Image: ShutterStock
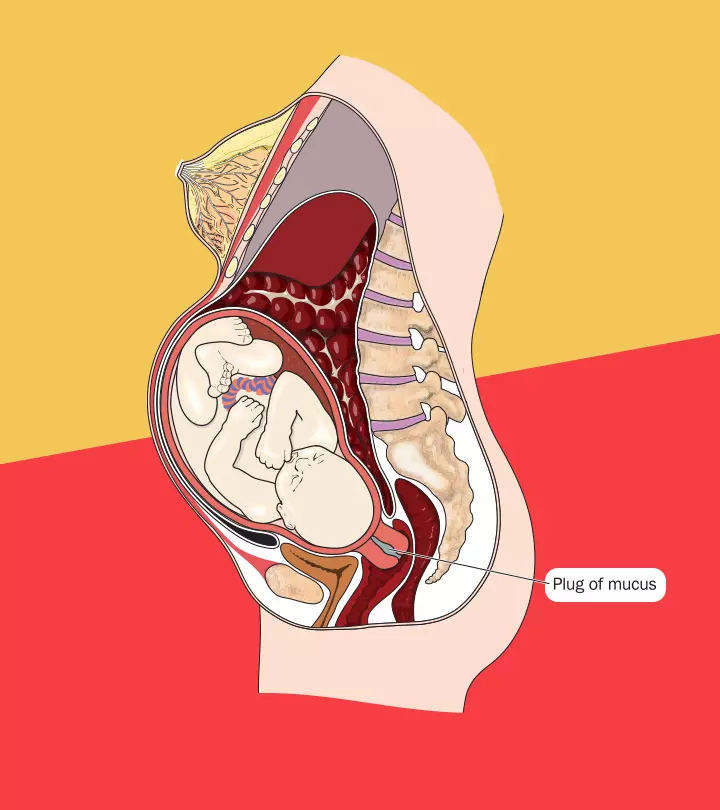
Marfan syndrome is a genetic disorder. Even though it is a congenital disorder, diagnosing Marfan syndrome in babies at birth or during infancy is not always possible. The symptoms of the disease may become more pronounced with age. Marfan syndrome is a disorder that affects the connective tissue throughout the body. According to The Marfan Foundation, about one in 5000 people are affected by this condition. Connective tissue plays an important role in providing strength and the necessary flexibility of the skin, bones, joints, muscles, and organs such as eyes, blood vessels, and heart valves.

Recognizing the early signs of Marfan syndrome is important for timely diagnosis and treatment, especially in babies, as symptoms may not show up right away. Read on to know more about the symptoms, causes, complications, and management of Marfan syndrome in newborns (1).
Key Pointers
- Marfan syndrome is a chromosomal disorder that affects connective tissue throughout the body.
- The skeletal, cardiovascular, and ophthalmic systems are most impacted by this condition.
- Factors such as a genetic history of Marfan syndrome and genetic mutations increase the likelihood of the condition.
- Symptoms of Marfan syndrome in babies include an elongated face, slanting eyes, a tall and thin body, loose skin, curved spine, and protruded chest.
- Among the potential complications of the syndrome are cardiomyopathy, heart failure, scoliosis, and glaucoma.
- Parents should consult a doctor if the baby displays signs such as cold or pale skin, trouble breathing, fever, or an irregular pulse.
What Are The Causes Of Marfan Syndrome?
Marfan syndrome is a spectrum of disorder caused by a heritable genetic defect in connective tissue that has autosomal dominant mode of transmissioniThe offspring gets the genetic condition even when the abnormal gene is passed from only one parent. (2).
- A genetic mutation in the FBN1 gene (on chromosome 15) is the main reason for the occurrence of Marfan syndrome. FBN1 gene is responsible for the formation of a protein called fibrillin1 which combines with another fibrillin1 and makes a filament, which is called microfibrils, a connective tissue.
- Microfibrils provide elasticity to the skin, ligaments, and blood vessels. It also provides strength to bones and to other tissues that support nerves, muscles, and lenses of the eyes.
- The poor formation of microfibrils eventually leads to the development of Marfan syndrome.
Symptoms Of Marfan Syndrome In Babies
The Marfan syndrome classically affects the skeletal, cardiovascular, and ocular systems of the body (3). However, some studies report effects on the pulmonary system and the skin as well.
The following are the symptoms that affect one or more of the systems mentioned above (4) (5).
