
Infection from certain types of human papillomaviruses can be prevented through the HPV vaccine. Make sure to get vaccinated before you conceive for the best protection. As per CDC, HPV vaccination is recommended for everyone before the age of 26. If you are older than 26, speak to your healthcare provider or obstetrician before getting the vaccine.
You can observe the following precautions to avoid the risk of infection during pregnancy (12) (13).
- Have safe sex: Make sure to use condoms during sexual intercourse to reduce the chances of acquiring HPV and other sexually transmitted infections. A study noted that condoms during sex could reduce the risk of HPV infection by 70% in women (14).

- Practice monogamy: Having multiple sex partners can increase your risk of acquiring sexually transmitted infections such as HPV infection.
- Discuss the risks of STIs with your partner: Be sure to know if your partner has any history of sexually transmitted infections before having sex (15).
 Caution
CautionFrequently Asked Questions
1. Can HPV cause infertility?
Studies suggest that HPV infection could be a risk factor for infertility but not the only cause. Further research is needed to evaluate the role of HPV in causing female infertility (16).
2. Can a woman with HPV give birth naturally?
It is possible to have a natural birth with HPV. However, your doctor will suggest the type of delivery based on the severity of the infection. Your doctor may suggest a cesarean or C-section delivery if the genital lesions obstruct the birth canal or are at the risk of rupturing during delivery (17).
3. Can HPV be transmitted during childbirth?
Studies have shown that a woman with an HPV infection may pass the infection to the fetus during birth (18). It may lead to infection symptoms, such as warts in babies.
4. Does HPV increase the risk of miscarriage?
HPV infection during pregnancy might be associated with certain pregnancy complications such as miscarriage, restricted fetal growth, low birth weight, and preterm birthiA birth that takes place three weeks before the normal due date or the 37th week of pregnancy (19).
5. Does HPV get worse during pregnancy?
The various hormonal changes that the body undergoes during pregnancy may make HPV worse (20). However, in some cases, the hormonal changes may make the virus less active, decreasing the risk of HPV-related complications.
HPV infection during pregnancy may be asymptomatic in some women, while others may have noticeable symptoms. Speak to your doctor if you suspect you have symptoms of HPV infection. Early detection may help avoid complications, including certain types of cancers. Vaccine and precautions may usually help avoid the infection in most women.
Infographic: HPV Infection Risk Factors In Pregnancy
HPV infections can spread from one to another through unsafe sex, coming in contact with HPV warts, or touching contaminated objects. However, it is generally asymptomatic, but it may affect pregnancy. Therefore, checking for HPV infection and taking the HPV vaccine before conception is recommended. Check out the infographic below to learn about the risk factors and diagnostic tests for HPV infection in pregnancy. Illustration: Momjunction Design Team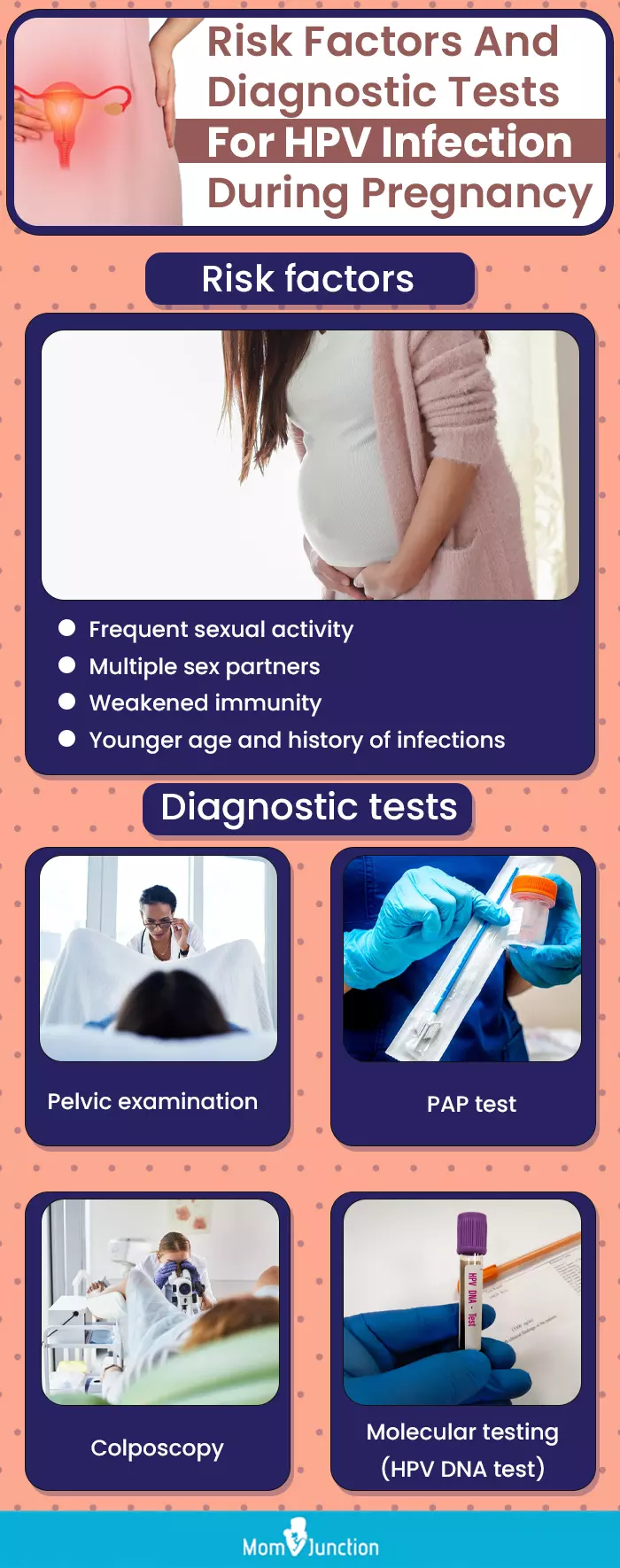
