Image: Shutterstock
Jaundice in pregnancy can be due to liver disorders or certain conditions directly or indirectly related to pregnancy. Liver disorders are rare, but when they do occur, they can affect both mother and her unborn baby. Nearly 3% of all pregnancies can be complicated with liver conditions (1).
Jaundice is the yellowing of the skin and the whites of the eyes. This is caused by a buildup of bilirubin, a yellow-orange bile pigment in the blood. Usually, the liver changes the chemical composition of the bilirubin that allows it to be excreted from the body. Pregnant women can have jaundice due to gallstones, cholestasis (slow bile flow), or changes in liver function due to hypertensive disorders.
Read on to know the causes, symptoms, complications, and treatments for jaundice in pregnancy and its impact on maternal and fetal health.
Key Pointers
- Bilirubin buildup in the blood causes jaundice.
- Gallstones, cholestasis, or liver function changes from hypertensive disorders can lead to jaundice in pregnant women.
- Jaundice may exhibit symptoms such as fever, chills, yellowing of skin and eyes, and itchy skin.
- Preeclampsia, Hyperemesis gravidarum, and Dubin-Johnson syndrome are specific pregnancy conditions that can cause jaundice.
- Treatment for pregnancy-related jaundice is dependent on the root cause and can include medication, dietary modifications, or delivery of the baby.
How Common Is Jaundice In Pregnancy?
Jaundice in pregnancy is relatively rare, occurring in one out of 1,500 pregnancies, which is an incidence rate of 0.067% (2).
It has been reported that abnormal liver tests do appear in 3%—5% of pregnancies (3). But these are not always jaundice, and most abnormalities in the liver are often associated with the state of pregnancy itself.
What Are The Symptoms Of High Billirubin During Pregnancy?
Signs and symptoms of jaundice may vary depending on the underlying condition (maternal infection or liver disease). Some of the general symptoms of jaundice in pregnancy are (4):
- Fever
- Chills
- Abdominal pain
- Yellowing of skin and white portion in the eyes, what we are calling jaundice.
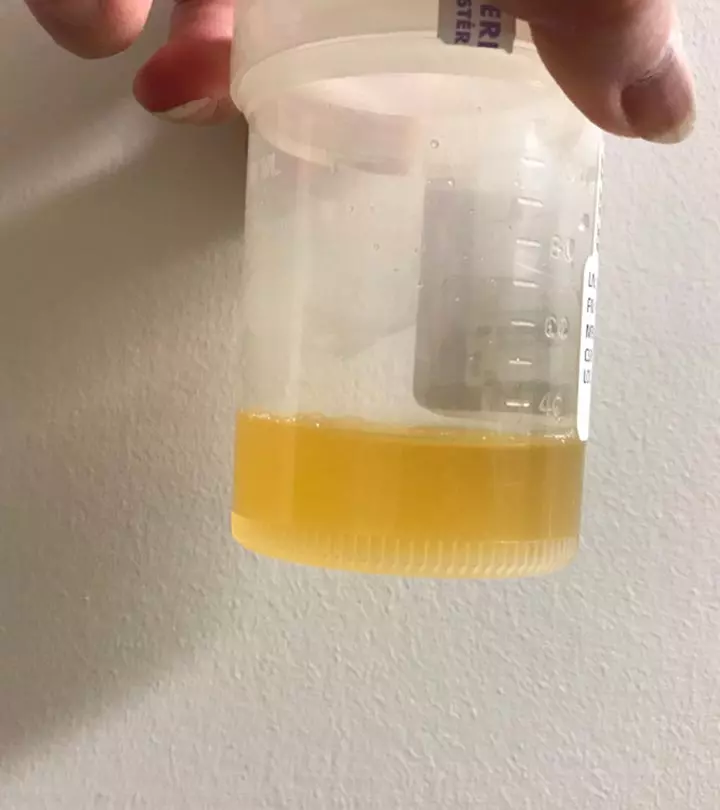
- Dark-colored urine
- Light or clay-colored stools
- Weight loss
- Itchy skin (pruritus)

What Are The Causes Of Jaundice In Pregnancy?
The fundamental cause of jaundice is the presence of excess bilirubin (hyperbilirubinemia), a yellow-orange pigment in the body. Bilirubin is a natural compound produced in the body and processed by the liver. The presence of high levels of bilirubin in the body suggests something wrong with the liver.
According to experts, jaundice in pregnancy can occur in any of the three trimesters. It may result from the conditions that are either associated with the pregnancy or unrelated to it (1).
Pregnancy-specific conditions that can cause jaundice are:
- Preeclampsia (second or third trimester): This condition affects 5—10% of all pregnancies. Affected women have high blood pressure, edema, and proteinuria ( high amount of protein in the urine) (3).
- HELLP syndrome (second or third trimester): The hemolysis (H), elevated liver tests (EL), and low platelet count (LP) (HELLP) syndrome occurs in one out of 1,000 pregnancies. A severe form of preeclampsia, it is characterized by vomiting, nausea, edema, weight gain, abdominal pain, proteinuria, hypertension, fatigue, and jaundice (3).
- Hyperemesis gravidarum (first trimester): This condition affects about 0.3% of pregnant women. It is characterized by severe nausea and vomiting that may lead to weight loss, electrolyte imbalance, disturbed nutrition, and jaundice (3) (5).
- Intrahepatic cholestasis during pregnancy (second or third trimester): This condition is rare but can increase the risk of fetal mortality. It is characterized by impaired bile flow and elevated bile acids in the bloodstream and causes severe itching (pruritus) in expecting mothers. Often, women also develop symptoms of jaundice, such as yellowing of skin and eyes (1) (6). Around 20% of the patients develop jaundice and pruritus due to intrahepatic cholestasis of pregnancy. It can cause complications like fetal distress, which may lead to preterm birth. It can also lead to the baby passing meconium (first stool) into the amniotic fluid, potentially causing severe respiratory issues at birth. In cases where bile levels in the blood are very high, there is also a risk of stillbirth (6).
Sai De Silva, a 38-week pregnant woman and vlogger, shares how her persistent itching was eventually diagnosed as cholestasis. She says, “I did not get the itching in my feet at all. However, I get itching in my hands. For me, the itching started in my breasts. I assumed it was hormonal, or my milk must be coming. Overall, I thought it was normal. However, gradually, it moved towards my chest, neck, face, and ears.
“Alarmed, I consulted my doctor three days later. She promptly suggested liver and bile acid tests. While my liver results were normal, the bile acid tests showed elevated levels, indicating a cause for concern (i).” Silva was diagnosed with cholestasis and put on medications to regulate the bile and schedule for induced labor.
- Dubin-Johnson syndrome (second or third trimester): It is a genetic disorder that is characterized by recurring jaundice. Usually, jaundice worsens during pregnancy due to this condition (7).
- Acute fatty liver of pregnancy (third trimester): Although rare, it is characterized by jaundice, nausea, vomiting, headache, anorexiaiAn eating disorder characterized by reduced food intake and extremely low body weight , ascitesiAbnormal fluid accumulation in the abdomen, which could be due to liver dysfunction , hypertension (high blood pressure), and edema (swelling). Abdominal pain during pregnancy is another symptom of acute fatty liver of pregnancy (3). The condition could be fatal.
Other conditions that can cause jaundice, but are unrelated or not associated with pregnancy are:
- Acute viral hepatitis: It is the most common cause of non-pregnancy jaundice. Acute hepatitis A occurs in one out of 1,000 pregnancies, and acute hepatitis B occurs in two out of 1,000 pregnancies. There is also a possibility of hepatitis C,but hepatitis D is rare (1) (3). Hepatitis E can be life-threatening.
- Gallstones in the common bile duct (Choledocholithiasis): This condition occurs when a gallstone blocks the common bile duct. Around 7% of women with jaundice in pregnancy have this condition (8).
- Drug-induced toxicity (hepatotoxicity): Excess dosage of a few drugs such as acetaminophen can induce toxicity in the liver, thus causing jaundice.
- Worsening of underlying chronic liver disease: Expecting mothers with chronic liver diseases such as chronic hepatitis, autoimmune disease, Wilson’s disease, and primary biliary cirrhosis may experience complications that may require regular screening (1).
What Are The Possible Risks And Complications?
Depending on the cause of jaundice in pregnancy, the complications may vary for both the mother and the baby (1) (3).
- Premature labor
- Abruptio placentae or placental abruption (premature separation of the placenta from the uterus)
- Placental insufficiency (placenta is unable to deliver necessary nutrients and oxygen to the developing fetus)
- Renal or hepatic failure
- Hepatic ruptureiA rare but severe complication of liver disease during pregnancy , also called hepatic hemorrhage
- Perinatal or fetal distress and death
- Postpartum hemorrhageiSevere bleeding after childbirth causing symptoms such as reduced blood pressure and weakness
- Variceal bleeding, which is the bleeding from ruptured blood vessels (a major risk factor for patients with cirrhosis)
- Hepatic encephalopathy (decline in brain function due to severe liver disease)
- Fulminant viral hepatitis (sudden and acute liver failure)
If you have chronic liver disease or have experienced any unusual symptoms, consult your healthcare practitioner for early diagnosis and better management of your underlying condition.
Diagnosis Of Jaundice In Pregnancy
Healthcare practitioners diagnose jaundice by identifying signs and symptoms for liver diseases. They may check for the presence of the following (4).
- Yellow discoloration of the skin and the sclera (white of the eye)

- Appearance of red coloration and bruises on the skin of palms and fingers
- Presence of abnormal collection of blood vessels near the skin surface (also known as spider angiomas)
- Bilirubin levels in the blood and urine
- Hepatitis viral test to determine the presence of hepatitis in pregnancy
- Liver enzyme tests to determine the levels of liver enzymes such as aspartate aminotransferase (AST) and alanine aminotransferase (ALT) through a blood test
- Ultrasound imaging to check the size of the liver
In rare cases, the doctor might suggest a liver biopsy. The above tests are usually sufficient to determine the cause of jaundice in pregnancy.
Treatment Of Jaundice In Pregnancy
Jaundice in adults does not require any treatment, and the condition cures by itself. The doctor may recommend management techniques and, in a few cases, medication when the risk of jaundice is severe enough to affect the mother or the fetus. Here are some measures taken to manage jaundice during pregnancy (3).
- Bed rest and intravenous fluids.

- Providing the mother with supplements that help in ensuring that the growing fetus gets sufficient nutrition.
- Balanced nutritious diet that can help the immune system fight viruses better.
- Stabilizing the blood pressure through hospitalization and medication.
- Laparoscopic surgeryiA surgical intervention used to evaluate and treat medical conditions in the abdominal and pelvic regions might be required in the cases of jaundice caused by blocked bile ducts.
Timely treatment of jaundice in severe cases is vital to prevent kernicterus, a rare but serious condition that occurs when there is too much bilirubin in a newborn’s blood, leading to brain damage and other complications. Careful monitoring of liver function and bilirubin levels is important for managing jaundice during pregnancy. Doctors may suggest regular check-ups to track the health of both the mother and baby and adjust the treatment plans.
Foods To Eat And Foods To Avoid
During jaundice, you might have to avoid foods that could strain the liver and slow down its repair. In addition to the dietary recommendations made by your doctor, you may follow some general guidelines for jaundice in pregnancy (9).
- You could add five portions of fruits and vegetables in your diet. These are excellent sources of fiber, minerals, and vitamins. Some fruits and vegetables might not be suitable for consumption during pregnancy. Therefore, consult a doctor to know more.

- Include whole grains like oatmeal and brown rice in your diet. You can also have lean protein from meat.
- Opt for food items that are low in saturated fat and prefer unsaturated fat. Check the food labels for the presence of these fats.
- Avoid packaged or canned food items that have added refined sugars, saturated fats, and high sodium levels.
- In the case of viral hepatitis infection (Hepatitis A), you may continue with a regular healthy diet. You might need nutritional supplements to help the body cope with the illness and to manage any sudden weight loss.
 Quick tip
Quick tipDo oranges cause jaundice during pregnancy?
No correlation or association has been found between the consumption of oranges and jaundice in pregnancy. They are an excellent source of vitamin C, which is required during pregnancy.
How To Prevent Jaundice During Pregnancy?
There is no single method to prevent jaundice in pregnancy. Below are some general precautions and preventive measures (4).
- Have a healthy diet and maintain a healthy weight to keep your liver and body systems healthy.
- Quit alcohol.
- Make regular visits to your healthcare practitioner during pregnancy. Regular checkups might help detect any problems early.

- Observe hygiene to prevent hepatitis infection. Wash hands before eating and always eat food cooked hygienically. Avoid sharing personal items, like plates, through the course of your pregnancy. Vaccination is available for some forms of hepatitis. Speak to your doctor about immunization against hepatitis.
- If you have not conceived yet and have chronic liver disease, then consult a healthcare practitioner before planning your pregnancy.
Jaundice in pregnancy is a rare occurrence. However, an expecting mother can develop jaundice due to liver disorders or pregnancy-specific conditions, such as preeclampsia. Regular prenatal checkups and fetal monitoring can help in early diagnosis and timely initiation of treatment. However, if the treatment is delayed, jaundice could lead to adverse complications like hepatic failure. Though preventing jaundice isn’t always possible, following simple antenatal care measures, such as eating a well-balanced diet and maintaining a healthy weight, can help. Also, ensuring you observe precautions can help prevent hepatitis infection.
Frequently Asked Questions
1. What are the long-term effects of jaundice during pregnancy?
The long-term effects of jaundice during pregnancy depend on the underlying cause and how soon the treatment is given. Overall, long-term effects have decreased in recent times due to early identification and treatment of pre-existing liver disorders and quick recognition of liver anomalies (12).
2. How do hormones affect jaundice in pregnancy?
In the second half of pregnancy, a surge in placental hormones can impact the liver’s function, causing bile movement to slow down and metabolism to decrease. This may cause jaundice when the liver cannot remove bilirubin from the blood, resulting in elevated maternal bilirubin levels (13).
3. How long does it take for jaundice to resolve after delivery, and are there any long-term effects on the mother or baby?
Cholestatic jaundice of pregnancy is typically a temporary condition that occurs during the final trimester and resolves within 1-2 weeks following delivery (14).
4. Is jaundice in pregnancy a serious condition?
Jaundice during pregnancy is usually mild and can be effectively managed. However, in specific circumstances such as pre-eclampsia, HELLP syndrome, and other medical conditions, it can lead to adverse consequences for both the mother and the baby, depending on the extent of liver damage (13).
5. Are there any natural remedies for jaundice in pregnancy, and are they safe to use?
There are numerous natural ways to manage jaundice during pregnancy. These include maintaining a nutritious diet, staying hydrated, reducing stress, engaging in gentle exercise, using essential oils for relaxation, and choosing paraben-free and eco-friendly personal and household products (15). Dandelion Root and Milk Thistle are natural remedies for pregnancy-related jaundice, but consulting a healthcare provider is crucial to ensure their safety and effectiveness (16).
6. Is breastfeeding safe with jaundice during pregnancy, or should the baby be formula-fed?
Breastfeeding is safe if you have jaundice during pregnancy. Doctors may recommend continuing medications to normalize bile acids in the blood, which can pass into breast milk. These medications can assist the baby’s immature liver eliminate residual bile acids while it aids in managing jaundice. Formula feeding is not necessary in this case. Consult your doctor for guidance on breastfeeding (17).
Infographic: Measures For Preventing Jaundice During Pregnancy
Jaundice can affect pregnant women during any phase but is most common in the last trimester, and it may cause adverse complications when not treated promptly. Therefore, you may follow the preventive measures explained in this infographic to reduce the risk of jaundice during pregnancy. Illustration: Momjunction Design Team
Are you pregnant and worried about being diagnosed with jaundice during this beautiful journey? Watch the video given below to acquire valuable tips for treatment, offering guidance during your pregnancy journey.
Illustration: Jaundice In Pregnancy: Causes Symptoms Treatment And Risks

Image: Dall·E/MomJunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i.How I knew I had cholestasis during pregnancy.https://www.youtube.com/watch?feature=shared&v=2SrgtYZrowE
References
1. Saketh R. Guntupalli and Jay Steingrub, Hepatic disease and pregnancy: an overview of diagnosis and management; Critical Care Medicine
2. Sherlock S.,Jaundice in pregnancy; British Medical Bulletin
3. Hay J. E.,Liver disease in pregnancy;American Association for the Study of Liver Diseases
4. Adult Jaundice; Cleveland Clinic
5. Weng M.T.et al., Hyperemesis gravidarum presenting as jaundice and transient hyperthyroidism complicated with acute pancreatitis; Journal of the Formosan Medical Association
6. Intrahepatic cholestasis of pregnancy; U.S. national Library of Medicine
7. Gupta A., Tiwari P., and Sachdeva P., A Case of Dubin-Johnson Syndrome in Pregnancy; Cureus
8. Liver Disease in Pregnancy; American Academy of Family Physicians
9. Liver disease and diet.University Hospitals Conventry and Warwickshire
10. All You Need to Know about Jaundice in Pregnancy; Sitaram Bhartia Institute of Science and Research
11. Diet For People With Jaundice; Health Online Unit, Ministry of Health Malaysia
12. Jaundice in Pregnancy; Association of Physicians of India
13. All You Need to Know about Jaundice in Pregnancy; Sitaram Bhartia Blog
14. Prolonged postpartum course of intrahepatic cholestasis of pregnancy; National Library of Medicine
15. Self Help for Intrahepatic Cholestasis of Pregnancy (ICP);; ICP Care
16. Cholestasis of Pregnancy: Causes, Symptoms & Treatment; American Pregnancy Association
17. Symptoms of Intrahepatic Cholestasis of Pregnancy;; ICP Care
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Mozhgan Sayyad
Read full bio of Dr Bisny T. Joseph
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das






 Caution
Caution