Image: Midjourney/ MomJunction Design Team
Hypothermia is characterized by the body’s temperature dropping below the normal range. While it may occur in both adults and children, low temperature in babies can be a cause for concern because infants cannot maintain their body temperature. If prompt treatment is not provided, low body temperature may lead to complications (1). Regular monitoring of the baby’s temperature is vital for early detection and timely intervention. Read this post to learn about the causes, risks, symptoms, and preventive measures for low temperature in babies.
Key Pointers
- A baby is said to have a low temperature when its body temperature drops below 97.7°F (36.5℃).
- Hypothermia or low temperature in babies is a complication that needs immediate medical attention as infants can’t regulate their body temperature.
- Parents should pay attention to early signs of hypothermia in babies to arrange prompt care necessary to avert complications.
- Babies can develop hypothermia due to medical and non-medical reasons, like bathing the baby immediately after birth.
- Unless the cause for hypothermia is an underlying medical condition, parents can prevent the low temperature in babies by ensuring appropriate care during and after childbirth.
How To Know If Your Baby Has Low Temperature?
According to the guidelines released by the Whole Health Organization (WHO), essential care is required during delivery and the initial days after birth as a newborn’s body is not yet developed to regulate the body temperature.
The average body temperature of an infant ranges between 35.5℃ and 37.5℃ when measured orally, 36.6℃ and 38℃ when measured rectally, 35.8℃ and 38℃ when measured through the ear, and 36.5℃ and 37.5℃ when measured in the armpit.
Your baby is said to be hypothermic when their body temperature drops below 36.5℃. This condition can be classified into three stages:
It is recommended that you measure the temperature of babies below five years of age through the rectum for an accurate reading (2).
 Quick tip
Quick tipSigns Of Hypothermia In Babies

It is important to detect the signs of hypothermia in your baby early on, as it would help you identify it in the early stages. Dr. Andrea Wadley, MD, IBCLC, a lactation consultant from Bedford, Texas, says, “Young babies don’t always have many symptoms that would alert you to their low temperature. A baby with a low body temperature will often feel cool to the touch. They may shiver or have goosebumps. They may also have a bluish hue around their lips and a lacy-appearing rash over their bodies. Blue hands and feet can also signify a cold baby.”
- The feet become cold before the body gets chilly.
- Weakness or inability to suck while breastfeeding
- Sluggish and slow reactivity to stimuli
- Weak and shallow cry
Beyond this stage, the baby would be at risk of developing a cold injury, which is characterized by lethargy; slow, shallow, and irregular respiration; slow heart rate; low blood sugar; and metabolicacidosisiA condition in which the pH of the blood is too low due to an excess of acid caused by various factors, including metabolic disorders. .
Other severe symptoms of hypothermia include reddening of the face and extremities, central cyanosis, and hardening of the skin on the back and limbs (1). These symptoms are risky and might need medical attention.
 Quick fact
Quick factNext, let us look at some of the causes of low body temperature in babies.
Causes Of Low Body Temperature
Hypothermia is a serious yet preventable complication in babies. Knowing the causes of low body temperature might help you prevent it.
1. Prematurity and low birth weight

Infants born with a birth weight less than 1,500g and born at a gestation period of fewer than 28 weeks are at a 30 to 78% chance of developing hypothermia. In a study by Iowa Center for Research, among 532 premature and very low birth weight infants studied, 421 infants had low body temperature, with about 66% of them having moderate to severe hypothermia.
Preterm and low birth weight babies are at a higher risk of developing hypothermia because of the following factors.
- A large surface-area-to-volume ratio
- Immature skin with minimal stratum corneumiOutermost layer of the epidermis, composed of dead skin cells that form a protective cover against the environment.
- A thin layer of insulating fat
- Poor vasomotor controliRegulation of blood vessel diameter by the autonomic nervous system, affecting blood pressure and blood flow to different organs.
- Lack of heat production in the body
Also, environmental factors, such as low ambient air temperature and low surface temperature of the beds, might contribute to hypothermia in preterm babies
.