Illustration: HPV During Pregnancy: Symptoms Risks Factors And Treatment

Image: Dall·E/MomJunction Design Team
Pregnancy is a special time for many women, but HPV can affect it. What the video to know how HPV can affect your pregnancy and what you can do.
References
- Ankit H. Bharti, et al.; (2013); An update on oral human papillomavirus infection.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3841675/ - DeekshaPandey, et al.; (2019); Human Papillomavirus (HPV) Infection in Early Pregnancy: Prevalence and Implications.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6451823/ - S. Bandyopadhyay and R Chatterjee; (2006); HPV viral load determination during pregnancy as a possible cervical cancer risk.
https://pubmed.ncbi.nlm.nih.gov/16761615/ - HPV During Pregnancy.
https://americanpregnancy.org/healthy-pregnancy/pregnancy-concerns/hpv-during-pregnancy/ - Genital warts.
https://medlineplus.gov/ency/article/000886.htm - About Genital HPV Infection; CDC
https://www.cdc.gov/sti/about/about-genital-hpv-infection.html?CDC_AAref_Val=https://www.cdc.gov/std/hpv/stdfact-hpv.htm - How to get rid of warts.
https://www.health.harvard.edu/diseases-and-conditions/how-to-get-rid-of-warts - P. Liu et al.; (2014); The prevalence and risk of human papillomavirus infection in pregnant women.
https://www.cambridge.org/core/journals/epidemiology-and-infection/article/prevalence-and-risk-of-human-papillomavirus-infection-in-pregnant-women/27A4494461AFF1D0418382DBB9041360 - S. Arena, et al.; (2002); HPV and pregnancy: diagnostic methods, transmission and evolution.
https://pubmed.ncbi.nlm.nih.gov/12063438/ - Jon K. Hathaway; (2012); HPV: diagnosis, prevention, and treatment.
https://pubmed.ncbi.nlm.nih.gov/22828099/ - Lynette Luria, Gabriella Cardoza-Favarato; (2021); Human Papillomavirus.
https://www.ncbi.nlm.nih.gov/books/NBK448132/ - HPV (Human Papilloma Virus).
https://my.clevelandclinic.org/health/diseases/11901-hpv-human-papilloma-virus - Genital Warts (Human Papillomavirus).
https://www.uofmhealth.org/health-library/hw105401 - Consistent Condom Use Lowers Risk Of HPV Infection.
https://acsjournals.onlinelibrary.wiley.com/doi/full/10.3322/canjclin.56.6.319 - HPV Vaccination Recommendations.
https://www.cdc.gov/vaccines/vpd/hpv/hcp/recommendations.html - Shuang Yuan. et al.; (2019); Human papillomavirus infection and female infertility: a systematic review and meta-analysis.
https://pubmed.ncbi.nlm.nih.gov/31987733/ - P. Singhal, et al; (2009); Pregnancy and sexually transmitted viral infections
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3168062/ - SeungMi Lee, et al.; (2013); Risk of Vertical Transmission of Human Papillomavirus throughout Pregnancy: A Prospective Study.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3681772/ - Victor N Chilaka, et al.; (2021); Human papillomavirus (HPV) in pregnancy – An update.
https://www.ejog.org/article/S0301-2115(21)00397-3/fulltext - Deeksha Pandey et al.; (2019); Human Papillomavirus (HPV) Infection in Early Pregnancy: Prevalence and Implications.
https://www.hindawi.com/journals/idog/2019/4376902/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Pamela Adhiambo Muga
Read full bio of Vidya Tadapatri
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das