Image: Shutterstock
You may be tempted to pop a pill for your headache, body ache, or nausea commonly experienced during pregnancy but ensure the drug’s safety before you do so. As it is not always possible to know which medications to avoid during pregnancy, it is wise to ask your doctor before taking any medicine during pregnancy to ensure the right prenatal care. Some medications may cross the placenta and reach the developing baby. It may lead to serious adverse effects such as congenital anomalies and other pregnancy complications. This post tells you about certain drugs that may harm your maternal health and fetal development. In addition, it helps you to understand which drugs to avoid and why fetal exposure to certain medications can be harmful.
Key Pointers
- Vitamin A derivatives used for acne treatment are classified as Category X by the FDA, and should be avoided during pregnancy due to an increased risk of congenital disabilities.
- Oral tetracyclines, such as doxycycline, should not be used during pregnancy as they may cause permanent tooth discoloration in the infant.
- Antihistamines are not classified under pregnancy Category A, and their safety should be reviewed with a doctor before taking.
- Benzodiazepines, including Valium and Ativan, may cause infant withdrawal symptoms and floppy infant syndrome, but can be taken during pregnancy with caution.
- Consult a doctor before taking any medication during pregnancy, as certain medications may cross the placenta and harm the developing fetus.
Why Medication Safety Is Important
Medication safety is particularly critical during pregnancy due to the potential risks to fetal development. Pregnant women must be aware of the medications that can adversely affect both maternal and fetal health, ensuring they make informed choices.
Medications To Avoid During Pregnancy
The following is the list of groups and individual drugs you should avoid as they could have an impact on fetal development. Most of the studies are inconclusive and need further research to confirm the adverse effects of the drugs on the fetus. However, you should never take these drugs without your doctor’s prescription.
1. Acne medications
Vitamin A derivatives, such as isotretinoin (Accutane), used to treat severe acne, increase the risk of birth defects, cardiac and brain defects, physical abnormalities, and other adverse neonatal outcomes.
The US Food and Drug Administration (FDA) has classified this drug under category X, which means there is positive evidence of fetal risk (1).
Oral tetracyclines such as doxycycline (Doryx) used to treat acne, and bacterial infections can cause permanent discoloration of teeth of the baby (2). The American College of Obstetricians and Gynecologists advises against the use of these two drugs during pregnancy because of its potential risks (3).
 Point to consider
Point to consider2. Antifungal medications
Antifungal medications (4), such as fluconazole (Diflucan), are typically used as prescription drugs for oral thrush and vaginal fungal infections (5). According to the FDA, the long-term use of high-dose (400-800 mg/day) fluconazole during the first trimester may result in ‘abnormal-looking’ face, oral cleft, bowing thigh bones, thin ribs, long bones, and congenital heart diseases in the infant (6). However, this risk was not found to be associated with a single dose of fluconazole 150mg to treat vaginal yeast infection (candidiasis).
There are no well-controlled studies of Diflucan in pregnant women, so if you are pregnant or planning to, and need to take Diflucan, then inform your doctor about your pregnancy.
3. Antihistamines
These are taken for nasal congestion, hives, rash, and other allergic symptoms. While there are no studies to prove any definite teratogenic effects (effects on the fetus), antihistamines are not categorized under Pregnancy Category A (safe to take during pregnancy) (7). Therefore, you need to discuss the safety of the drugs with your doctor.
The American College of Obstetricians and Gynecologists (ACOG) and The American College of Allergy, Asthma and Immunology (ACAAI) recommend chlorpheniramine and tripelennamine as safe options during pregnancy. They also recommend cetirizine and loratadine after the first trimester, for patients who cannot tolerate high doses of chlorpheniramine and tripelennamine (7). However, the safety of antihistamines is still under question because of the limited human studies.
As most of the antihistamines are available as over-the-counter drugs for motion sickness, and allergies, it is best to consult your doctor before taking them during pregnancy.
4. Benzodiazepines
Clonazepam (Klonopin), alprazolam (Xanax), lorazepam (Ativan), and diazepam (Valium), belonging to the class of benzodiazepines, help treat anxiety, panic attacks, insomnia, and seizures.
As per the American College of Obstetricians and Gynecologists (ACOG) guidelines on the use of psychiatric medications during pregnancy and lactation, benzodiazepines are not considered to be harmful teratogens, as they do not pose a serious teratogenic risk (effects on the growth of the fetus) (8). However, the guidelines also mention about the possible risks such as 0.01% increase in the risk of oral cleft associated with diazepam (Valium), and floppy infant syndrome (hypothermia, lethargy, poor respiratory effort, and feeding difficulties) if benzodiazepines are taken during labor. Also, the infant is likely to have withdrawal symptoms for several months if the mother took alprazolam, chlordiazepoxide (Librium), or diazepam during pregnancy.
The FDA has categorized benzodiazepines under Pregnancy Category D, which means that there is a potential risk to the fetus but the drug may be used if the potential benefits outweigh the possible risks.
