Image: Shutterstock
Low-dose birth control pills are hormonal contraceptives with lower concentrations of synthetic hormones (estrogen and progestin) than traditional pills. When used correctly, these are just as effective as conventional pills in preventing unwanted pregnancies. Besides, they are considered safer and may have fewer side effects due to lower hormone levels (1). However, their use may be contraindicated in some cases. Thus, using them under medical guidance is essential. Experts recommend taking these pills consistently, same time every day, to ensure their effectiveness. Keep reading to learn about the types of low-dose birth control pills, their mode of action, benefits, side effects, and alternative birth control methods.
Key Pointers
- Low-dose birth control pills contain lower levels of hormones – estrogen and progesterone.
- They are 99% effective in preventing unwanted pregnancy when taken at the same time daily.
- The dosage and frequency of these pills can vary depending on certain factors, such as pre-existing medical conditions.
- Their use under medical guidance helps ensure their effectiveness and reduces the risk of any side effects.
What Is A Low-Dose Birth Control Pill?

Image: IStock
Low-dose birth control pills are a prescription medication and oral contraceptives with lower levels of synthetic estrogen and progesterone (progestin) hormones. These pills are available in standalone (minipill – progestin only) and combination (estrogen and progestin) forms. Their main goal is to reduce the risk of side effects that could occur with high-dose oral contraceptives.
Estrogen combination pills are preferred to progestin-only pills since the former is known to cause fewer side effects (2). The dosage of estrogen hormone in these oral contraceptives is around 30 micrograms (20 for very low-dose pills), as opposed to the standard 30-50 micrograms found in traditional high-dose pills (3). However, the dosages may vary, and the pills may contain between 20-35 micrograms of estrogen (4).
What Are The Types Of Low-Dose Birth Control?
A low-dose birth control pill may be of the following types (6) (7).
1. Combined Hormonal Contraceptives
These hormonal contraception pills contain estrogen and progestin hormones. A few examples (brand names) include:
- Yasmin (Drospirenone and Ethinyl estradiol (in 30mcg))
- Levlen ED (Levonorgestrel and Ethinyl estradiol (in 30mcg))
- Ortho Tri-Cyclen Lo (Norgestimate and Ethinyl estradiol (25mcg))
- Femme-Tab ED (Levonorgestrel and Ethinyl estradiol (in 30mcg))
- Ultra-low dosage pills such as Femme-Tab ED (Levonorgestrel and Ethinyl estradiol (20 mcg) and Yaz (Drospirenone and Ethinyl estradiol (20mcg))
2. Progestin-Only Oral Contraceptives
These pills contain only progestin hormone and are usually prescribed when estrogen use is contraindicated or not well-tolerated (2). A few examples of these pills are Errin, Camilla, and Micronor (8). Estrogen could be contraindicated in individuals with cancer, a history of stroke, autoimmune diseases, high blood pressure, and migraines.
 Point to consider
Point to consider3. Other Non-Oral Contraceptives
These may be used as low-dose combinations and include combined hormonal patches and combined vaginal ringsiA flexible, soft ring inserted into a woman’s vagina to prevent pregnancy . However, there is not much information regarding their use in a large population of women (9).

Image: Shutterstock
Who Should Go For Low Estrogen Pills?
A doctor usually prescribes a low-dose pill equal to or below 35 micrograms.
However, when using a combined hormonal method, certain factors might influence the dosage or whether or not a woman should consume these pills. Generally, low-dose estrogen birth control pills are prescribed to women who may be more susceptible to side effects from higher doses of estrogen. These include the following factors (6).
- History of cardiovascular disease
- Being overweight
- Age greater than 35 years
- Smoking
- High blood pressure
- Diabetes
- History of headaches such as migraine

Image: Shutterstock
Note: Very low doses of estrogen (tablets with 20mcg or lower quantities of estrogen) are not advisable for women above 40 with a history of deep vein thrombosisiA medical condition where blood clots develop in one or more deep veins or breast cancer (3).
How Does Low-Dose Birth Control Work?
Low-dose birth control pills with estrogen and progestin block the release of eggs from the ovaries and prevent ovulation.
Additionally, they thicken the cervical mucus, making it difficult for the sperm to fertilize the egg. Furthermore, some pills alter the uterine lining, making the environment in the uterus less hospitable for implantation (10).
 Point to consider
Point to considerHow Does Low-Dose Birth Control Affect Your Period?
The progestin component of the pill prevents pregnancy, while the estrogen component regulates menstrual bleeding (11). According to some studies, oral contraceptives suppress ovulation and reduce endometrial tissue growth, which helps alleviate menstrual blood flow and prostaglandiniA group of lipids that act like hormones, performing different functions production. These changes might help control heavy blood loss, pain during menstruation (12), and symptoms associated with premenstrual syndromeiA cluster of symptoms a woman may experience before her period (6).

Image: IStock
What Are The Advantages Of Low-Dose Birth Control Pills?
Besides preventing unwanted pregnancy, a low-dose birth control pill may also confer a few health advantages, including reduced likelihood of (13) (14):
- Irregular or painful periods
- Ectopic pregnancy
- Iron deficiency anemia
- Skin conditions, particularly acne
- HirsutismiExcessive hair growth on the face and other body parts
- Gynecological cancers, including uterine, endometriumiInner lining of the uterus, shed during a menstrual period in females , and ovarian cancers
What Are The Side Effects Of Low-Dose Birth Control Pills?
Although these pills are highly efficacious and may benefit women’s health, they also come with the possible risks of a few adverse effects, including (6) (11):
- Abnormal or breakthrough bleeding
- Headaches
- Tender or sore breasts
- Elevated blood pressure
- Nausea
- Abdominal pain
- Reduced sexual drive
- Bloating or water retention
- Increased body weight

Image: IStock
If you notice any of these side effects after consuming a pill, contact your gynecologist to prevent any long-term health complications.
 Point to consider
Point to considerWhat Are The Alternatives For Low-Dose Birth Control?
Apart from oral contraceptive pills, other successful pregnancy prevention methods include:
- Contraceptive implantiA small rod-like device placed under the skin of a woman’s upper arm for birth control
- Intrauterine devices (IUDs)
- Hormonal injection or shot
- Birth control skin patch
- Contraceptive vaginal ring
According to the US Centers For Disease Control And Prevention (CDC), the above contraceptive methods have around or less than 7% failure rates. Also, once administered, they help prevent pregnancy from a few weeks to months (16).
Frequently Asked Questions
1. How long does it take for low-dose birth control to be effective?
A low-dose contraceptive pill generally takes about seven days to begin working as a form of birth control. However, if the medication is being taken for other conditions, such as acne or irregular bleeding, it may take several months (3-4 months) to see a significant improvement (17).
2. How long does it take for low-dose birth control to leave my system?
Low-dose pills typically metabolize and get cleared from the body quickly, usually in less than a week or even a couple of days (18) (19). However, if you are considering discontinuing these pills and trying to conceive, you should speak to your doctor about any necessary precautions to consider.
3. Can I still get pregnant on birth control?
When taken consistently in appropriate dosages, a low-dose pill is about 99% effective in preventing unintended pregnancy. However, if not appropriately used, approximately 9% of women may conceive while using the pill (20).
4. Do I get my period while on birth control?
The menstrual cycles may be affected by the type of birth control method used. Some birth control methods, such as hormonal pills, alter your menstrual cycle, including heavier or lighter periods or even no periods at all. On the other hand, methods such as IUD are not known to affect the menstrual cycle (21).
Low-dose birth control pills contain lower levels of hormones, making them a preferable contraception method for many women. Generally, they are 99% effective in preventing unintended conception and may lower your risk of certain health issues, such as ovarian cancer. However, certain pre-existing health conditions and medications may raise the risk of side effects associated with this contraception method. Therefore, it’s crucial to speak to your healthcare provider and determine the best birth control plan for you, considering your overall health and desired birth control goals.
Infographic: What Are The Uses And Side Effects Of Low-Dose Birth Control?
Low-dose birth control pills are considered to have lesser side effects than traditional hormonal pills. Besides, they are also known to be beneficial in treating and/or managing other medical issues, such as irregular menstruation and endometriosis. However, they may have adverse effects in some cases. Read our infographic below to learn about the possible benefits and disadvantages of low-dose birth control pills, which will help make you an informed choice.
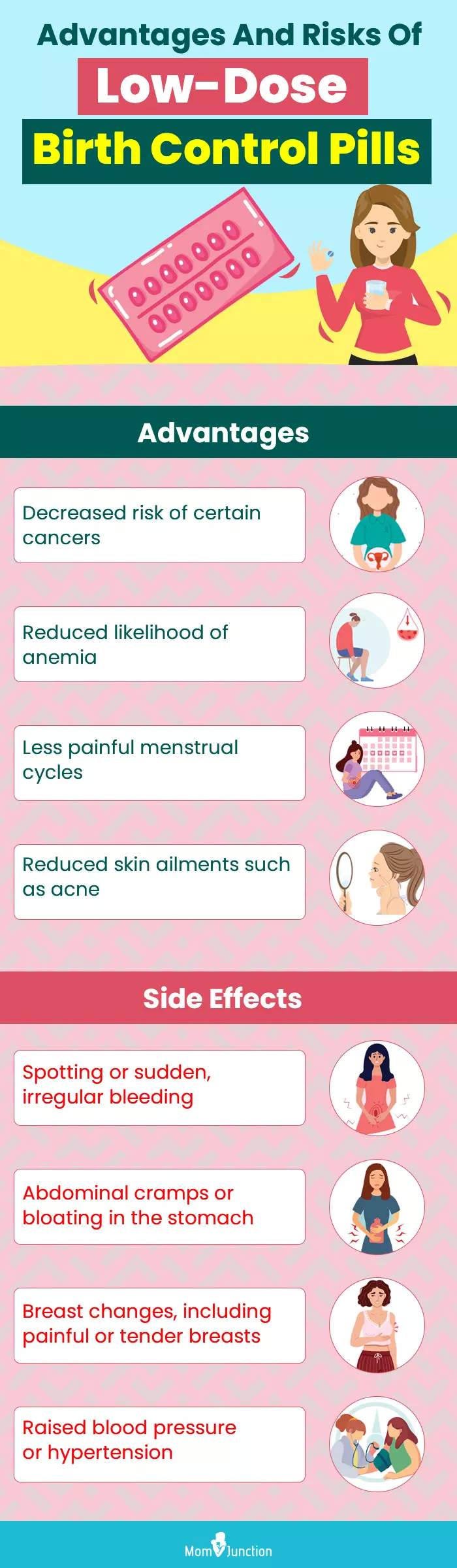
Illustration: Momjunction Design Team
Illustration: Low-Dose Birth Control: Types Advantages And Side Effects

Image: Stable Diffusion/MomJunction Design Team
Are you confused about low-dose birth control? Learn how to use low-dose birth control with this helpful video. Get answers to all your questions about the effectiveness, side effects, and more.
References
- Birth control methods.
https://www.womenshealth.gov/a-z-topics/birth-control-methods - Frances E. Casey; Oral Contraceptives.
https://www.msdmanuals.com/en-in/professional/gynecology-and-obstetrics/family-planning/oral-contraceptives - Very-Low-Dose Birth Control Pills in Mid-Life (Perimenopause).
https://www.aafp.org/pubs/afp/issues/1998/1015/p1381.html - Sheila Krishnan and Jessica Kiley; 2010; The lowest-dose extended-cycle combined oral contraceptive pill with continuous ethinyl estradiol in the United States: a review of the literature on ethinyl estradiol 20 μg/levonorgestrel 100 μg + ethinyl estradiol 10 μg.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2990890/ - Regine Sitruk-Ware Et Al. (2013); Contraception Technology: Past Present And Future.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3530627/ - Mary Stewart et al. (2015); Choosing a combined oral contraceptive pill.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4654044/#!po=16.6667 - Kelli Stidham Hall and James Trussell; (2012); Types of combined oral contraceptives used by U.S. women.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3469779/ - Kelli Stidham Hall et al. Progestin-only contraceptive pill use among women in the United States.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3440515/#!po=31.2500 - Classifications for Combined Hormonal Contraceptives.
https://www.cdc.gov/contraception/about/index.html - Estrogen and Progestin (Oral Contraceptives).
https://medlineplus.gov/druginfo/meds/a601050.html - Cooper DB et al. Oral Contraceptive Pills.
https://www.ncbi.nlm.nih.gov/books/NBK430882/ - Tasuku Harada et al. Low-dose oral contraceptive pill for dysmenorrhea associated with endometriosis: a placebo-controlled double-blind randomized trial.
https://www.fertstert.org/action/showPdf?pii=S0015-0282%2807%2903394-8 - Noncontraceptive health benefits of combined oral contraception.
https://academic.oup.com/humupd/article/11/5/513/606151 - Jeffrey T.Jensen and LeonSperoff; Health Benefits Of Oral Contraceptives.
https://www.sciencedirect.com/science/article/abs/pii/S0889854505701698?via%3Dihub - R Ansbacher; Low-dose oral contraceptives: health consequences of discontinuation.
https://pubmed.ncbi.nlm.nih.gov/11239614/ - Contraception.
https://www.cdc.gov/contraception/about/index.html - Birth Control: The Pill.
https://my.clevelandclinic.org/health/drugs/3977-birth-control-the-pill - How Soon Can You Get Pregnant After Stopping Birth Control?
https://healthcare.utah.edu/the-scope/shows/1_38px3nd9 - Should You Try a Birth Control Cleanse?
https://health.clevelandclinic.org/birth-control-cleanse - How effective is contraception at preventing pregnancy?
https://www.nhs.uk/conditions/contraception/how-effective-contraception/ - P G Stubblefield; Menstrual impact of contraception.
https://pubmed.ncbi.nlm.nih.gov/8178900/#
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Ben Abbes Taarji Hicham
Read full bio of Vidya Tadapatri
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das







 Did you know?
Did you know?