- Elongated face (dolicocephalic facies)
- Deep-set and lower slanting eyes
- Crumpled ears
- Poor feeding
- Tall stature and thin build
- Long hands, legs, fingers, and toes or arachnodactyly (6)

- Loose and redundant skin with stretch marks
- Poor healing of lesions on the skin
- Curved spine
- Flat feet
- Protrusion of the chest known as Pectus Carinatum or a concave or sunken appearance of the chest known as Pectus Excavatum
- Laxity or joint hypermobility
- A reduced ratio of the upper body to the lower body
A combination of these symptoms might indicate Marfan syndrome.
 Be watchful
Be watchfulWhen To Call The Doctor?
The symptoms of Marfan syndrome may not always be evident during infancy.
See a doctor if you observe any of the following changes in the baby’s health:
- Breathlessness
- Cold or pale skin
- Sudden blue discoloration of the lips, nails, skin, etc.
- Shallow breathing
- Confusion
- Loss of consciousness
- Baby not exhibiting any movement
 Caution
CautionFactors That Increase The Risk Of Marfan Syndrome
The risk of the baby having Marfan syndrome increases if he or she has a parent with the disorder. The following are the risk factors for Marfan disease.
- It is an inherited autosomal dominant condition, which means an abnormal gene from any one parent can cause Marfan syndrome in the baby (7).
- There is a 50% risk of a baby being born with Marfan syndrome in each pregnancy, even if one of the parents has Marfan syndrome. (8)
- Three out of four cases of Marfan syndrome are due to the gene inheritance from the parent (4).
- In some cases, the condition is caused due to (new) gene mutation in the affected baby.
- Gene mutation is the reason for one out of four Marfan syndrome cases (4).
What Are The Complications Of Marfan Syndrome?
The progression of the disease could lead to the following complications. These complications may not be seen immediately in the babies but may surface as they grow.
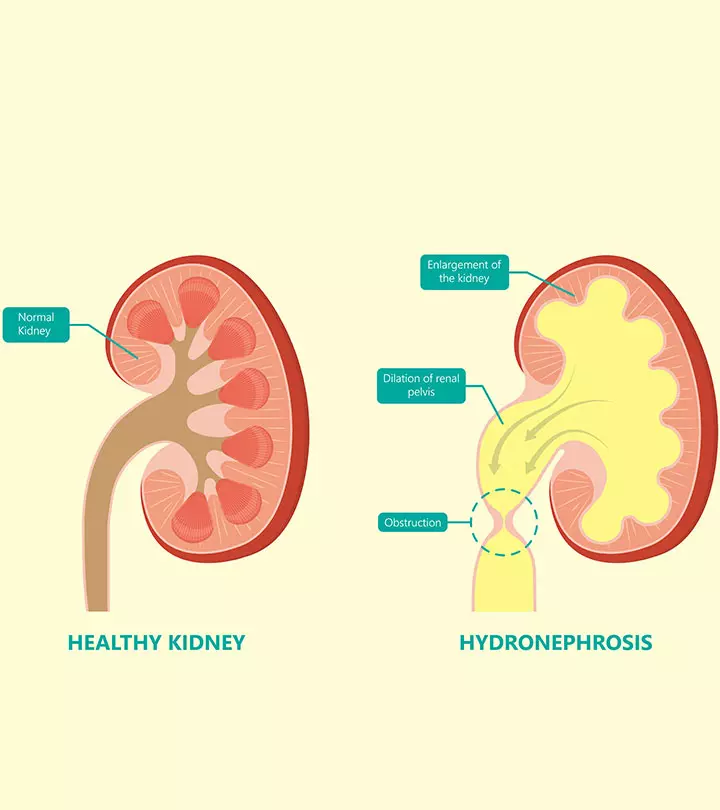
Cardiac complications

- Aorta is a major blood vessel in the human body originating in the heart. Aortic dilation, a severe complication happens due to an aortic aneurysm (an abnormal bulge in the aorta) (8).
- Dilation or loosening of the walls of the aorta leads to the improper blood supply in the baby’s body. The aorta might even tear in severe cases, thus resulting in aortic dissection, which might be life-threatening (9).
- Mitral valve prolapse is a condition in which the mitral valveiThe valve present between the heart’s upper-left and lower-left chambers. located on the left side of the heart does not open and close properly. It leads to backflow or leakage of the blood into the heart. It may cause breathlessness and irregular heartbeat in the baby (10).
