Image: Shutterstock
Hypo means less, and tone refers to the resistance of muscles in our bodies. So, the condition of hypotonia in babies refers to a low muscle tone, causing a flexed posture. However, it should not be confused with muscle weakness.
Hypotonia often occurs due to disorders of nerves, which control muscle movements. The condition commonly affects newborns and infants, although it may occur at a later age, as well. It is usually treated depending on the underlying cause, and prognosis and outcomes may vary accordingly.
Hypotonia can greatly affect a baby’s physical development and overall health. Recognizing its symptoms is essential for parents to get timely medical guidance and support. This post discusses the signs, causes, diagnosis, and treatment of hypotonia in babies.
Key Pointers
- Hypotonia results in poor muscle tone mostly since birth but noticeable later.
- Floppy hands and difficulty swallowing or sucking are signs of hypotonia in babies.
- Hypotonia can be caused by cerebral palsy, encephalitis, or brain injury, among other reasons.
- Support therapy or physiotherapy can help treat this condition.
Signs And Symptoms Of Hypotonia In Babies

Image: Shutterstock
Hypotonia may not be noticeable in babies younger than six months, although they might have it since birth. Babies with severe hypotonia (floppy baby syndrome) can be like rag dolls without any muscle strength. Many of them have a frog-like posture.
Hypotonic or floppy babies may have delayed motor development, but their intelligence is not affected by this condition. However, the clinical features may vary depending on the underlying causes of hypotonia.
The signs and symptoms of hypotonia in babies may include the following(1).
- Floppy head due to no or less control on neck muscles even after three months of age
- Sucking and swallowing problems
- Arms or legs may slip through your hands while holding
- Unable to keep any weight on shoulder or neck muscles
- Weak cry
- Arms and legs stay straight with no bending at joints, such as elbows, knees, or hips
Infants usually achieve head control after three months of life, but they have some muscle strength from birth. Motor developmental milestones such as crawling, sitting up, talking, eating, and walking, are often delayed in babies with hypotonia due to poor muscle control.
 Point to consider
Point to considerCauses Of Hypotonia
The most common cause of hypotonia is abnormalities in neurological control of muscle tone. Muscles need electrical signals from motor nerves for functioning. Any disruption in the signal generation or conduction may affect the muscle tone. Various inherited conditions and other factors can cause hypotonia.
Neurological disorders affecting the brain and spinal cord (central nervous system) may cause central hypotonia (2).
- Cerebral palsy is a neurological condition causing problems with coordination and movement.

Image: Shutterstock
- Meningitis is the infection of the outer membrane of the brain.
- Injury of the brain and spinal cord.
- Intracranial bleeding, which is bleeding inside the cranium.
- Encephalitis is an infection of the brain.
- Spinal muscular atrophy (SMA) is a genetic disorder affecting the muscle tone.
Neurological conditions affecting the peripheral nervous system (outside brain and spinal cord) may result in peripheral hypotonia(2)
.
- Congenital myasthenia gravis is a condition that causes increased muscle fatigue and weakness.
- Muscular dystrophy may include a group of genetic conditions causing muscle weakness and disability.
- Charcot-Marie-Tooth disease is a degenerative disease damaging the myelin that covers the nervous tissue. This may result in muscle weakness and other neurological issues.
- Spinal muscular atrophy causes muscle weakness and gradual loss of movement.
Non-neurological conditions may also lead to hypotonia in some cases (2).
- Premature birth, since muscle tone is not fully developed at the time of birth.

Image: Shutterstock
- Down’s syndrome is a chromosomal anomaly causing physical and mental developmental delays.
- Tay-Sachs disease is caused by mutation of genes on chromosomes producing specific proteins resulting in nervous system damage.
- Prader-Willi syndrome caused by loss of function of some genes may also result in muscle weakness.
- Connective tissue disorders, such as Marfan syndromeiA connective tissue disorder resulting in a blood vessel, heart, bone, eye, and joint problem. and Ehlers-Danlos syndromeiA hereditary disorder that primarily affects the connective tissues of skin, joints, and blood vessels. , may also result in muscle weakness.
- Autism and autismiA neurodevelopmental condition that impacts a person’s ways of learning and communication and behavior. spectrum disorders may be associated with hypotonia in some babies.
Endocrine disorders, such as hypothyroidism in babies, and nutritional deficiency can also cause hypotonia. It indicates that hypotonia can be a symptom of many diseases in babies. If there are no underlying causes, hypotonia usually improves when the baby grows older. However, some babies may have benign congenital hypotonia (BCH) present at birth without any underlying causes. BCH is non progressive hypotonia, which means it does not worsen with time.
Tanya, a mother to three beautiful children, talks about the birth of her eldest, Ava. She says, “I also noticed that Ava’s arms hung loosely down at her sides. She didn’t seem to have the strength to keep her limbs tucked in at her sides on her own. It didn’t dawn on me that this was an issue.
“In hushed tones, the pediatrician stated that she felt Ava might have Down syndrome. She explained to us that Ava had low muscle tone throughout her body, called hypotonia. This is why Ava’s arms hung loosely from her body. Ava’s jaw and tongue showed signs of low tone as well. Ava’s cute, peeping tongue was labeled a ‘tongue thrust’ and was not normal for children born without Down syndrome (i).”
 Quick fact
Quick factDiagnosis Of Hypotonia
Pediatricians may refer your baby to a specialist (pediatric neurologist) if they suspect hypotonia after primary evaluation. Family history, medical history, pregnancy, and delivery-related issues are asked to identify the cause. Healthcare providers may also use screening tools to evaluate the baby’s motor skills and overall development.
The following tests might be ordered to identify the cause of hypotonia in babies (3).
- Blood tests and genetic testing help to determine various congenital disorders and other conditions.

Image: Shutterstock
- CT scan helps visualize the nervous system damage.
- MRI scan helps to visualize any abnormalities.
- EEG or electroencephalogram records the electrical activity in the brain using electrodes. This may help to identify certain issues, such as seizures.
- Nerve conduction studies (NCV) use electrodes over the skin to measure electrical signals transmitted from the brain or spinal cord to the muscles.
- EMG or electromyography measures the electrical activity of the muscles.
- Muscle biopsy helps to identify the structural abnormalities of the muscle tissue, like muscle atrophy or muscle wasting.
Treatment For Hypotonia In Babies
The choice of treatments may vary depending on the underlying cause. Hypotonia may not be curable if the underlying conditions are not curable. However, hypotonia due to certain causes, such as prematurity and infections, may cure once the baby grows out of these conditions.
Developmental pediatrician or pediatric neurologist may design a skill training program for your baby according to the requirements and age. The program may include the following therapies and procedures (4).
- Physical therapy/physiotherapy may help to strengthen the muscles and improve coordination and posture.

Image: Shutterstock
- Occupational therapy aims to teach day-to-day skills, such as feeding, or any other skills apt for the age. They also identify and provide training for feeding and swallowing They could also make recommendations for feeding support.
- Speech and language therapy help the baby to learn speech and language skills relevant to their age.
- Support equipment, such as a foot or ankle support, and mobility solutions, such as a wheelchair, are recommended depending on the baby’s age and severity of hypotonia.
The outlook for infants with hypotonia can vary greatly based on the underlying cause. Some infants may show improvement with therapy, while others may experience ongoing challenges (5). Regular check-ups with healthcare providers are essential to track progress and adjust treatment plans as needed.
Frequently Asked Questions
1. How common is hypotonia in infants?
The exact incidence and prevalence of hypotonia are unknown as it may be a symptom of many other underlying conditions. Among congenital hypotonias, 60% of babies have central hypotonia. The rest of the cases are either from peripheral or unknown causes (6).
2. Is hypotonia a disability?
Hypotonia is a condition that can be counted as a disability since it affects a person’s independence to perform day-to-day activities (7).
3. Can hypotonia affect speech?
Hypotonia can affect the oral and facial muscles used to generate sounds. Therefore, children with hypotonia may experience speech problems (1).
4. Can hypotonia get better by massage?
Studies show that massages have a positive effect on hypotonia (8). Consult your pediatrician to know how to massage your baby correctly for maximum benefit.
Hypotonia in babies occurs when there is a disorder in the nerves controlling the muscle movements. As a result, you may notice floppy heads, sucking problems, and weak cries in these babies. Hypotonia may be caused by inherited conditions or other problems, such as injury, meningitis, muscular dystrophy, and premature birth. The condition in babies may remain the same, improve, or worsen over time. Hypotonia due to genetic and inherited conditions stay throughout life. Usually, the treatment depends on the cause of the hypotonia. If the cause is incurable, the condition persists. However, several therapies and management techniques help in improving the quality of life in children.
Infographic: What Causes Hypotonia In Infants?
Hypotonia leads to floppy babies with delayed cognitive and motor development. Check out the infographic below to learn about several neurological and non-neurological causes of hypotonia in children. Since the treatment depends on the underlying cause, knowing the reasons will help determine a treatment plan. Illustration: Momjunction Design Team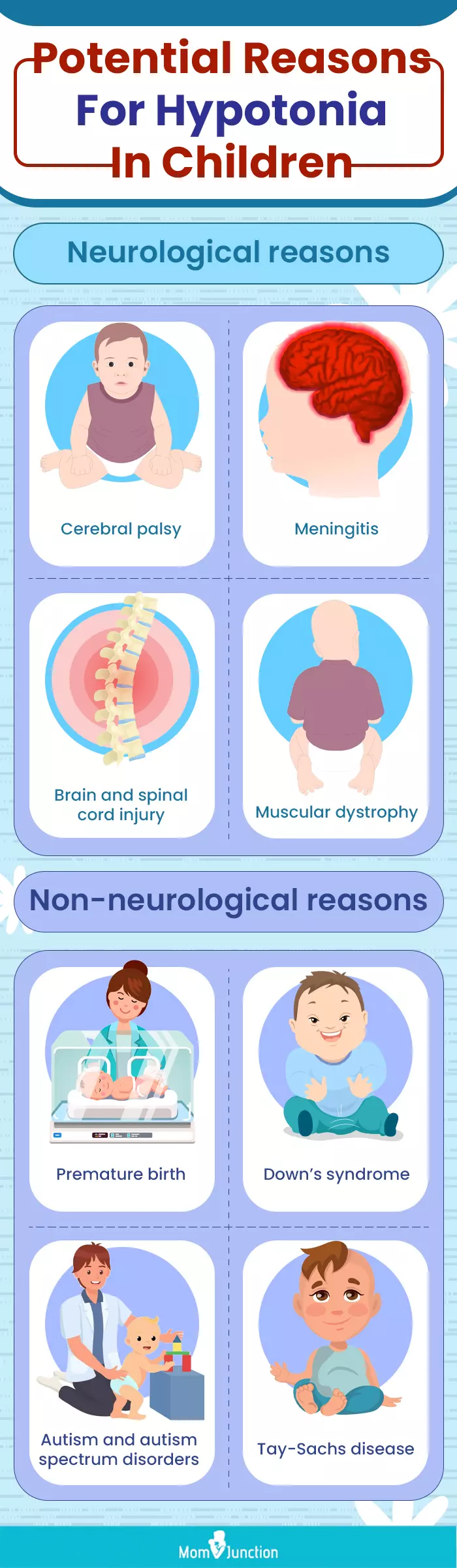
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Down syndrome and Ava — turning Hypotonia into wings;https://avasangelwings.wordpress.com/2018/12/27/hypotonia-and-ava-turning-low-tone-into-wings/
References
1. Muscle Weakness (Hypotonia); Boston Children’s Hospital
2. Causes; Hypotonia; National Health Service
3. Diagnosis; Hypotonia; National Health Service
4. Treatment; Hypotonia; National Health Service
5. Hypotonia; Child Neurology Foundation
6. Hypotonia; National Library Of Medicine
7. Hypotonia in Babies; Cleveland Clinic
8. Tiffany Field; Pediatric Massage Therapy Research: A Narrative Review; National Library of Medicine (2019)
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Anuradha Bansal
Read full bio of Dr Bisny T. Joseph
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny