Image: Shutterstock
Premature labor and preterm birth may have considerable negative health impacts on the baby and the mother. Tocolytics are a category of medications used to suppress uterine contractions and deter labor onset. The use of tocolytics such as Nifedipine in pregnancy is one of the ten recommendations of the World Health Organization (WHO) to prevent preterm birth and support the premature baby’s survival (1). Read this post to know about the safety of using Nifedipine during pregnancy, when and how to use it, and its potential side effects.
Key Pointers
- Nifedipine is a medication used to manage hypertension, vasospastic angina, and chronic stable angina, and to suppress preterm labor and delay delivery.
- The drug works by relaxing smooth muscles and inhibiting uterine wall contractions. It can prolong delivery by up to 48 hours, allowing for proper lung development in the fetus.
- Nifedipine should not be used if the mother has preterm pre-labor rupture of membranes, placental abruption, or cardiac disease.
- Possible side effects of taking the drug include headache, vomiting, palpitations, difficulty breathing, and anxiety.
What Is Nifedipine?

Image: Shutterstock
Nifedipine (sold under the brand names Procardia, Adalat,) is a calcium ion influx inhibitor and is used as an antihypertensive medication, which helps in managing hypertension, vasospastic angina (spasms in the coronary heart), and chronic stable anginaiChest pain that frequently happens with action or under emotional stress. (2). This drug is also used to suppress preterm labor and delay delivery (3).
Is It Safe To Use Nifedipine During Pregnancy?
It is both yes and no, read on to find out more.
The US Food and Drug Administration (FDA) categorized nifedipine as “pregnancy category C” drug, which means animal studies have shown some adverse effects, and there are no well-controlled studies in humans. It recommends the use of nifedipine only if the potential benefits outweigh its risks, such as to reduce maternal and fetal distress (2).
 Quick fact
Quick factAlso, the usage of this antihypertensive drug depends on why it is considered in the first place during pregnancy. Next, we take a look at such scenarios.
What Is Nifedipine Used For During Pregnancy?
There are two cases during pregnancy where your doctor could prescribe nifedipine. Do not take this medicine without consulting a doctor.
1. Hypertension

Image: IStock
The overall prevalence of hypertensive disorders of pregnancy during 2017-2019 was 14.6%, as per the CDC. A descriptive study of 21 pregnant women with acute episodes of severe maternal blood pressure during pregnancy showed a significant fall when given nifedipine. Even though there were side effects such as headache and cutaneous flushing, no adverse fetal defects were seen (4).
2. Tocolysis
The WHO guideline development group agreed that “in women at risk of imminent preterm birth, who have an otherwise uncomplicated pregnancy, the acute use of a tocolytic drug to prolong the pregnancy to up to 48 hours can be considered as a window for administration of antenatal corticosteroidsiDrugs that are given to expectant mothers to prevent premature birth. ” (1).
Nifedipine is considered the preferred tocolytic agent to others. Your doctor might prescribe this medication for prolonging the pregnancy for as long as it is safe to do if it helps in improving the neonatal outcome.
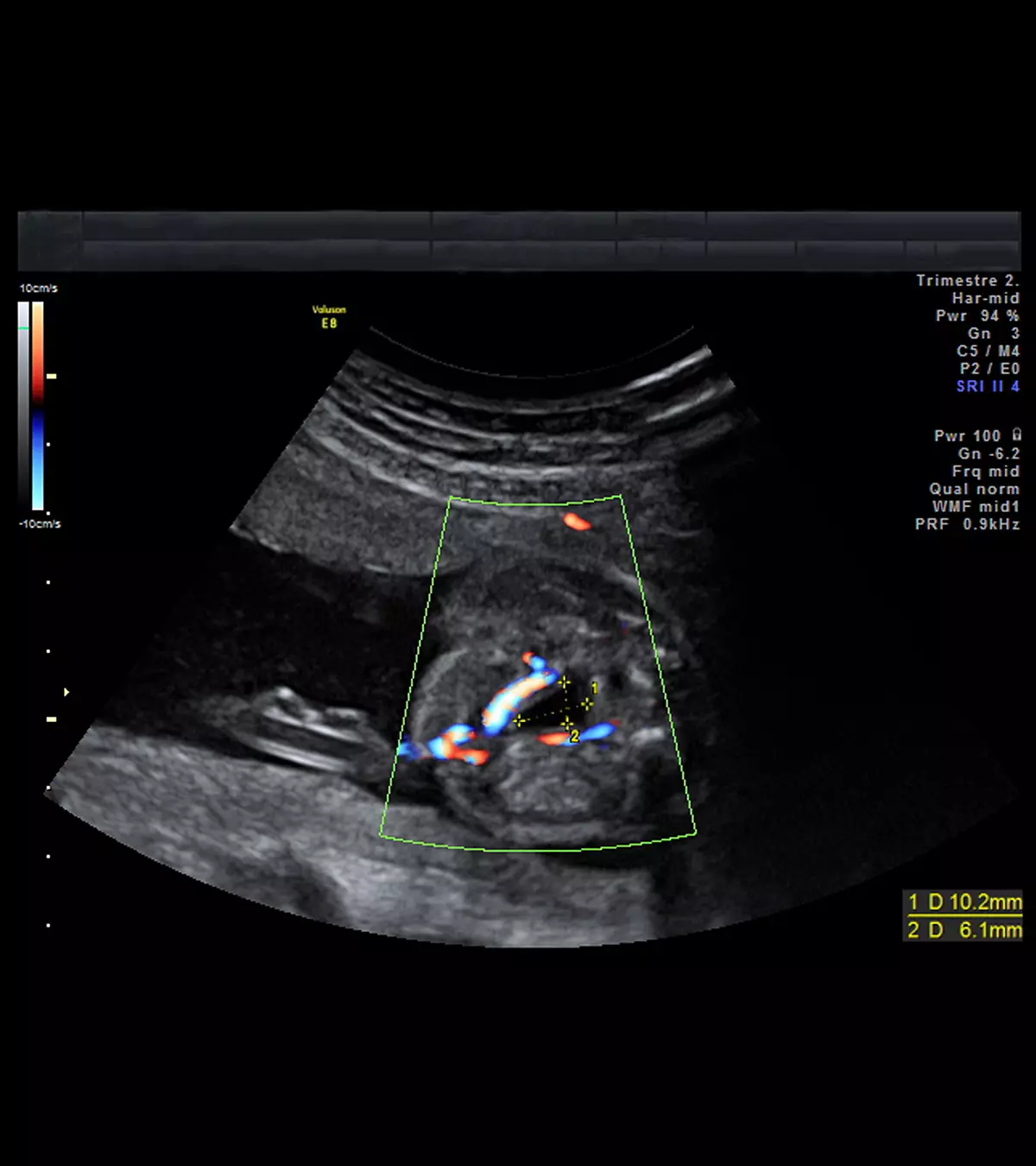
How Does Nifedipine Work During Pregnancy?
Nifedipine helps in the short-term prolongation of pregnancy by relaxing the smooth muscles and inhibiting the contraction of the uterine wall. The main advantage of this drug is to prolong the delivery by 48 hours such that it gives time for the corticosteroidsi to accelerate the lung formation of the baby. Nifedipine is given between 24 and 34 weeks of gestation with intact membranes in an otherwise uncomplicated pregnancy. It is usually administered under medical supervision with close monitoring, especially during the first doses, to check its effectiveness and side effects. Dosages are adjusted based on the mother’s response and fetal condition (5).
When Is Nifedipine Not Used As A Tocolytic Agent?
While nifedipine is considered safer than other tocolytic agents, doctors do not prescribe this drug in certain cases. The WHO contraindicates the usage of nifedipine for tocolysis if the mother has the following conditions (1).
- Preterm pre-labor rupture of membranesiA membrane breakage that occurs before the labour contractions and prior to 37 weeks of pregnancy.
- Chorioamnionitis (a bacterial infection before or during the labor)
- Placental abruptioniThe early detachment of placenta from the uterine lining before the second stage of labour ends.
- Cardiac disease
What Is The Recommended Dosage Of Nifedipine During Pregnancy?
Once there is confirmation of preterm labor, a stat dose of 20mg is usually given. If the contractions do not settle, your doctor might give a second dose of 20mg 30 minutes after the first dose. No further medicine is given until three hours after the second dose (6).
 Research finds
Research findsIf the contractions continue even after that, then another 20mg of nifedipine is given every three to six hours for 48 hours until the contractions stop.
The doctors usually do not give more than 160mg within 24 hours.
What Are The Side Effects Of Nifedipine During Pregnancy?

Image: IStock
A study on 70 consecutive women with clinical features of preterm labor concluded that nifedipine was more successful in prolongation of the pregnancy with fewer side effects and better tolerability (7).
Although calcium channel blockers such as nifedipine are generally well tolerated, they are associated with a few side effects such as (8).
- Headache associated with transient hypotensioniTemporary or short-term drop in blood pressure.
- Maternal tachycardiaiIncreased heart rate during pregnancy.
- Anxiety
- Vomiting
- Palpitations and flushing
- Maternal pulmonary edema (when given orally)iThe buildup of fluid in the lungs during pregnancy.
- Difficulty in breathing
Does Nifedipine Affect The Fetus?

Image: Shutterstock
Studies show that nifedipine does not affect fetal movements, heart rate, or blood flow, so the probability of adverse defects, such as fetal heart rate abnormalities, is low when used as a tocolytic agent (8).
A retrospective analytical study of 4,478 uncomplicated pregnancies, which were treated with nifedipine for preterm delivery, resulted in an overall success rate of 84.92% with no major maternal and fetal side effects (9).
How Long Does Nifedipine Work For Preterm Labor?
A tocolytic agent such as nifedipine can delay the labor for over 48 hours (1). In a randomized study with 206 threatened preterm labor patients, after 90 minutes of administration of nifedipine, 88.3% women of the nifedipine group had no uterine contractions (10).
There is a chance that drugs like nifedipine can help in better neonatal outcomes in risky pregnancies. The doctors prescribe such medications only when the need outweighs the risks.
Precaution: Consumption of grapefruit as a whole or its juice must be avoided while taking nifedipine, because the chemicals in the fruit bind with the medicine and reduce its absorption through the gut. Thus, high concentrations of the medicine can enter directly into your bloodstream, causing an overdose (11).

Image: IStock
Frequently Asked Questions
1. Which is better, labetalol or nifedipine in pregnancy?
According to a study, nifedipine was better at controlling blood pressure than labetalol. Also, it was found that nifedipine reduced preterm labor, possibly due to its tocolytic activity, and it performed better in cases of hypertensive urgency (15).
2. Can labetalol and nifedipine be taken together during pregnancy?
Nifedipine and labetalol are safe and effective drugs that can help treat hypertensive disorders in pregnancy, including gestational hypertension and preeclampsia, that could lead to placental insufficiency and fetal growth restriction. However, you should only take these medications during pregnancy under strict medical supervision and guidance (15).
3. Are there any contraindications or precautions for using Nifedipine during pregnancy?
The use of Nifedipine is subjective to the individual patient. It should not be used if the person possesses hypersensitivity to nifedipine and its components or has an ST-elevation myocardial infarction. Nifedipine may also be contraindicated for women with unstable angina, severe aortic stenosis, heart failure, hypotension, and moderate or severe hepatic impairment (16).
4. What should a pregnant woman do if she experiences any adverse effects while taking Nifedipine?
Nifedipine is usually considered one of the safest calcium blockers that can be administered to pregnant women. If the mother experiences any side effects, such as headaches, edema, dizziness, vomiting, and difficulty breathing, then they should notify and consult their healthcare provider immediately. In rare and extreme cases, they may face hypersensitivity reactions, such as pruritus, bronchospasms, and urticaria, which also require immediate medical attention (16).
Due to its categorization as a “pregnancy category C” drug, Nifedipine in pregnancy can be taken if its benefits outweigh its risks. Your doctor may prescribe this drug as a tocolytic agent to avoid obstetric complications, such as preterm labor, and maintain the premature baby’s survival. It may also be used for blood pressure control in the case of severe hypertension in expectant mothers, which can sometimes lead to intrauterine growth restriction. While Nifedipine’s risk of serious fetal abnormalities is low, it can produce side effects such as maternal tachycardia, anxiety, and pulmonary edema. So, only take Nifedipine if your doctor has recommended it, and avoid eating grapefruit while taking it.
Infographic: Possible Adverse Effects Of Nifedipine During Pregnancy
Nifedipine is an effective drug for preterm labor, whose adversities on the pregnant mother and fetus are poorly understood. So, if you are advised to take this medication during pregnancy, learning about its possible side effects can help. We highlight some common adverse effects of nifedipine in this infographic. Illustration: Momjunction Design Team
Illustration: Nifedipine In Pregnancy: Safety Usage Dosage And Side Effects

Image: Dall·E/MomJunction Design Team
Are you wondering about the safety of blood pressure medications for you and your baby? The following video may provide you with more information on this question.
References
1. WHO Recommendations on interventions to improve preterm birth outcomes; World Health Organization
2. Procardia XL; The US Food and Drug Administration
3. Patricia Smith, John Anthony, Richard Johanson; Nifedipine in pregnancy; British Journal of Obstetrics and Gynaecology
4. Walters and Redman; Treatment of severe pregnancy‐associated hypertension with the calcium antagonist nifedipine; BJOG
5. Protocol: Tocolysis with Nifedipine; Cree Health
6. Nifrdipine for preterm labour; South Australian Perinatal Practice Guideline; Department for Health and Agening, Government of South Australia
7. Maitra Nandita, Christian Vincent, Verma RN, Desai VA; Maternal and fetal cardiovascular side effects of nifedipine and ritodrine used as tocolytics; The Journal of Obstetrics and Gynecology of India
8. Robert Gaspar; and Judit Hajagos; Calcium Channel Blockers as Tocolytics: Principles of Their Actions, Adverse Effects and Therapeutic Combinations; NCBI (2013)
9. Parag Hangekar, Anand Karale, and Neelesh Risbud; Our experience of nifedipine as a tocolytic agent in preterm labor (24 weeks to 36 weeks 6 days); International Journal of Reproduction, Contraception, Obstetrics and Gynecology
10. Srisuda Songthamwat, Chatchanawadee Na Nan, and Metha Songthamwat; Effectiveness of nifedipine in threatened preterm labor: a randomized trial; NCBI(2018)
11. Grapefruit and medication: A cautionary note; Harvard Health Publishing
12. C H Childress and V L Katz; Nifedipine and its indications in obstetrics and gynecology; NCBI(1994).
13. D N Papatsonis et al; Calcium channel blockers in the management of preterm labor and hypertension in pregnancy; NCBI(2001).
14. Bibi Shahnaz Aali and Samira Shahabi Nejad; Nifedipine or hydralazine as a first-line agent to control hypertension in severe preeclampsia; NCBI (2002).
15. Dr. Nilesh Dalal, Dr. Somen Bhattacharjee and Dr. Mansi Tiwari ; A comparative study of oral labetalol versus oral nifedipine in hypertensive disorders of pregnancy; International Journal of Clinical Obstetrics and Gynaecology (2019).
16. Kashif M. Khan et al.; (2022);Nifedipine; NCBI.
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Jenni Johnson
Read full bio of Sakshi Mishra
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das