- Cardiomyopathy is a heart muscle disease where the muscles of the heart are not healthy enough to pump blood to the body (11).
- Heart failure is a condition where the heart can’t pump or fill enough blood to meet the body’s needs (12).
Skeletal complications
- Congenital hip joint dislocation is commonly seen in Marfan syndrome (13).
- The vertebral column is significantly affected in Marfan syndrome, causing a curve in the spinal cord known as scoliosis (13).
- Inequality in the length of limbs is also seen (13).
- Improper development of ribs due to Marfan causes pectus carinatum or pectus excavatum.
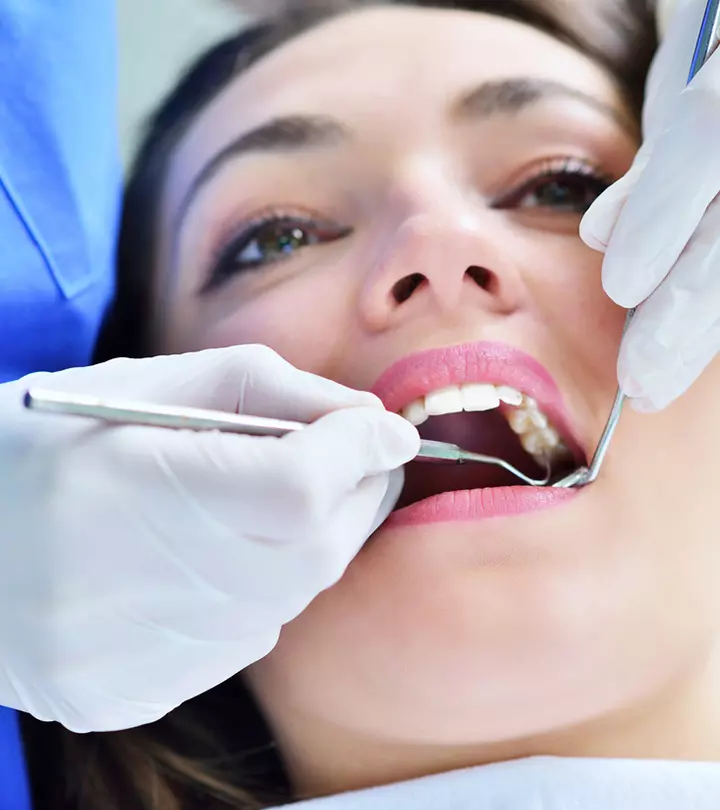
Ocular complications
- Myopia or nearsightedness is a common finding. It develops in childhood and worsens with age (5).
- Ectopia lentis or lens dislocation from the center of the eyeball is seen in about 60% of cases. It may occur at birth or develop in a later part of life. . (5)
- Early cataractiA condition in which the eye’s lens becomes cloudy, leading to diminished vision. and early glaucomaiA group of conditions that damage the optic nerve and cause vision loss due to fluid build-up in the front part of the eye. are some other findings (14).
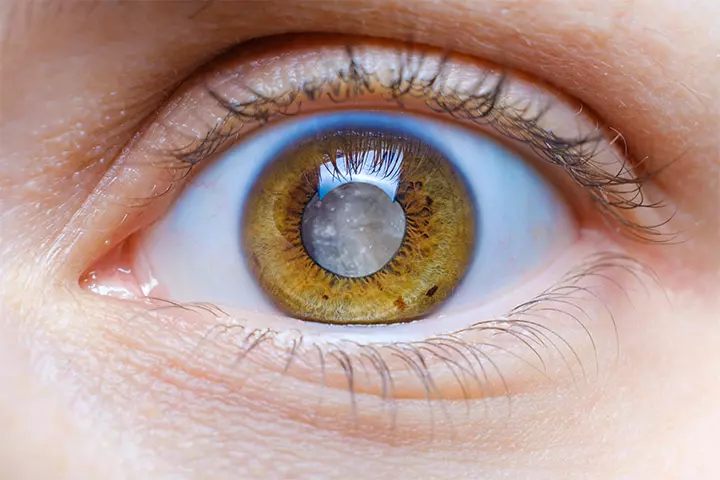
- Retinal detachment (severe complication) is a condition in which the light-sensitive membrane in the back of the eye gets separated from its supporting layers. (15)
- Pulmonary conditions like emphysema (breathlessness due to damaged air sacs in the lungs), bullae (enlarged air sacs in lungs), pneumothorax (collapsed lung), etc., might also occur in Marfan syndrome. Pulmonary involvement occurs much less frequently. (3)
Other complications
- The enlargement of the membrane that surrounds the brain and spinal column along with the occasional presence of cysts is known as dural ectasia. Dural Ectasia is present in more than 60 percent of people who have Marfan syndrome (16).
- A limited group study demonstrated that Marfan syndrome might be linked to a high prevalence of obstructive sleep apnea (17).
When symptoms of Marfan syndrome are present at the time of birth, then the condition is known as neonatal Marfan syndrome. It is the most severe type of Marfan syndrome, and has a poor prognosis.
Neonatal Marfan syndrome is different from Marfan syndrome. The difference lies in the early-onset and visible characteristics at the time of birth. There is also a rapid progression of symptoms with heart, airways, and the lungs being the most affected (18).
How Is Marfan Syndrome Diagnosed?
Marfan syndrome may be suspected on antenatal ultrasound, but the diagnosis is often not made until late childhood or in adulthood (19). The doctor will begin the diagnostic procedure with a proper physical examination and enquiring thoroughly about the baby’s family history.
The major diagnostic tests are (4):
- Electrocardiogram (ECG) records the electrical activity of the heart. It helps in knowing about irregular heartbeats and muscle damage.
- Echocardiography (echo) is the ultrasound of the heart. It helps in capturing live and moving images of the heart.
- A complete eye examination is done by an instrument called a slit lamp. It is used to examine the entire interior part of the eye.
- X-rays help determine the structure of the bones and detect the presence of anomalies.

- Computerized tomography or magnetic resonance imaging (CT or MRI scans) might be needed to check for any abnormalities in the joints and multiple organs.
- Molecular genetic testing through a blood sample might be conducted to determine the presence of a faulty FBN1 gene.
As the baby grows in age, the symptoms become pronounced and might make the diagnosis easier.
Treatment Of Marfan Syndrome
Marfan syndrome is a genetic disease, and it is not possible to reverse the genetic mutation. While there is no treatment, there are several ways to manage the condition (4).
1. Cardiac issues
- For cardiac issues, you will need to consult a pediatric cardiologist.
- The doctor might suggest some medicines like beta-blockersiDrugs that control heart rate and blood pressure by blocking the action of the adrenaline hormone. to support the heart. The dosage will be decided according to the baby’s age, tolerance to medicines, and other factors.
- In severe cases, planned or emergency surgery might be needed to repair the dissected aorta or heart valves, and rarely, the child might need a heart transplant.
2. Skeletal issues
- For issues related to the baby’s bones, you might need to consult a pediatric orthopedist.
- The doctor might suggest brace, physical therapy, or surgery in some severe cases.
3. Ophthalmic issues
- For eye-related issues, an ophthalmologist may suggest either medicine or surgery.
- Prescription glasses can help rectify vision problems.
Any treatment protocol is decided by the doctor depending on various factors like age, weight, severity of symptoms, and gauging the prognosis of the intervention.
Regular follow-ups with a multidisciplinary team, including pediatric eye and heart specialists, orthopedic doctors, and genetic counselors, can help monitor and manage all aspects of the child’s health.
Home Care For Babies With Marfan Syndrome
Home care includes lifestyle modifications and maintaining a thorough health check-up routine.
- Regular electrocardiograms or electrocardiographs should be done at the frequency and duration suggested by the doctor.
- Regular eye check-ups help keep a watch on any change in vision.

- Routine visits to the orthopedic doctor and the physical therapist are recommended to help monitor any changes in the bones.
- Lifestyle changes are more relevant when the baby steps into toddlerhood and becomes more active. A pediatrician can suggest the changes based on the extent of symptoms and other limitations of the child.
- It is also crucial to provide emotional support and positive encouragement to babies as MFS could be associated with mental health disorders such as depression, anxiety, and social isolation (20).
Frequently Asked Questions
1. Does Marfan syndrome get worse with age?
Marfan syndrome and its related symptoms are progressive. The symptoms vary from person to person, and the progression is often not easy to predict. Nevertheless, regular monitoring, medications, surgical interventions, and necessary precautions allow people with the condition to live a long life (21).
2. Does Marfan syndrome affect intelligence?
Marfan syndrome, by itself, does not have any direct effect on intelligence (22).
3. What is the life expectancy of a child with Marfan syndrome?
The life expectancy of a person with Marfan syndrome is about 70 years which is comparable to the general population (24).
4. How tall is the average person with Marfan syndrome?
A study shows that men with Marfan syndrome may reach an average of 6.2 feet and women 5.7 feet. These measurements may vary widely based on many factors (25).
5. Can kids with Marfan’s play sports?
Kids with Marfan’s syndrome may need to avoid contact and high impact sports such as football, basketball, gymnastics, baseball, weightlifting, and volleyball as they may stress the heart and lungs and have the potential risk of a blow to the chest. However, they may pursue non-competitive activities such as bike riding, swimming, and dancing (23).
Marfan syndrome, one of the inherited genetic disorders in children, affects the baby’s connective tissues. Its signs and symptoms may not always be present at birth or infancy. Instead, the condition becomes more pronounced as the child grows older. There is currently no cure for Marfan syndrome, and the treatment focuses on symptom management and decreasing the risk of complications. Regular visits to a physical therapist, an ophthalmologist, and an orthopedic doctor can help keep track of the condition and enable babies with Marfan syndrome to live a regular life as far as possible.
Infographic: How Is Marfan Syndrome Diagnosed?
Marfan syndrome is a genetic disorder, detectable on an antenatal scan; however, it may go undiagnosed until childhood. Here is an infographic detailing the diagnostic tests that could be suggested by a doctor when they suspect your baby has Marfan syndrome.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Illustration: Marfan Syndrome In Babies: Symptoms Risks And Treatment

Image: Stable Diffusion/MomJunction Design Team
Seeking answers about potential causes of your child’s Marfan syndrome? Enlighten yourself through this video, unraveling the complexities of origins and available treatments.
References
1. Jessica Warnink-Kavelaars et al.; Marfan syndrome in childhood: parents’ perspectives of the impact on daily functioning of children, parents and family; a qualitative study; Journal of BMC Pediatrics
2. FBN1 gene; US National Library of Medicine
3. Weiming Hao et al.; Marfan syndrome with pneumothorax: case report and review of literatures; Journal of Thoracic Diseases
4. Marfan Syndrome in Children; University of Rochester Medical Center
5. Marfan Syndrome; National Organization for Rare Disorders.
6. Arachnodactyly; National Library of Medicine
7. Gwenaelle Collod-Beroud, and Catherine Boileau; Marfan syndrome in the third Millennium; U.S. National Library of Medicine.
8. Pediatric Marfan Syndrome; Children’s National Organization
9. Hung‐Hsuan Wang et al.; Does altered aortic flow in marfan syndrome relate to aortic root dilatation?; Journal of Magnetic Resonance Imaging
10. Problem: Mitral Valve Prolapse; American Heart Association
11. Roland Hetzer et al.; Cardiomyopathy in Marfan syndrome; European Journal of Cardio-thoracic Journal
12. Arthur E. Weyman and Marielle Scherrer-Crosbie; Marfan syndrome and mitral valve prolapse; The Journal of Clinical Investigation
13. Ali Al Kaissi et al.; Musculo-Skeletal Abnormalities in Patients with Marfan Syndrome; U.S. National Library of Medicine
14. MARFAN SYNDROME; March of Dimes
15. EYE EMERGENCIES; The Marfan Foundation
16. NERVOUS SYSTEM; The Marfan Foundation
17. Sleep apnea in Marfan’s syndrome. Increased upper airway collapsibility during sleep; National Library of Medicine
18. WHAT IS NEONATAL MARFAN SYNDROME?; The Marfan Foundation
19. Alan Graham Stuart and Andrew Williams, Marfan’s syndrome and the heart; U.S. National Library of Medicine
20. A Review of Psychosocial Factors of Marfan Syndrome: Adolescents, Adults, Families, and Providers; National Library of Medicine
21. Aging with Marfan Syndrome: 5 Common Questions; The Marfan Foundation
22. WHAT IS MARFAN SYNDROME?; The Marfan Foundation
23. Marfan Syndrome; Nemours Kids Health
24. Marfan syndrome; Better Health Channel
25. Gurkan Erkula et al.;Growth and maturation in Marfan syndrome; NCBI
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Surabhi Gupta
Read full bio of Dr. Ritika Shah
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny