Image: Shutterstock
Jock itch (tinea cruris) in kids is a fungal skin infection seen in children who sweat profusely and often swim in public pools. The jock itch is an infection commonly occurring in and around the moist areas of the body, such as the upper thighs and the privates. Therefore, this infection is mostly associated with athletes, however, it can occur in children, especially during the summer months, when they are sweating profusely.
The main clinical manifestation of this infection is a ring-shaped fungal rash, which can cause redness and itchiness in the affected area. In some children, the infection may spread to the surrounding areas, causing discomfort and irritation. However, it is usually not very serious and can be managed with good hygiene practices and over-the-counter (OTC) antifungal medications.
Read this post to learn more about the symptoms and causes of the jock itch and whether the infection is contagious.
Key Pointers
- Jock itch is a fungal infection caused by any fungus belonging to the group dermatophytes.
- The infection mainly occurs in those who are obese, sweat excessively, wear tight clothing, or have a weak immune system.
- Jock itch is contagious and looks like a ring with a clear center and raised edges.
- Mild infections clear with antifungal creams and ointments, while severe conditions need prescription oral or topical medications.
What Causes Jock Itch In Children?
Jock itch, medically known as tinea cruris, is a fungal infection caused by any fungus from a group of fungi called dermatophytes(1)(2)
. Infections caused by these fungi are known as tinea infections (3).
The fungus usually lives on skin, nails, and hair. Prolonged heat and moistness in an area can cause the fungus to multiply and cause jock itch infection. When the infection occurs as an upper thigh, buttocks, and groin rash, it is known as jock itch. If feet are affected, it is called athlete’s foot, and if the infection occurs on the other parts of the body, it is referred to as ringworm in kids.

Why Is It Called Jock Itch And Who Is At Risk Of Getting It?
The rash is known as jock itch, as it is most common in athletes. The following are some of the factors that can increase the risk of getting a jock rash (4).
- Boys are said to be more likely to get it than girls.
- Obese children have a high chance of developing this rash, as their skin folds provide a conducive climate for the fungus to thrive.
- Children who are physically active or sweat excessively (hyperhidrosis).
- Children who actively play contact sports, such as football, martial arts, and boxing, are at higher risk because of skin friction and sweat.
- Those who share pools or locker rooms since they might catch the fungus from others.
- Wearing tight clothing and undergarments traps the moisture and aids in the development of the infection.
- Children with a weak immune system and diabetes.

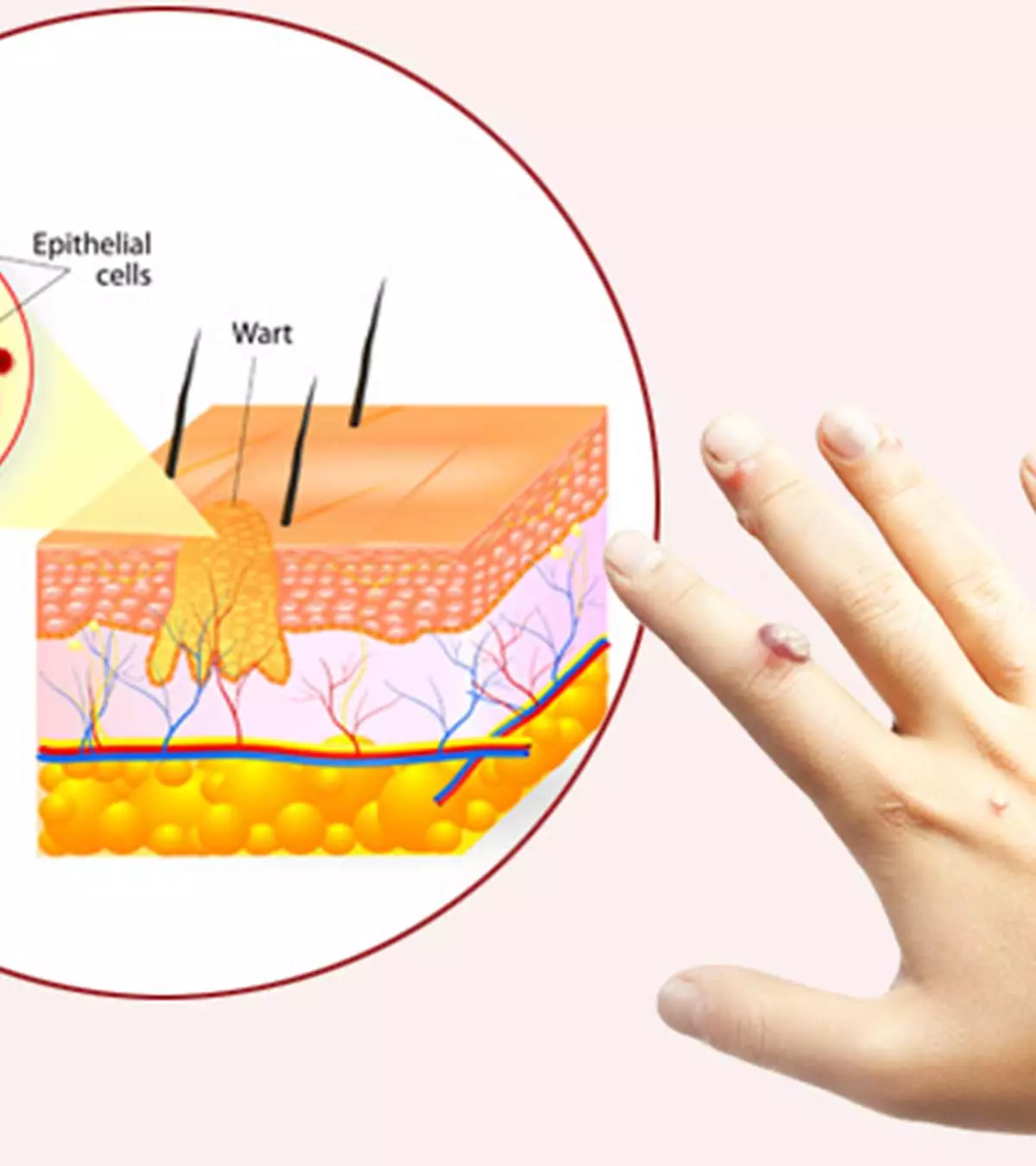
Signs And Symptoms Of Jock Itch
- Red, itchy groin or inner thighs accompanied by rashes.
- Spreads in a ring-like circular pattern, and the center appears clear.
- The edges are raised and red in color.
Many times, parents confuse jock itch with other skin infections like eczema and heat rashes. Therefore, knowing the symptoms, appearance, and location of jock itch is essential to prevent misdiagnosis. Your doctor would perform a physical examination to determine the infection. They would also enquire about your child’s medical history, lifestyle, and hygiene habits. A small flake of the rash may be sent for a lab test or examined under a microscope to check for the presence of fungus.
 Things to know
Things to knowIs Jock Itch Contagious And How Long Does It Take to Heal?
Yes, jock itch can spread from one child to another through skin contact, contaminated towels, and clothing. In the case of athlete’s foot in children, the fungus can travel from the feet to the groin through clothes, hands, or a towel. It can also spread from animals to humans.
Mild cases of jock itch clear up in two to four weeks. If the infection is severe and has spread to the nails and scalp, then it might take up to three months to get cured. However, studies note that the fungal spores can live on bedding and towels for a year if these are not properly washed (2). Therefore, it is essential to take proper steps to contain the skin infection.
Treatment For Jock Itch In Children

Mild infections can be cured with over-the-counter (OTC) antifungal treatments such as creams and ointments. However, severe conditions could require prescription oral or topical medications. If the infection does not subside in two weeks with OTC medications or worsens, see a doctor (1). The doctor may prescribe stronger antifungal medications, along with comprehensive skincare routines, to prevent the recurrence of jock itch.
Along with medication, you may need to follow the below measures for skin care for kids to help relieve the itching and discomfort.
- Wash the infected area and dab dry it with a clean towel. Don’t rub the affected area with the towel as it will worsen the rash and increase the likelihood of spread.
- Change the clothing and undergarments every day.
- Avoid tight clothing that can further irritate the rash.
It should be noted that you need to continue the medication until the period prescribed by the doctor, even when the symptoms disappear, to eliminate the fungus.
Prevention Of Jock Itch In Children
Adequate precautions and good personal hygiene can protect children from jock itch (3).
- Keep groins clean and dry.
- Shower after playing sports.

- Change undergarments daily.
- Wear loose clothing during warm or humid weather.
- Choose breathable cotton undergarments and avoid tight polyester undergarments.
- Periodically wash gym outfits, sports outfits, towels, and bed sheets with warm water and detergent.
- Do not share clothes or towels with others.
- Avoid public showers or shared locker rooms as much as possible.
If someone in the family has jock itch, then keep their belongings separately to prevent the spread of infection.
 Quick tip
Quick tipHome Remedies For Jock Itch
Along with the antifungal medications, you can also follow a few home remedies to reduce the healing time. However, it should be noted that these remedies may have little scientific backing, so it is best to use them only after informing your child’s doctor.
1. Apple cider vinegar
The antifungal properties are said to hasten the healing process. Dilute apple cider vinegar with water, dip a cotton ball, and dab over the rashes; do it thrice a day for better results (5).
2. Tea tree oil
Studies found that using tea tree oil twice daily could be effective in children with tinea pedis(6)
. Mix tea tree oil with coconut or olive oil and dab it on the rashes. Do this three to four times a day.
 Quick tip
Quick tip3. Turmeric
Turmeric’s antifungal properties are said to be useful in providing relief from the rash and itching caused by tinea infections (7). Turmeric for children can also be beneficial. Mix turmeric with a little water and apply the mixture on the rashes.
4. Garlic
Studies suggest that garlic exhibits antifungal properties that might be effective against dermatophyte fungi. Crush some garlic and mix it with olive oil to make it into a paste, apply it on the rashes and leave it for 30 mins (8).
5. Neem and aloe vera

Research suggests that a mixture of aloe vera and neem inhibits the growth of fungus in tinea infections (9). Grind and paste neem leaves, mix it with aloe vera gel, apply it on the rashes, and leave it for 20 mins.
6. Honey
Studies say that honey could be therapeutic in the treatment of tinea infections (10). Dip a clean cotton ball in honey, dab it on the rashes, and let it stay for 15 minutes before rinsing. Repeat this for three to four times a day using a new cotton ball each time.
7. Coconut oil
Coconut oil
is known for its antifungal properties and can be used to quicken the healing time of jock itch. Apply virgin coconut oil on the rashes and rinse it after ten minutes. Repeat at least two to three times a day (11).
8. Lemon oil
Studies suggest that lemon oil has antifungal properties and might inhibit the growth of dermatophyte fungi (12). Add two to three drops of lemon oil in one tablespoon of coconut oil, dab it on the affected area, and leave it for 30 minutes. You can do this daily until the rashes begin to subside.
Note that these home remedies should be used in conjunction with the treatment. Also, these remedies might take time to show effect. If a home remedy causes a burning sensation or discomfort to the child, then stop using it.
Frequently Asked Questions
1. Can girls get a jock itch?
Although jock itch is more common in boys, girls can get it too.
2. How do I know if my child’s jock itch is healing?
The jock itch is healing when the rashes and redness begin to subside, and the skin regains its original color. Also, you will find a reduction in itching and irritation.
3. Can I leave jock itch untreated?
If left untreated, jock itch can spread to other body parts and to other family members. It may also lead to secondary infections.
4. What is the fastest way to cure jock itch?
Using a prescription antifungal cream, gel, spray, ointment, or powder in dosage and frequency as advised by the healthcare professional is the fastest and most effective way to treat jock itch in children (13).
5. Is hydrocortisone good for jock itch?
The topical application of prescribed hydrocortisone may relieve inflammation and related irritation due to the fungal infection. However, the medicine is a topical steroid and not an antifungal. Therefore, it may be combined with antifungal medications (14).
6. Is hot water good for jock itch?
Running cool water over the affected area may help alleviate symptoms such as itchiness and skin irritation. Using hot water for tinea cruris may instead worsen your itchiness. Check with your doctor before trying any home remedies (15).
A ring-like rash, redness around the ring, and intense itching are the signs of jock itch (Tinea Cruris) in kids. Since this fungal infection is common in areas with excess moisture such as thighs, buttocks, or the groin, wearing loose clothing and maintaining proper personal hygiene could be helpful. Because the infection is contagious, have your children refrain from sharing clothes with others. Over-the-counter medications such as antifungal creams are effective for mild infections. If the condition persists or worsens, consult a dermatologist. You may also try a few home remedies to reduce the healing time after seeking a doctor’s approval.
Infographic: How To Prevent Jock Itch In Children?
Jock itch is a fungal infection that causes rashes and itchiness around the groin, upper thighs, and buttocks. While there are many risk factors for developing jock itch in children, the measures in the infographic below can help prevent the infection in children easily.

Illustration: Momjunction Design Team
Understand effective methods to treat jock’s itch effortlessly! Eliminate bothersome itchiness and redness using this user-friendly instructional video.
References
1. Jock itch; U.S. National Library of Medicine
2. Dermatophytosis; The Center for Food Security & Public Health
3. Jock Itch (Tinea Cruris); Harvard Medical School
4. Ramdas B. Darade, Krushna K. Zambare, Nareshkumar R. Jaiswal and Amar A. Kaware; An Overview On Pharmacotherapy Of Jock Itch (Tinea Cruris); World Journal of Pharmaceutical Research
5. Judy Gopal, Antonydhason Vimala, Manikandan Muthu, and Enkhtaivan Gansukh; Authenticating apple cider vinegar’s home remedy claims: antibacterial, antifungal, antiviral properties and cytotoxicity aspect; Research Gate
6. C. F. Carson,K. A. Hammer, and T. V. Riley; Melaleuca alternifolia (Tea Tree) Oil: a Review of Antimicrobial and Other Medicinal Properties; American Society For Microbiology
7. Mukda Jankasem, Mansuang Wuthi-udomlert,and Wandee Gritsanapan; Antidermatophytic Properties of Ar-Turmerone, Turmeric Oil, and Curcuma longa Preparations; ISRN Dermatology
8. Farzad Aala, Umi Kalsom Yusuf, Rosimah Nulit,and Sassan Rezaie;Inhibitory effect of allicin and garlic extracts on growth of cultured hyphae; Iranian Journal of Basic Medical Sciences.
9. Vivek Shukla, Gyan Vikas Mishra, and Mitesh Dwivedi; In Vitro Inhibition of Tinea Corporis from Various Extracts of Aloe vera and Azadirachta indica; Acta Scientific Microbiology.
10. PaulineMcLoone, MaryWarnock, and LornaFyfe; Honey: A realistic antimicrobial for disorders of the skin; Journal of Microbiology, Immunology and Infection
11. Lindsey K. Elmore, Gwen Nance, Samantha Singleton, and Luke Lorenz; Treatment of Dermal Infections With Topical Coconut Oil; Natural Medicine Journal
12. Sabrina P. M. Pinontoan, Nurmila Sunati, Befani Aditya Febriana, and Elne Vieke Rambi; Antifungal Activity of Essential Oil Extract of Lemon Cui (Citrus microcarpa) Skin against Trichophyton rubrum Growth; International Journal of Pharma Medicine and Biological Sciences
13. Jock Itch (Tinea Cruris); Cleveland Clinic
14. Alok Kumar Sahoo and Rahul Mahajan; (2016); Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review; National Library of Medicine
15. Jock Itch; Sutter Health
16. Jock Itch; Seattle Children’s
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Pooja Parikh
Read full bio of Dr. Ritika Shah
Read full bio of Rebecca Malachi
Read full bio of Ghazia Shah