If a baby is about to be born preterm or with low birth weight, the baby should be wrapped in a polyethylene wrap (to prevent drying) immediately after the delivery. Heating and incubator systems or heated mattresses can also be used to keep the baby warm (3).
2. Environmental factors
Environmental factors during birth might cause the newborn’s body to lose heat, leading to hypothermia. Within the first minutes after birth, the baby’s skin temperature falls by 3 to 4℃. Leaving the baby unattended after birth, delaying the drying and wrapping, and bathing the baby immediately after birth may increase the risk of hypothermia in newborns (4).
3. Hypoglycemia
Hypoglycemia can also cause hypothermia in babies. It is a condition in which the blood sugar or glucose levels are low in the body. Babies can become hypoglycemic at birth or later. It is usually seen in
- Babies with intrauterine growth restriction (IUGR)
- Babies of Diabetic mothers or large-for-gestational-age (LGA) infants
- Preterm babies of 34–36.6 weeks
- Infants with perinatal stress (fetal distress, maternal high blood pressure (preeclampsia))
- Babies born to a family with a history of diabetes (5)
4. Infections

In a few cases, hypothermia can be a symptom of severe infections in babies. Two such infections are meningitis and neonatal sepsis.
Meningitis is a bacterial infection that causes inflammation of the spinal cord membranes. It may sometimes cause fever in babies, or there could be a drop in their body temperature. Along with hypothermia, you may also notice symptoms such as irritability, lethargy, feeding difficulties, respiratory distress, and seizures (6).
Sepsis refers to the body’s extreme reaction to a bacterial infection. In newborns, it may lead to inflammation and organ failure. A drop in body temperature is one of the symptoms of sepsis. Along with hypothermia, you may also notice feeding difficulties, irritability, vomiting, and lethargy (7).
Both these infections are severe in neonates, and they may require medical help.
5. Deficiencies
Some rare metabolic disorders such as Aromatic L-amino acid decarboxylase deficiency, Menkes diseaseiA rare genetic disorder that affects copper metabolism in the body, leading to damage in the brain and other organs , and Coenzyme Q10iA naturally occurring substance in the body that helps produce energy in cells and acts as an antioxidant. deficiency may also cause a drop in the body temperature in babies. These are rare and may cause lethargy, feeding difficulties, seizuresiSudden, abnormal electrical activity in the brain causing symptoms such as convulsions, loss of consciousness, and muscle spasms. , and weak muscle tone.
Additional risk factors include:
- A large body surface area in relation to their weight
- A large head in proportion to the body as newborns lose 75% of body heat through the uncovered head.
- Asphyxia (low oxygen levels) (1)
If you spot any of the above signs and risk factors, it is best to talk to your pediatrician.
 Experts say
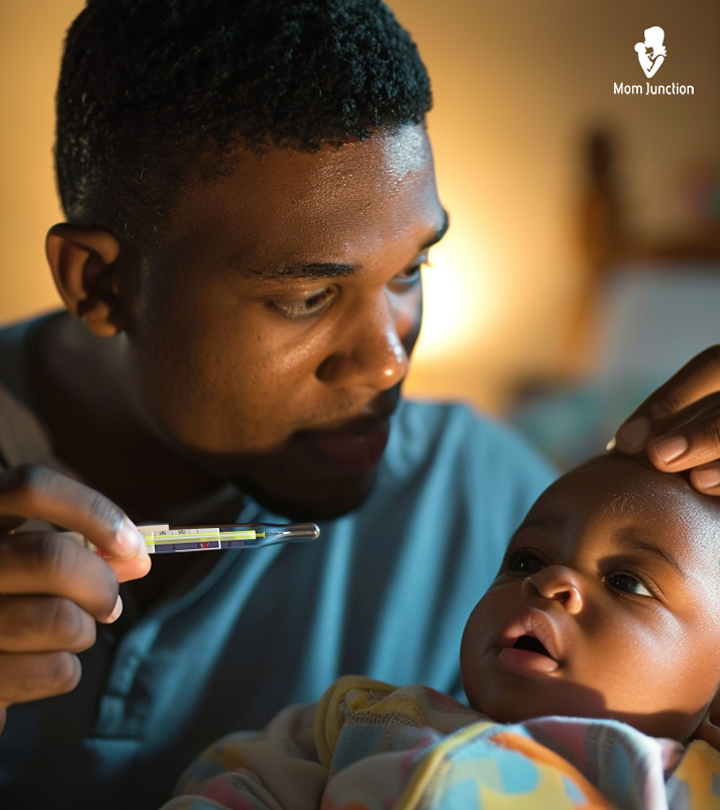
Experts sayDr. Wadley recommends, “If your baby feels cold to the touch, the first thing you should do is to measure their temperature rectally. If their temperature is below 97.5°F, you should attempt to warm the baby by wrapping them in warm layers, including a blanket. If their temperature continues to be low after about an hour of warming them up, you should call your pediatrician if your baby is less than three months old.”
The next section covers a few ways in which you can prevent hypothermia in babies.
How To Prevent Hypothermia In A Newborn?
If your baby’s doctor rules out underlying medical reasons, hypothermia can be prevented in babies. First and foremost, appropriate care should be taken during and after delivery to avoid the loss of temperature from the body. The baby should not be left unattended and bare on a table or the bed. Also, awareness of parents regarding proper infant care and the potency of environmental conditions like exposure to cold weather leading to hypothermia in babies can help prevent this condition.
Here are a few steps you can take:
- Ensure the hospital adheres to the warm chain system of keeping the baby warm to prevent hypothermia during birth. The warm chain is a set of interlinked events, including:
- Keeping the delivery room clean and maintaining the ideal room temperature for babies.
- Ensuring the room does not have a draught through the windows or doors
- Immediately drying the infant with a clean towel and avoiding bathing at this time
- Wrapping the baby in layers of loose clothing and never placing them naked on a table
- Encouraging skin-to-skin contact with the mother and initiating breastfeeding

All these steps are applicable to full-term babies with normal vital signs, too. If your baby is born prematurely, talk to your doctor for special care instructions.
- Once your baby is home, you can try some of the below techniques to keep the baby warm.
- Always keep your baby covered in layers of loose-fitting and warm clothes, and make sure their head is always covered. “The general rule is to dress your baby in one extra layer than you would dress yourself. For outdoor events in the cold, generally adding a blanket to your baby’s layers works well to keep them warm,” suggests Dr. Wadley
- Swaddle the baby in a single blanket; however, follow the safety rules while doing it.
- According to the American Academy of Pediatrics, tub baths should be postponed until the umbilical cord falls off. Instead, a sponge bath should be given (8). This also helps limit the evaporation of moisture from the body.
- Follow the Kangaroo method in which the baby is placed in between the mother’s breasts wearing nothing except a diaper.
- Bathe the baby with lukewarm water. Do not let them be in the water for an extended period, and make sure you wrap them in a dry towel immediately after the bath.
 Experts say
Experts say- To help prevent hypoglycemia in babies, feed your baby frequently. Also, speak to your doctor, and maintain a healthy diet during pregnancy.

Frequently Asked Questions
1. What are the stages of hypothermia in babies?
Hypothermia can be classified into three stages: — mild (35-32°C), moderate (32-28°C), and severe (below 28°C). As the severity of hypothermia increases, the baby might show signs of unconsciousness, decreased breathing, and rigid muscles. While shivering is a sign of mild hypothermia, it might stop as the cold intensity increases (9).
2. Why is it important to prevent hypothermia in newborns?
Severe hypothermia could decrease the heartbeat, which could be life-threatening. Since a decrease in body temperature might also increase the rigidity of the muscles and affect the pulse and respiratory rate, it is essential to prevent hypothermia in newborns.
3. Is there a difference between low temperature in babies and adults?
Babies have a larger surface area-to-body mass ratio, a limited ability to produce heat, and less effective temperature-regulating mechanisms than adults, which is why babies can experience low body temperature more easily than adults (11).
4. Are there any nutritional deficiencies that can cause low temperature in babies?
Inadequate consumption of vital nutrients and minerals such as iron and vitamin B12 might influence metabolism and thermoregulation, potentially leading to reduced body temperature (12) (13).
5. Can a baby’s temperature fluctuate due to teething or other illnesses?
While teething is not typically associated with a high fever, some babies may experience a low-grade fever during this time. In addition, various illnesses, including infections, can also cause fever or lower body temperature. Fever is a common immune response when the body is fighting an infection (14).
6. What should I do if my baby has a low temperature?
If you think your baby has a low body temperature, take their accurate temperature using a thermometer. If they show signs of hypothermia, immediately seek medical care. Meanwhile, keep your baby warm with blankets and provide skin-to-skin contact while closely monitoring their body temperature.
Low temperature in babies needs to be taken care of immediately. Babies may suffer from hypothermia due to different reasons such as infections, certain deficiencies, or preterm birth. The condition can be effectively managed if treated immediately with appropriate care. Therefore, as parents, you should be aware and mindful of the symptoms. However, if there seems to be no comorbidity,iThe presence of multiple chronic health conditions in a single individual, often complicating treatment and management low temperature in babies can be prevented. Further, ensuring you take the necessary after-birth hospital and at-home care measures, such as swaddling, can help prevent the condition.
Infographic: Interventions To Preclude Hypothermia In Newborns
Newborns are more likely to develop hypothermia due to their inability to regulate or maintain their body temperature. If not handled right, hypothermia can result in serious neonatal complications. Check out the infographic below to learn about precautions to protect the newborn from low body temperature (hypothermia).
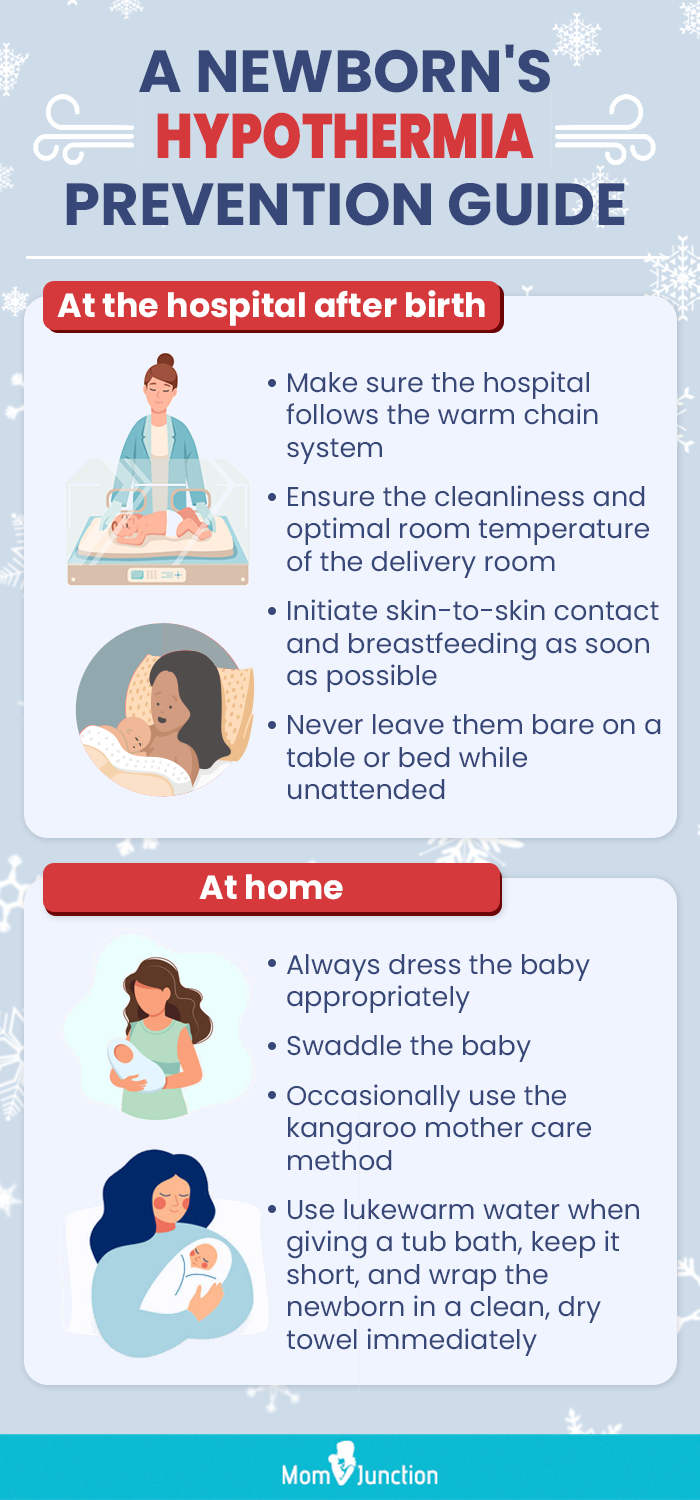
Illustration: Momjunction Design Team
Illustration: Baby Low Temperature: Causes Treatment And When To Worry

Image: Stable Diffusion/MomJunction Design Team
References
1. Thermal control of the newborn: A Practical Guide; World Health Organization
2. Fever and temperature taking; Caring for Kids
3. Madhu Manani, et al.; Elimination of Admission Hypothermia in Preterm Very low-birth-weight Infants by Standardization of Delivery Room Management; The Permanente Journal (2013).
4. V Kumar, et al.; Neonatal hypothermia in low resource settings: a review; Journal of Perinatology (2009).
5. Kajal Gandhi; Approach to hypoglycemia in infants and children; The Translational Pediatrics (2017).
6. Lawrence C. Ku, et al.; Bacterial Meningitis in the Infant; HHS Manuscript (2015).
7. Sepsis in Newborns; Cleveland Clinic
8. Tulay Ayyildiz, et al.; The Effects of Two Bathing Methods on the Time of Separation of Umbilical Cord in Term Babies in Turkey; Iranian Red Crescent Medical Journal (2015).
9. Hypothermia; Better Health Channel.
10. Caring for a newborn; WHO
11. Surface Body Temperature of Full-Term Healthy Newborns Immediately after Birth—Pilot Study; National Library of Medicine (2019).
12. Dillman, E et al.; Hypothermia in iron deficiency due to altered triiodothyronine metabolism; National Library of Medicine (2019).
13. Hasbaoui, Brahim El et al.;.Vitamin B12 deficiency: case report and review of literature; National Library of Medicine (2021).
14. Fever in children: Overview; National Library of Medicine (2013).
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Richard Mario Lurshay
- Dr. Andrea Wadley is the owner and head pediatrician at 127 Pediatrics, a home visit-only direct primary care pediatric and lactation practice based in the Dallas/Fort Worth area of Texas. She graduated with a medical degree in 2007 from the University of Texas Health Science Center in San Antonio and did his residency at the same university.
 Dr. Andrea Wadley is the owner and head pediatrician at 127 Pediatrics, a home visit-only direct primary care pediatric and lactation practice based in the Dallas/Fort Worth area of Texas. She graduated with a medical degree in 2007 from the University of Texas Health Science Center in San Antonio and did his residency at the same university.
Dr. Andrea Wadley is the owner and head pediatrician at 127 Pediatrics, a home visit-only direct primary care pediatric and lactation practice based in the Dallas/Fort Worth area of Texas. She graduated with a medical degree in 2007 from the University of Texas Health Science Center in San Antonio and did his residency at the same university.
Read full bio of Rohit Garoo
Read full bio of Dr. Ritika Shah
Read full bio of Vidya Tadapatri