Image: Shutterstock
Hydronephrosis in babies is a condition where urine gets trapped in the kidney and drains slower than it should into the bladder.
It is a common congenital condition and may affect one in 500 babies (1). However, it may also develop later in life for some babies. Further, it is more common in boys than girls (2).
Hydronephrosis can be diagnosed before birth (prenatal) or after birth (postnatal). It is treatable, and mild cases resolve without intervention (2).
Read this post to learn about the causes, symptoms, diagnosis, and treatment of hydronephrosis in babies.
Key Pointers
- Hydronephrosis in babies could be transient or chronic and may occur due to narrowing of a part of the urinary tract, congenital defects, or neurogenic bladder.
- Moderate to severe hydronephrosis may cause abdominal pain, urinary tract infection, or hematuria (blood in the urine).
- It can be diagnosed after 20 weeks of pregnancy or during the routine examination after birth.
- The treatment modality relies on the cause, severity of the condition, and whether one or both kidneys are affected.
- Mild hydronephrosis in babies can resolve itself, but if left untreated, moderate or severe cases could lead to complete renal failure.
What Is Hydronephrosis In Newborns?
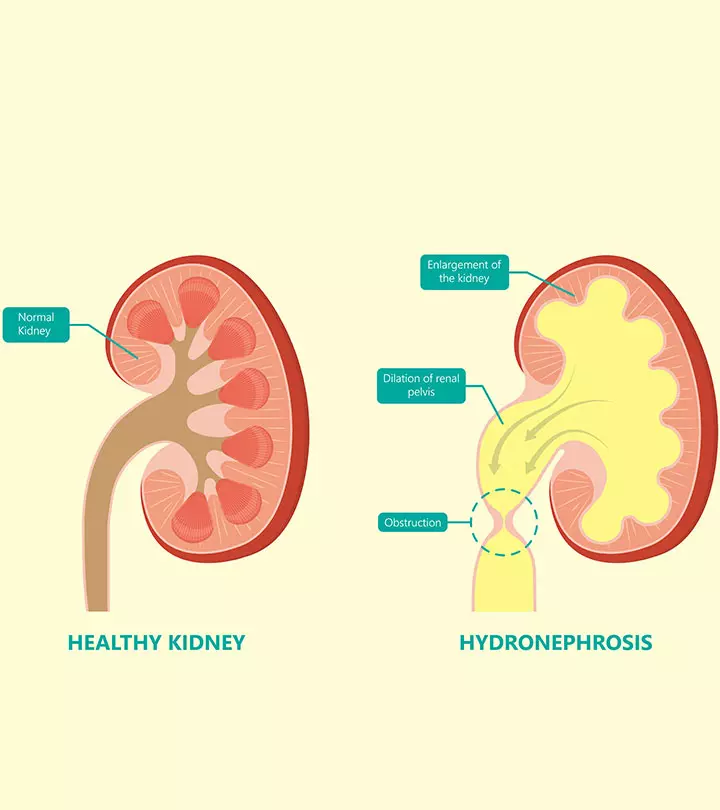
Hydronephrosis is defined as the enlargement or dilation of either one or both kidneys due to urine build-up (3). The condition is also known as urinary tract dilation (UTD). It usually occurs when the urine cannot drain out from the kidney to the bladder due to an obstruction or blockage. The blockage could occur anywhere in the urinary tract — the opening of the kidneys, the ureters, the bladder, or the urethra (3). Some other problems could also cause the accumulation of urine within the kidneys.
The condition is often diagnosed before birth during prenatal scans (2). Additionally, the severity varies from mild to severe depending on the extent of the blockage.
 Did you know?
Did you know?What Causes Hydronephrosis?

Image: Shutterstock
Some cases of hydronephrosis in babies may not have a definite cause, and it resolves on its own. This is referred to as transient hydronephrosis (2). However, in other cases, it occurs primarily due to a blockage in the urinary tract or backflow of the urine from the bladder to the kidney (2).
Below are some of the conditions that could lead to obstruction in the urinary tract or reversal of the urine flow, leading to urine accumulation in one or both kidneys (1) (2).
- Narrowing of a part of the urinary tract: It is often observed in transient hydronephrosis and occurs during the fetus’ early development. It resolves on its own as the urinary tract becomes mature.
- UPJ (ureteropelvic junction) obstruction: It is a blockage at the site where kidneys and ureters meet. It is one of the common causes of hydronephrosis in babies.
- UVJ (ureterovesical junction) obstruction: It is blockage at the site where the ureters connect to the bladder.
- Posterior urethral valves (PUV) obstruction: It happens when there are abnormal pieces of tissues within the prostatic urethra (the part of the urethra that passes through the prostate gland). It only occurs in boys.
- Ureterocele: The ureters do not develop normally and form a small pouch, which causes obstruction.
- Vesicoureteral reflux (VUR): It happens when muscles at the junction of the ureters and bladder do not function correctly, causing urine backflow to the kidneys. It is one of the common causes of hydronephrosis in babies.
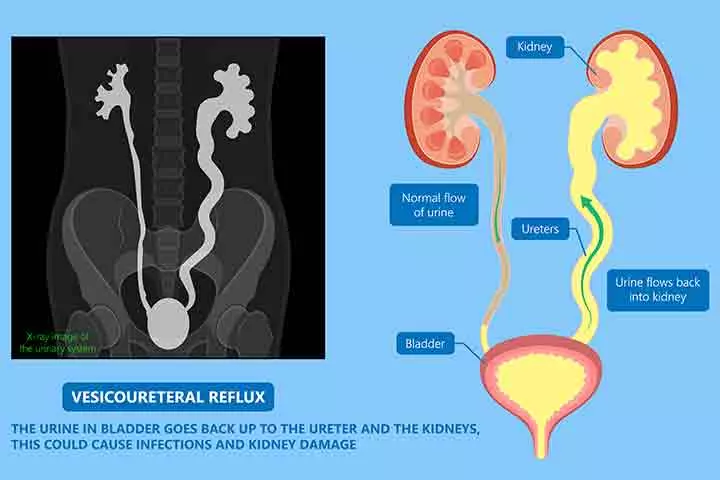
Image: Shutterstock
- Ectopic ureter: The ureters do not terminate at the bladder, causing the urine to flow outside the bladder.
- Neurogenic bladder: It develops when nerves between the bladder and the brain do not relay messages correctly.
- Congenital defects: Certain birth defects increase the risk of hydronephrosis in babies. An example is prune belly syndrome, a birth defect where the infant is born without abdominal muscles, leading to urinary tract malfunctions and other complications.
 Quick fact
Quick factRisk Factors For Hydronephrosis
There are no definite risk factors for hydronephrosis. Mild hydronephrosis does not have a genetic cause and is not hereditary (4). If the cause of hydronephrosis in the first child is ureteropelvic junction (UVJ) blockage, then the chances of its occurrence are as high as 50% in future children.
In some cases, certain genetic conditions can cause the development of cysts in the kidneys, leading to the accumulation of urine, which detrimentally affect renal function. If the first child develops hydronephrosis for this reason, there is a 25% chance of hydronephrosis in future children (4).
Signs Of Hydronephrosis In Babies
Mild hydronephrosis may not cause any symptoms, and it may resolve on its own without causing any discomfort to the baby (5).
Moderate to severe hydronephrosis could cause the following signs and symptoms (2) (5).
- Abdominal pain

Image: Shutterstock
- Swollen abdomen due to severe blockage
- Flank pain (pain on the sides of the torso)
- Urinary tract infection (UTI); its symptoms include painful urination, cloudy urine, back pain, fever, and vomiting
Multiple UTIs in babies with or without fever may indicate obstruction or reflux in the urinary system (5). Consult a doctor if symptoms worsen or you notice unusual behavioral changes in your baby.
Diagnosis Of Hydronephrosis
Hydronephrosis can be detected during pregnancy using routine prenatal ultrasound checks (5). Doctors may diagnose the condition after 20 weeks of pregnancy when the kidneys’ size is larger than before, and they produce urine.
Postnatal diagnosis may occur during the routine examination after birth. The condition could also be diagnosed later during routine checks, and it is likely to be the case when hydronephrosis is not congenital. The following steps and procedures could be used for diagnosis (1) (2).
- Physical examination to detect an abdominal lump, which could indicate an enlarged/swollen kidney or bladder.
- Renal ultrasound scans check for swelling and blockage.
- Voiding cystourethrogram is an imaging technique that uses an X-ray to visualize how urine flows through the bladder and urethra.
- Radionuclide (dimercaptosuccinic acid (DMSA)) scans use small quantities of radioactive material to visualize the functions of the urinary system.
The doctor will suggest appropriate tests based on the baby’s symptoms and the results of other tests.

Image: Shutterstock
Treatment For Hydronephrosis In Babies
The treatment depends on the following factors (2).
- The severity of the condition
- Whether one or both kidneys are affected
- Cause of hydronephrosis
The doctor may suggest any of the following treatment methods after considering the factors (6).
- Intervention during pregnancy: In rare cases, the condition may become so severe that the fetus may be unable to empty the bladder, leading to low levels of amniotic fluid. The doctor may suggest frequent ultrasound checks and other tests to assess the level of amniotic fluid and the growth of the fetus. Relevant medications or interventions may be suggested depending on the results of the tests.
- Frequent observation: If postnatal tests indicate mild hydronephrosis, the doctor may recommend observation through periodic ultrasound scans until the condition resolves on its own. The child may receive antibiotics to avoid infection. In case of moderate symptoms, if the kidney function is normal and the kidneys are growing well, doctors may still recommend observation.
- Surgery: In severe cases, surgery may be required. The surgery involves correcting the flow of the urine to reduce swelling and pressure in the kidneys. The type of surgery may vary depending on the cause of hydronephrosis. A common procedure is a pyeloplasty for ureteropelvic junction obstruction (UPJ), one of the most common causes of hydronephrosis in a newborn.
 Research finds
Research findsTaking Care Of Babies With Hydronephrosis, After Surgery
The baby may spend a couple of nights in the hospital after surgery. Post-surgery care includes the following (7).
- Diet: The baby may receive intravenous nutrition as a part of postnatal care for the initial days depending on the progress and whether the baby has other conditions, such as nausea.

Image: Shutterstock
- Pain management: The doctor may recommend pain medication. Some medications may cause constipation in children. In such cases, doctors may also prescribe stool softeners.
- Dressing: The site of the surgery may be tender for a couple of weeks. This may require proper and regular dressings.
- Catheter: It may be placed for some days to facilitate urination. The doctor may instruct parents about appropriate care after the baby is discharged.
- Restricted activity: The doctor would provide parents with dos and don’ts for the baby’s physical activity after being discharged. You may have to restrict the baby’s physical activity until they heal completely.
- Ultrasound: The baby may have to undergo periodic ultrasound scans to check for the progress and kidneys’ normal development.
Complications Of Hydronephrosis
Mild hydronephrosis usually resolves on its own without causing complications. Babies with moderate and severe hydronephrosis display a positive prognosis post-treatment. Untreated moderate and severe hydronephrosis may lead to long-term complications, including partial or complete renal failure (1). It could require a kidney transplant and may result in other related complications.
Frequently Asked Questions
1. What are the stages of hydronephrosis in babies?
The stages of hydronephrosis are decided based on the severity of the condition. Hydronephrosis in babies may be mild, moderate, or severe. Doctors may give it a grade of one to four, where one represents minimal dilation while four represents severe dilation (8).
2. Does hydronephrosis have other names?
Yes, hydronephrosis has other names (2). If the condition is present before birth, it may be called antenatal, prenatal, or fetal hydronephrosis. In other cases, it may also be called dilated or enlarged urinary tract
3. How long can hydronephrosis be left untreated?
If hydronephrosis is diagnosed in children after birth, it may be left untreated because, in most cases, it resolves on its own by the time they turn three (2).
However, if the condition in children is severe, immediate medical intervention is required to prevent further complications (1).
4. Is hydronephrosis related to Down syndrome?
Hydronephrosis in babies should not usually be a cause for concern as it does not lead to any side effects. However, if your baby shows signs of discomfort or is in pain, it is advised to consult the doctor. Ensure you are on the lookout for concerning symptoms and report them to the doctor immediately to avoid complications. If your baby needs surgery as part of the treatment, make sure you provide adequate post-surgical care by feeding them a nutritious meal, limiting their physical activity, and administering medications on time.
Infographic: How To Detect And Diagnose Hydronephrosis In Babies?
Hydronephrosis is a congenital kidney problem in babies that can be transient and resolve on its own or due to an underlying problem. Therefore, knowing about the symptoms can help in early diagnosis and treatment. Check out the infographic below to learn about the signs and various diagnostic methods to detect this condition in babies.
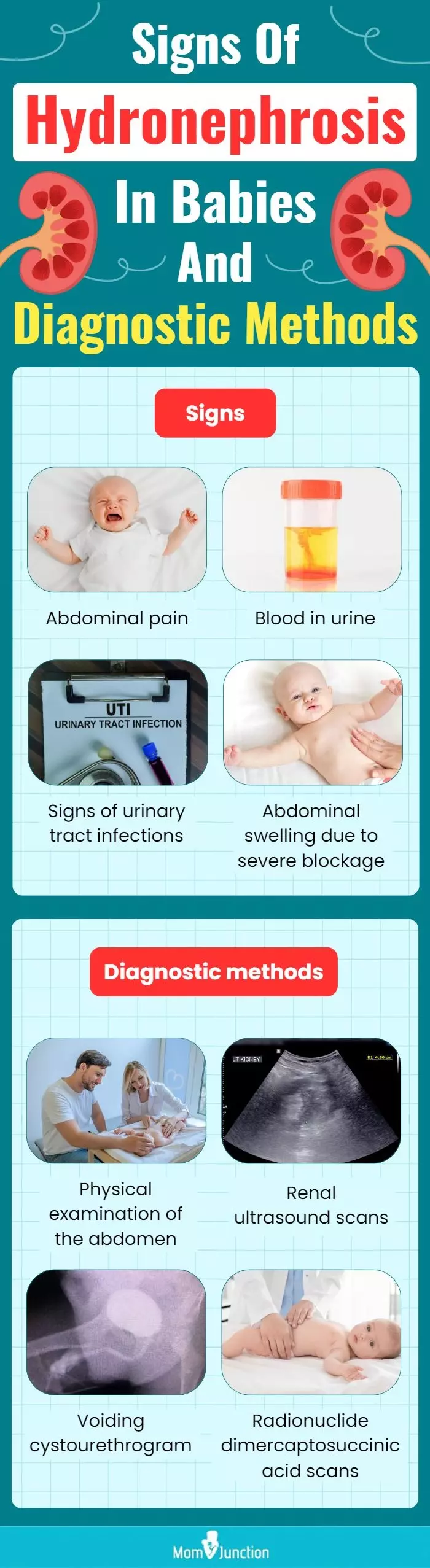
Illustration: Momjunction Design Team
Watch this interesting and informative video to better understand Hydronephrosis and how it is treated. Ensure you get a medical consultation before taking any steps.
References
- Hydronephrosis: CHOC Children’s
https://choc.org/programs-services/urology/hydronephrosis/ - Hydronephrosis in newborns: National Institute of Diabetes and Digestive and Kidney Diseases
https://www.niddk.nih.gov/health-information/urologic-diseases/hydronephrosis-newborns - Hydronephrosis: Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/15417-hydronephrosis - Hydronephrosis (pediatric): Columbia Doctors
https://www.columbiadoctors.org/treatments-conditions/hydronephrosis-pediatric - Hydronephrosis: Boston’s Children Hospital
https://www.childrenshospital.org/conditions-and-treatments/conditions/h/hydronephrosis - Hydronephrosis| Diagnosis & Treatments: Boston’s Children Hospital
https://www.childrenshospital.org/conditions-and-treatments/conditions/h/hydronephrosis/diagnosis-and-treatments - Postoperative Care Instructions for Pyeloplasty Nephrectomy Reimplant and Ureterostomy: CHOC Children’s
https://choc.org/programs-services/urology/postoperative-care-instructions-pyeloplasty-nephrectomy-reimplant-ureterostomy/ - Hydronephrosis
https://www.med.unc.edu/urology/pediatrics/pediatric-conditions/hydronephrosis/ - Juan C. Kupferman et al.; (2009); Increased Prevalence of Renal and Urinary Tract Anomalies in Children With Down Syndrome
https://publications.aap.org/pediatrics/article-abstract/124/4/e615/71823/Increased-Prevalence-of-Renal-and-Urinary-Tract - Fetal hydronephrosis
https://radiopaedia.org/articles/fetal-hydronephrosis
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Richard Mario Lurshay
Read full bio of Dr Bisny T. Joseph
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny
















