Image: ShutterStock
If you have developed diabetes during pregnancy, a healthy and nutritious diet and routine workout usually help normalize blood glucose levels and maintain maternal and fetal health. However, sometimes, your doctor may prescribe insulin during pregnancy to maintain your blood glucose levels within the normal range (1). But how does one get gestational diabetes (GD) during pregnancy?
When pregnant, the placenta in a woman’s womb secretes hormones essential for the baby’s development. However, these hormones can impair insulin activity and induce GD in certain pregnant women.
Read this post to know the safety profile of oral hypoglycemic medications and injections in pregnancy.
Key Pointers
- The placenta produces hormones that can impair insulin activity during pregnancy.
- Insulin is administered through an insulin pen or pump to treat glucose intolerance.
- Pregnant women should consult with their doctor regarding the type of insulin, injection site, and administration technique.
- Taking insulin may result in side effects like weight gain, dizziness, blurred vision, weakness, sweating, and muscle cramps.
When Do You Need To Take Insulin During Pregnancy?
Women with diabetes do not produce insulin or their body stops responding to the natural insulin, increasing the blood glucose levels. Their endocrine system is affected as it impacts insulin production or function, resulting in high blood sugar levels. Therefore, insulin is required and may be prescribed to facilitate maternal glucose control (2).
Both fasting glucose and postprandial blood glucose levels during conception and pregnancy are important to be normal both for healthy fetal development and to maintain normal fetal growth. Glucose intolerance (the body cannot metabolize blood glucose) during or before pregnancy could lead to certain complications. Insulin treatment helps maintain these levels if diet and exercise do not control them sufficiently.
The presented graph depicts the variations in serum insulin levels throughout pregnancy. It reveals that in non-diabetic women, the typical insulin secretion increases from the 10th week of gestation, reaching its maximum around the 40th week, and then significantly decreases.
However, in gestational diabetes, the serum insulin levels decline from about the 20th week, taking a deep plunge at the 40th week. Consequently, this reduction in insulin levels leads to a surge in hepatic glucose production, resulting in elevated fasting blood glucose levels in the second and third trimesters.

Serum insulin variation throughout pregnancy
Source: Pregestational Diabetes in Pregnancy; Obstetrics and gynecology clinics of North AmericaIs Insulin Safe To Treat Gestational Diabetes During Pregnancy?

In prenatal care, insulin is the first line of treatment for type 1 and type 2 diabetes and uncontrolled GD during pregnancy. There are different types of insulin used during pregnancy, including rapid-acting, short-acting, intermediate-acting, and long-acting. The right dose depends on your blood sugar levels, diabetes type, and pregnancy stage (3). Your doctor will prescribe insulin only if necessary.
According to the American Diabetes Association (ADA), insulin administered through injection, insulin pen, or through an insulin pump is safe for pregnant women (4).
Does Insulin Affect The Baby During Pregnancy?
ADA says that insulin does not cross the placenta, and so it does not affect the baby.
Can Insulin Cause Miscarriage?
No, insulin is not known to cause miscarriage (5).
What Is The Suggested Drug Therapy For Treating Gestational Diabetes?
The guidelines of the American College of Obstetricians and Gynecologists (ACOG) recommend insulin as the first-line treatment for gestational diabetes that cannot be controlled by pregnancy nutrition and lifestyle changes.
The US National Institute for Health and Care Excellence (NICE) guidelines advise an initial treatment of insulin resistance either with or without metformin for women with complications of gestational diabetes (6). Insulin is available in only injection and pump form.
Your doctor may prescribe oral medications, such as metformin in pregnancy, for treating gestational diabetes and mild hyperglycemia. However, this is not standard practice. (6).
 Things to know
Things to knowWhich Insulin Is Safe During Pregnancy?

Your doctor is the best person to determine the type of insulin for you.
According to an article published in the American College of Clinical Pharmacy, intermediate-acting neutral protamine Hagedorn (NPH) insulin, the long-acting NPH, long-lasting insulin glargine, and regular insulin, or short-acting insulin may be considered by the doctors for treating GD (6). Additionally, regular blood sugar monitoring is essential for managing diabetes and keeping levels within the target range set by your healthcare provider.
Can You Inject Insulin On The Stomach When Pregnant?
Insulin should be injected into any fatty tissue. According to a publication in the Indian Journal of Endocrinology and Metabolism, the abdomen is a safe site for insulin injection during pregnancy.
The article recommends the below techniques to follow during the various stages of pregnancy.
- First trimester: You can inject insulin into your abdomen. If you’ve been injecting it into the abdomen before conception, there is no need to change the injection site or technique.

- Second trimester: Lateral parts of the abdomen are suitable for injection, but avoid the skin overlying the fetus (7).
- Third trimester: The Forum of Injection Techniques, India, suggests that insulin be injected into the abdomen but by ensuring that the skin fold is properly raised. If you are apprehensive about getting an injection on your abdomen, talk to your doctor about changing the injection site to the thigh, upper arm, or buttock (8).

Talk to your healthcare provider for initial guidance on injecting insulin. With time, you will become comfortable in safely administering insulin by yourself.
 Quick tip
Quick tipAre There Any Side Effects Of Using Insulin During Pregnancy?

Insulin is crucial to protect the mother and the growing baby from the effects of gestational diabetes. However, the injection itself might have a few side effects, such as (9):
- Redness, swelling, and itching near the injection site
- Skin thickening or a little depression in the skin
- Weight gain
- Constipation
- Shortness of breath
- Wheezing
- Dizziness
- Blurred vision
- Sweating
- Fast heartbeat
- Weakness
- Muscle cramps
- Swelling of the arms, legs, feet, ankles and lower legs
 Quick fact
Quick factIf you experience any of the following symptoms, call your doctor.
Frequently Asked Questions
1. How many units of insulin is safe during pregnancy?
Units for insulin dosage taken during pregnancy can depend on factors such as body weight, blood sugar levels, and how far you are in pregnancy. The desirable insulin levels can be different for each woman and are prescribed by the doctor after a thorough evaluation (12).
2. Can I stop insulin after delivery?
For most women, healthcare providers will advise stopping insulin immediately after childbirth. However, you may have to carry on with glucose monitoring regularly (13).
3. What are some of the risks associated with insulin resistance or gestational diabetes during pregnancy?
Insulin resistance and gestational diabetes during pregnancy can increase the risk of complications such as neonatal hypoglycemia, a large baby, high blood pressure, cesarean delivery, and increased susceptibility to developing type 2 diabetes later in life (14).
4. Can insulin therapy during pregnancy have any long-term effects on the mother or baby?
Although insulin therapy is generally considered safe during pregnancy, a few studies state that it might impact placental size and function. However, there is limited research on its long-term effects on both the mother and baby. Therefore, large-scale studies are necessary to understand the potential impacts on pregnant women (15) (16).
Most women have been successful in gestational diabetes management with insulin during pregnancy. However, your doctor will suggest insulin only when your diabetes is uncontrolled with diet and exercise. You need to take the prescribed insulin dosage regularly to prevent ketoacidosis. The type and dosage of insulin will be based on the severity and stage of your pregnancy. Moreover, insulin is safe for pregnant women as no reports suggest its adverse effects on pregnancy or the fetus. However, it is crucial to be in close contact with your antenatal care provider to facilitate close monitoring and favorable pregnancy outcomes.
Infographic: Hypoglycemia During Pregnancy
An overdose of insulin or delaying meals while on insulin may cause blood glucose to fall below normal. Hypoglycemia during pregnancy may be problematic. This infographic helps you identify the symptoms of low blood sugar and suggests a few ways to deal with it.
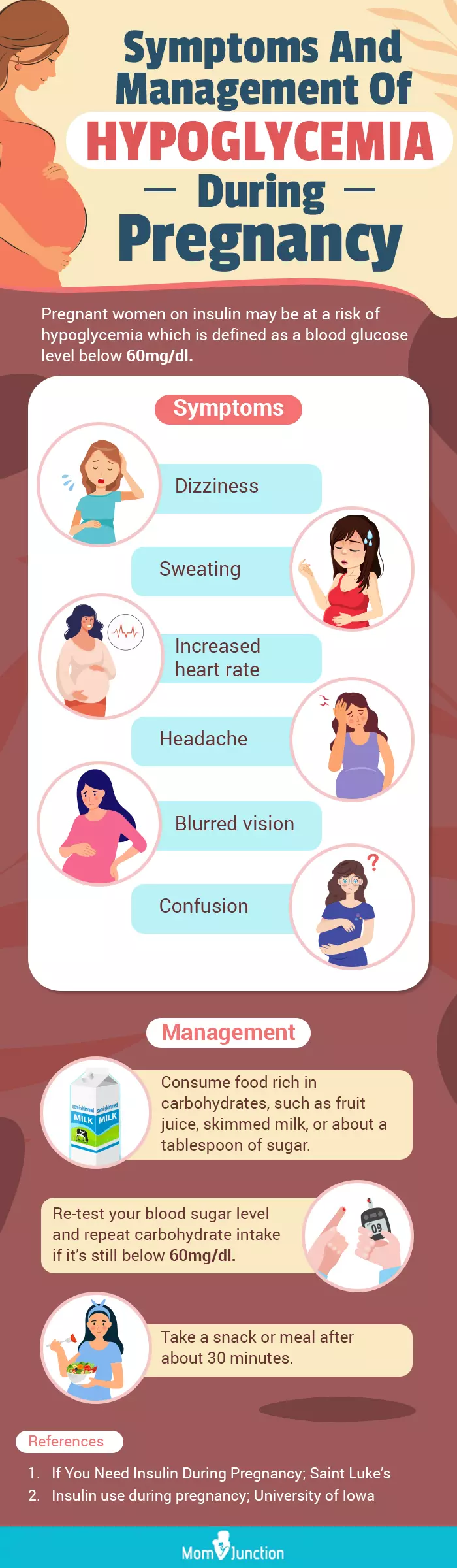
Illustration: Momjunction Design Team
Illustration: Insulin During Pregnancy: When You Need It And Safety Measures

Image: Dall·E/MomJunction Design Team
Navigating pregnancy becomes even more intricate when facing gestational diabetes. Discover the potential benefits of insulin as a supportive measure through insightful video content.
References
1. Gestational Diabetes Information- Commencing Insulin Therapy; Department of Health; Queensland Government
2. Laura Hieronymus, and Patti Geil; Expecting the best: Diabetes, Pregnancy, and Blood Glucose Control; National Federation of the Blind
3. Alyson K. Blum; Insulin Use in Pregnancy: An Update; NCBI (2016)
4. Prenatal Care; American Diabetes Association
5. Karen L. Whalen and James R. Taylor; Gestational Diabetes Mellitus; American Academy of Clinical Pharmacy
6. Pregnancy if You Have Diabetes; National Institute of Diabetes and Digestive and Kidney Disease
7. Sanjay Kalra, et al.; Addendum: First injection technique recommendations for patients with diabetes, Forum for Injection Techniques India; NCBI (2013)
8. Nikhil Tandon, et al.; Forum for injection technique and therapy expert recommendations, India: The Indian recommendations for best practice in insulin injection technique, 2017; Indian Journal of Endocrinology and Metabolism
9. Insulin Injection; MedlinePlus; US National Library of Medicine
10. Taking medication and insulin for gestational diabetes; Tommy’s
11. Insulin use during pregnancy; University of Iowa Hospitals and Clinics
12. Eman M. Alfadhli ; Gestational diabetes mellitus; NCBI (2015)
13. Your health after birth with type 1 or type 2 diabetes; Tommys
14. About Gestational Diabetes.; Centers for Disease Control and Prevention.
15. Subiabre Mario et al.; Insulin therapy and its consequences for the mother, foetus, and newborn in gestational diabetes mellitus; NCBI (2018).
16. Rabia Arshad et al., Effects of insulin on placental, fetal and maternal outcomes in gestational diabetes mellitus; NCBI (2014).
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Christian Pope
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das