Image: Shutterstock

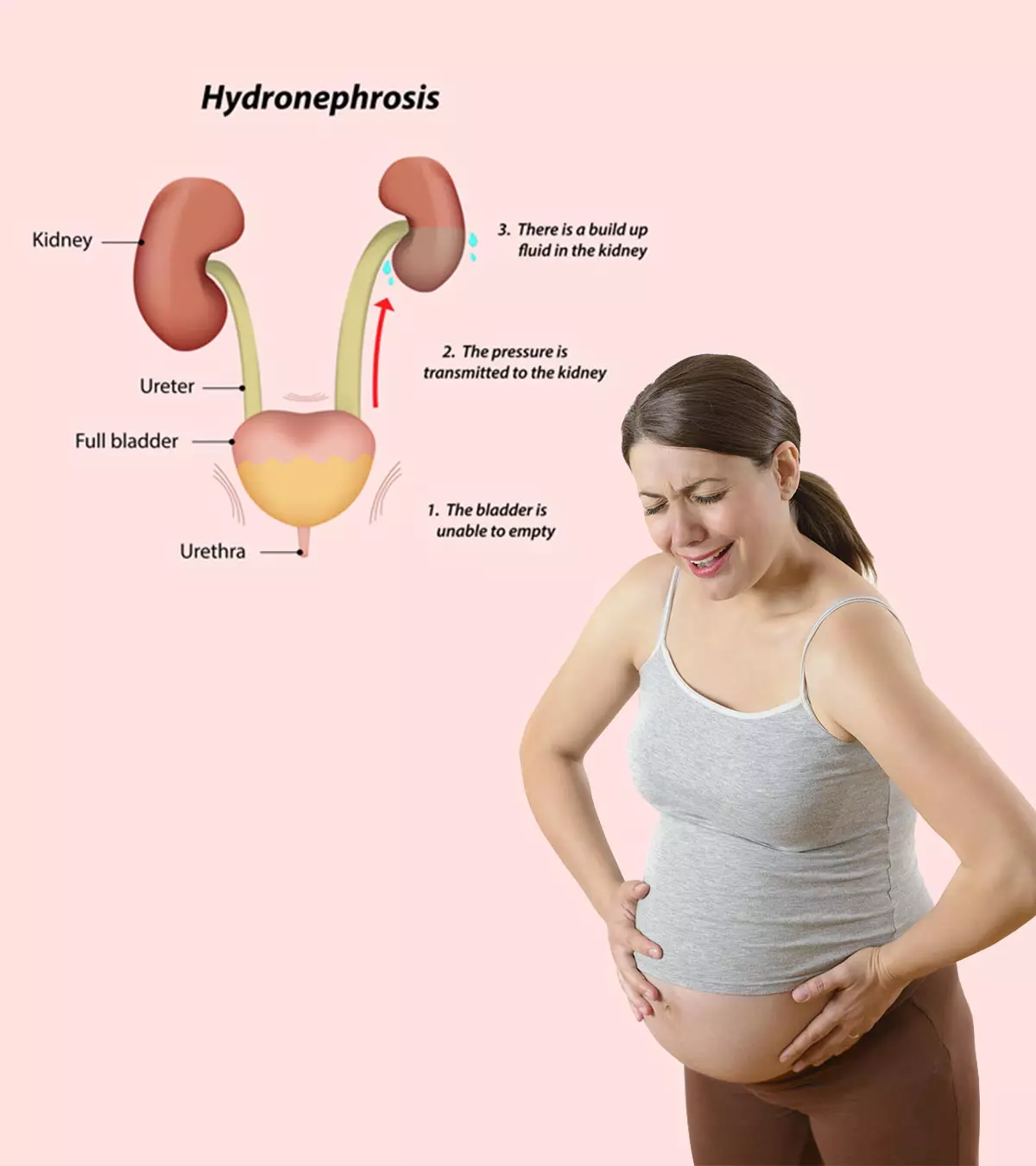
Hydronephrosis during pregnancy refers to the swelling of the kidney due to the accumulation of urine, and the condition is known to affect 90% of pregnant women (1). In this condition, the kidney swells up as the urine is unable to pass through it and reach the bladder due to urinary tract obstruction or blockage. You must consult your doctor immediately if you notice hydronephrosis symptoms to prevent further complications. Read on to know more about hydronephrosis, including its causes, signs and symptoms, treatment, and prevention options.
Key Pointers
- Hydronephrosis is when the kidney swells due to urine backup, and it is common during pregnancy.
- Symptoms of hydronephrosis include nausea, vomiting, fever, blood in urine, and swollen legs.
- Some of the causes of maternal hydronephrosis are hormonal imbalance, kidney stones, blood clots, and diabetes.
- Hydronephrosis during pregnancy can cause preterm labor and may lead to kidney failure if left untreated.
- After childbirth, hydronephrosis usually resolves on its own. However, if you experience recurring symptoms, speak to your doctor.
What Is Hydronephrosis In Pregnancy?
Hydronephrosis in pregnancy is not a disease. It is a structural condition that typically occurs in one kidney or can affect both kidneys in chronic cases. The failure of normal urine drainage from the kidney to the urinary bladder can result in the swelling of either one of the kidneys or both. This condition commonly refers to hydronephrosis. It may happen as a normal physiological variant or an underlying illness.
When the swelling affects one of the kidneys, it is called Unilateral Hydronephrosis. While, when both the kidneys are simultaneously affected, the disorder is called Bilateral Hydronephrosis (2).
Hydronephrosis can occur during pregnancy and is known as maternal/gestational hydronephrosis. The asymptomatic dilation of the renal calyces, the renal pelvis, and the upper two-thirds of ureters during pregnancy results in this typical condition.
 Quick fact
Quick factGestational hydronephrosis is often associated with a urinary tract infection or UTI during pregnancy. It is estimated that around 90% of pregnant women may suffer from some form of hydronephrosis or urinary retention during pregnancy. However, they are mostly asymptomatic. The symptomatic hydronephrosis only occurs in about 0.2-3% of these cases and may become symptomatic in later stages of pregnancy (3). The existence of hydronephrosis due to some pathological condition prenatally worsens the disorder (1).
Facts About Hydronephrosis In Pregnancy
- Gestational hydronephrosis usually occurs during the second trimester. It typically happens around 26 to 28 weeks of pregnancy when the uterus is larger and may compress the urinary system (3).
- Nulliparous patients are more likely to develop severe hydronephrosis. (A woman who has not carried the pregnancy beyond 20 weeks is termed nulliparous). Additionally, the occurrence of anemia in pregnant women can further increase the risk of developing urosepsis, a severe complication of hydronephrosis in pregnancy (8).
- Usually, gestational hydronephrosis is asymptomatic and disappears independently without any form of treatment. The ideal period is six weeks after delivery, but sometimes, it may persist longer (1).
The graphical representation below illustrates the outcomes of a study conducted on 58 expectant mothers experiencing different levels of symptomatic ureterohydronephrosisiA condition in which ureters and kidneys swell due to a blockage in the urine flow . The results corroborate that maternal ureterohydronephrosis is a common anatomical modification during pregnancy. Also, its prevalence varies based on gestational age, with a higher frequency observed during the second and third trimesters (9).

Distribution of hydronephrosis cases according to gestational age
Source: Early diagnosis of maternal ureterohydronephrosis during pregnancy; Experimental and Therapeutic MedicineSymptoms Of Hydronephrosis

Image: Shutterstock
Symptoms vary based on the severity of the condition. Some women may have mild symptoms, while others may have none. Here are some typical symptoms of hydronephrosis during pregnancy (4) (2) (5):
- Acute flank pain or pain in the back and abdominal region, particularly at the right side
- Tenderness at the right kidney
- Nausea and vomiting
- Constant urinary tract infection with painful urination
- Fever
- Colicky painiA sudden, intense, spasm-like stomach ache that can strike suddenly and is recurrent.
- Stains of blood in the urine or hematuria
- Chest pain
- Swelling of the legs
- Increased frequency of urination due to inability to empty bladder completely
- Increased urgency of urination
- More or less urine than normal
Causes Of Hydronephrosis During Pregnancy
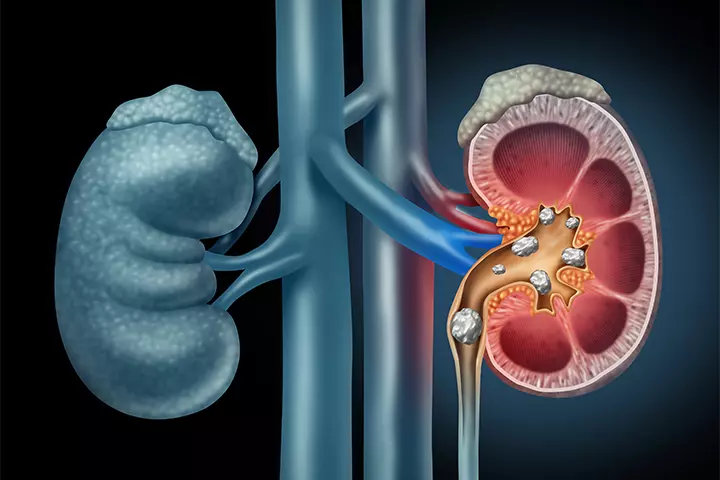
Image: IStock
Pregnancy itself is the primary cause of maternal hydronephrosis, which can result from various physiological changes that occur during this time. These changes include (6) (3):
- Increased urine volume
- Increased uterus pressure due to the growing baby
- Uteral compression due to twin pregnancy
- Ovarian veins dilation
- Enlargement of urinary tract
- Generalized relaxation of smooth muscles due to progesterone
- Constipation
Some other causes of hydronephrosis that are not related to pregnancy are (7):
- Kidney stones
- Blood clots
- Stricture or scarring of the kidneys
- Bladder cancer
- Urethral stricture
- Diseases causing inflammation of the uterus, such as UTI
- Existing medical conditions such as ovarian vein syndromeiAn unusual syndrome when the dilated ovarian vein leads to an obstruction of the ureter. , diabetes, and vesicoureteral refluxiA disorder when the urine flows backward via one or both ureters and reaches the kidney
Sharing about her hydronephrosis diagnosis during pregnancy, Natalia, a mother and blogger, says, “I started out my pregnancy with Typhoid feveriA fatal bacterial infection caused by the Salmonella Typhi bacteria . A couple of months later I was hit with Malaria…and Typhoid at the same time. (To be clear, I wash my hands, drink filtered water, wash clothes a lot, and stay in a mosquito net when it starts to get dark or too buggy. But sometimes, even the best prevention leaves you defeated.)
“As soon as I arrived in the States for a visit, I ended up in the hospital with severe pain and multiple doctors taking days to find the right answer… My ureter is basically kinked like a hose and fluid has filled up around my kidney. I guess the official term for this is Hydronephrosis. It can be caused by anything from stones to tumors and yes, you guessed it: pregnancy (i).”
 Quick fact
Quick factDiagnosing Hydronephrosis During Pregnancy

Image: Shutterstock
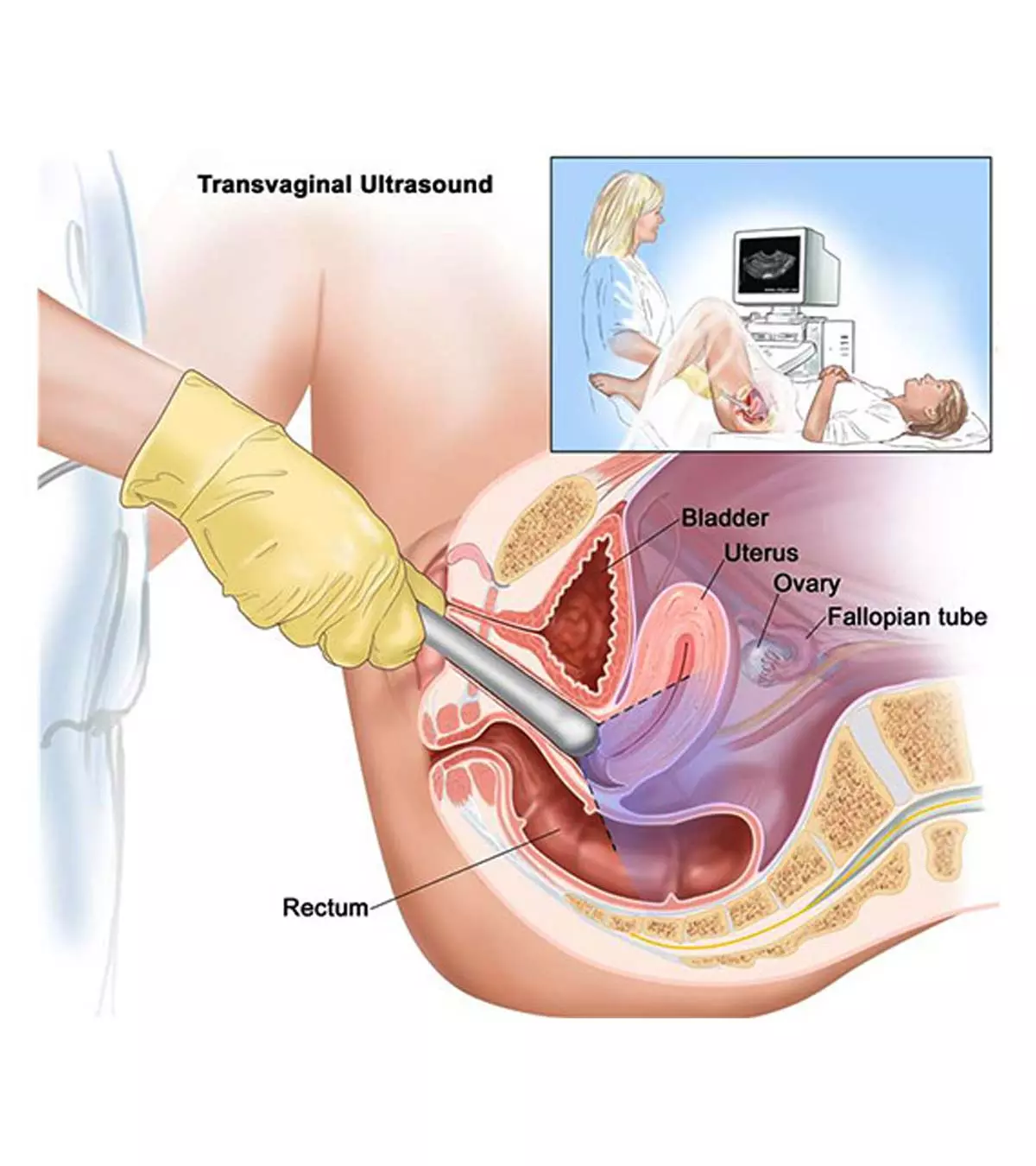
Diagnosis of hydronephrosis during pregnancy includes (2):
- Physical examination, where the doctor will ask about your symptoms, medical and family history, and examine your kidney area.
- Urine analysis to determine an infection.
- Blood test to check for anemia.
- Renal function test to detect the proper functioning of kidneys.
- Ultrasound scan to differentiate physiological hydronephrosis from obstruction secondary to renal stones/calculus.
In rare cases, doctors may suggest advanced imaging techniques such as MRI or CT scans.
Risks Associated With Gestational Hydronephrosis
The obstetric complications and risks due to gestational hydronephrosis include urosepsisiA life-threatening condition when the urinary tract infection spreads to the kidneys and causes sepsis. , preterm labor and delivery and pyelonephritisiA bacterial infection of the kidneys. (3). A very rare but potentially life-threatening complication associated with severe gestational hydronephrosis is a spontaneous renal rupture. It occurs due to increased hydrostatic pressure within the collecting structures that exceed the holding capacity of the calyceal-renal capsular junctions (10).
Kidneys with prior damage before pregnancy are more susceptible to suffering from a spontaneous renal rupture. If left untreated beyond a reasonable period, the kidney will permanently fail to function, leading to renal failure (7). However, regular monitoring and immediate treatment can help prevent long-term renal damage.
When To Seek Medical Assistance
An incidence of fever, acute pain in the abdomen, traces of blood in the urine, bladder dysfunction, or any other urological complications are all pointers to seek medical help immediately. Hydronephrosis can be fatal in pregnant women with just one kidney. Therefore, the development of slight symptoms, even in the case of a single kidney, should be brought to the attention of your doctor immediately.
Treatment For Hydronephrosis During Pregnancy
The treatment of symptomatic gestational hydronephrosis during pregnancy is carefully performed through different stages. Take a look at them (3).
1. Most cases with mild symptoms of gestational hydronephrosis with normal renal function can be treated conservatively. Some conservative treatments include regular analgesics, proper hydration, a left lateral position while sleeping, and treating urinary tract infections, if any.
2. Draining the urine through a thin catheter inserted into the bladder or directly to the kidney through the skin under local anesthesia relieves the pressure on the kidneys.
3. Treating the underlying cause, which primarily caused the blockage, is the next line of management. A surgery called ureteral stentingiA procedure involving the insertion of a thin and flexible tube into the ureter for the treatment or prevention of blockages in the urinary tract usually removes the obstruction. However, it is only required in cases of severe hydronephrosis.
4. Different causes will have different treatments. For instance, if a large kidney stone triggers hydronephrosis, sound waves or lasers are used to break it (11). In severe cases leading to kidney failure, your obstetrician may suggest dialysis.
Dani Tippet, a first-time mother shares, “My second trimester was one I was looking forward to, as many women enjoy this part of pregnancy most. Unfortunately, I was greeted with excruciating pain caused by a kidney condition called hydronephrosis. I worked through this pain from my 25th week in pregnancy, up until my 33rd week. At that point, my urologist recommended I undergo surgery to relieve the pain and pressure I was experiencing for the safety and comfort of both myself and my baby (ii)”
Prevention Of Hydronephrosis During Pregnancy

Image: Shutterstock
Kidney diseases often have no/mild symptoms. Hence, it can go undetected if not tested at the right time. Early detection and treatment can slow or prevent the progression of kidney disease. A regular urine test and blood test can help us in finding the prevalence of any kidney disorders in pregnancy (12). Some preventive measures you should keep in mind are:
- Drink enough water
- Eat a well-balanced diet, especially plant-based protein
- Attend prenatal checkups timely
- Manage blood glucose level and blood pressure
- Treat urinary tract infections
- Exercise regularly
- Manage any existing conditions effectively
- Be careful with pain medications
Frequently Asked Questions
1. Is hydronephrosis in the fetus serious?
Untreated hydronephrosis may result in complications such as kidney stones, urinary tract infections, and chronic kidney disease (14).
2. Which side of the body is most prone to hydronephrosis during pregnancy?
Hydronephrosis during pregnancy is more prominent on the right than on the left due to the changes that happen during pregnancy, such as rotation of the uterus and engorgement of the ovarian veins (15).
3. How often should women with hydronephrosis during pregnancy be monitored by a healthcare provider?
The number of times a doctor should monitor a woman with hydronephrosis during pregnancy varies and relies on several factors, such as the individual’s health, the severity of the condition, and the underlying cause. Generally, women with hydronephrosis during pregnancy are monitored regularly to ensure the well-being of the mother and the baby.
4. Should I worry if I’m diagnosed with fetal hydronephrosis?
Obstetrician and gynecologist Dr. Himali Maniar Patel says, “Fetal hydronephrosis refers to the swelling of a baby’s kidney due to urine buildup. While it can be alarming when first diagnosed, it is a relatively common finding in pregnancy. In many cases, fetal hydronephrosis is mild and resolves without causing long-term issues.”
Hydronephrosis during pregnancy is common and mostly resolves after childbirth without requiring specific treatment. It refers to the inability of the kidneys to drain the urine. This could be due to the growing fetus taking up space in the abdominal cavity and the changes in the hormone levels. It may cause flank pain, fever, or blood in the urine. It may cause concern if associated with renal stones, urinary tract infections, or other underlying kidney conditions. Discuss with your doctor if you observe any symptoms of hydronephrosis and ensure not to miss prenatal check-ups as they are essential for the early diagnosis.
Infographic: How To Keep Your Kidneys Healthy During Pregnancy?
Pregnancy induces changes in all aspects of kidney functions, including increased glomerular filtration rate and renal plasma flow. Regular prenatal checkups and controlling certain pregnancy complications are necessary to avoid kidney damage. Follow the tips given in the infographic below to promote kidney health during pregnancy. Illustration: Momjunction Design Team
Are you unable to pass urine through your bladder during your pregnancy? You could be suffering from Hydronephrosis. Watch this video to know how specialists cater to you and your unborn child’s well-being.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. The Pregnant Woman’s Guide to Hydronephrosis and Stents;
https://thesteepingslough.wordpress.com/2016/08/19/the-pregnant-womans-guide-to-hyrdonephrosis-and-stents/
ii. A first time mother’s birth story;
https://medium.com/fearless-she-wrote/a-first-time-mothers-birth-story-64be92676f09
References
- Maternal Hydronephrosis in Pregnancy.
https://radiopaedia.org/articles/maternal-hydronephrosis-in-pregnancy - Hydronephrosis.
https://my.clevelandclinic.org/health/diseases/15417-hydronephrosis - Mohannad Hosny et al.; (2025); The Management of Symptomatic Hydronephrosis in Pregnancy.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10784716/ - Hydronephrosis of one kidney.
https://medlineplus.gov/ency/article/000506.htm - Frank Rohde Nielsen and Per Emil Rasmussen; (1988); Hydronephrosis during pregnancy: four cases of hydronephrosis causing symptoms during pregnancy.
https://www.ejog.org/article/0028-2243(88)90129-3/pdf - Barış Saylam et al.; (2025); Clinical Course of Pregnant Women with Maternal Hydronephrosis: Retrospective Clinical Study.
https://dergipark.org.tr/en/download/article-file/1709194 - Hydronephrosis.
https://www.kidney.org/kidney-topics/hydronephrosis-0 - Viorel Dragos Radu et al.; (2025); Factors Associated with Increased Risk of Urosepsis during Pregnancy and Treatment Outcomes, in a Urology Clinic.
https://pmc.ncbi.nlm.nih.gov/articles/PMC10673142/ - Elena Ciciu et al.; (2025); Early diagnosis and management of maternal ureterohydronephrosis during pregnancy.
https://www.spandidos-publications.com/10.3892/etm.2025.10949 - KL Lo et al.; (2007); Spontaneous rupture of the left renal collecting system during pregnancy.
https://www.hkmj.org/system/files/hkm0710p396.pdf - Hydronephrosis.
https://www.nhs.uk/conditions/hydronephrosis/treatment/ - P E Rasmussen and F R Nielsen; (1988); Hydronephrosis during pregnancy: a literature survey.
https://pubmed.ncbi.nlm.nih.gov/3280355/ - How to Prevent Kidney Disease.
https://www.kidney.org/news-stories/how-to-prevent-kidney-disease - Hydronephrosis in Newborns.
https://pubmed.ncbi.nlm.nih.gov/3280355/ - Debasmita Mandal et al.; (2017); Urological disorders and pregnancy: An overall experience.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5308034/#
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Arpita Chakraborty
- Dr. Himali M Patel is an Ahmedabad, India based gynecologist with 13 years of experience. She currently practices at Nisha Women's Hospital and IVF Centre. Dr. Patel did her graduation in Medicine at Bharati Vidyapeeth University, Pune and holds a diploma in Obstetrics and Gynecology.
 Dr. Himali M Patel is an Ahmedabad, India based gynecologist with 13 years of experience. She currently practices at Nisha Women's Hospital and IVF Centre. Dr. Patel did her graduation in Medicine at Bharati Vidyapeeth University, Pune and holds a diploma in Obstetrics and Gynecology.
Dr. Himali M Patel is an Ahmedabad, India based gynecologist with 13 years of experience. She currently practices at Nisha Women's Hospital and IVF Centre. Dr. Patel did her graduation in Medicine at Bharati Vidyapeeth University, Pune and holds a diploma in Obstetrics and Gynecology.
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das