5. Chloramphenicol
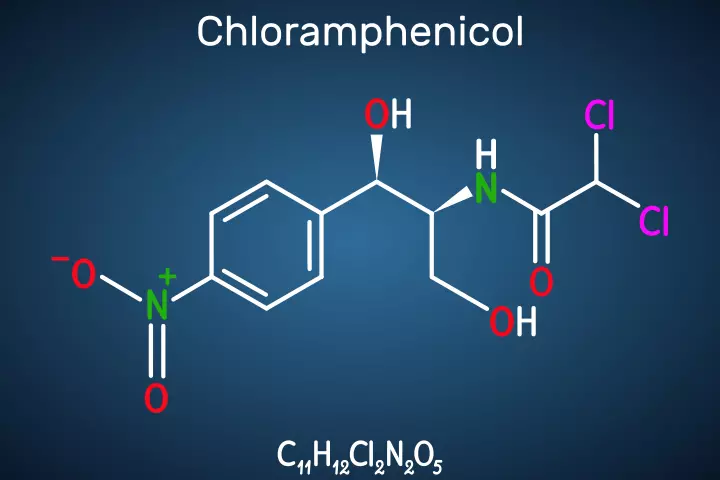
The antibiotic may not have any adverse effects on the fetus when taken during pregnancy.
A Hungarian population-based study states that the use of chloramphenicol in therapeutic doses during the early stages of pregnancy pose little risk to the developing fetus (9). Also, a Danish nationwide cohort study concluded that administering chloramphenicol eye drops or eye ointments during the first trimester was not associated with any major congenital malformations (10).
The first issue of Clinical Infectious Disease states that there is clinical data that chloramphenicol, when administered during delivery, crosses the placenta and causes grey baby syndrome in the baby (11), and hence be avoided during labor.
6. Codeine
The opioid medication is used for pain and cough. A Scientific Impact Paper by The Royal College of Obstetricians and Gynaecologists (RCOG) states that opioids could be taken during all stages of pregnancy. However, they have to be taken in the lowest dose for the shortest possible time (12). The Centers for Disease Control and Prevention highlights that approximately 7% of pregnant women self-reported using prescription opioid pain medications .
A Michigan Medicaid study also reported that there was no increased risk of abnormal congenital disabilities in pregnant women exposed to codeine in the first trimester (13). But neonatal withdrawal symptoms are observed in the newborns (in non-addicted mothers) even when therapeutic doses of codeine were taken during the last trimester.
7. Coumadin (warfarin)
The blood-thinning medication is prescribed to treat and prevent clots in the heart, veins, arteries, and lungs. Its intake during the first trimester could lead to a rare condition called fetal warfarin syndrome (14) and is also associated with spontaneous abortions. There could be a risk of central nervous system abnormalities if warfarin is taken at any stage in the pregnancy. For mothers who need to be on long-term warfarin therapy, experts recommend heparin as a substitute (15). Warfarin must be avoided during pregnancy; if you are using this medication, and planning to get pregnant, then talk to your doctor.
8. Fluoroquinolones

These are another class of antibiotics. The use of fluoroquinolones during early pregnancy was found to have been associated with an increased risk of miscarriage (16). While there are no controlled studies on the effects of fluoroquinolone (Ciprofloxacin) on pregnant women, animal studies showed adverse effects such as permanent cartilage erosion in weight-bearing joints, and cystic fibrosis (17).
9. NSAIDs
Non-steroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen (Advil), diclofenac(Voltaren), naproxen (Naprelan), and piroxicam (Feldene) are prescribed as pain relief options. According to the Scientific Impact Paper by the Royal College of Obstetricians, NSAIDS should be avoided during pregnancy unless prescribed by the physician. They should be avoided during the early embryonic development or first trimester and after 30 weeks of gestation (18).
The use of NSAIDs during pregnancy is found to result in low birth weight in the baby, but the low weight could be attributable to the underlying inflammatory condition than the drug itself. There is a borderline risk with these drugs, so it is good to avoid them during pregnancy (19).
10. Primaquine
The antimalarial drug treats malaria caused by Plasmodium virax parasite. Although there are no human studies, there is likely to be a risk of fetal anemia if you have G6PD deficiency (20).
 Things to know
Things to know11. Sulfonamides
Also referred to as sulfa drugs, they are another group of antibiotics that treat bacterial infections. A population-based case-control study concluded that using Cotrimoxazole (sulfonamide) during pregnancy may increase the risk of cardiovascular malformations, and urinary tract abnormalities (21). The American College of Obstetricians and Gynecologists recommends doctors prescribe antibiotics after discussing the possible outcomes with the mother (22). The doctors prescribe antibiotics after discussing the possible outcomes with the mother. Taking antibiotics while pregnant warrants caution as some drugs can pass the placenta and affect the fetus.
12. Topiramate
The anti-epileptic drug is used to treat migraine headaches and other psychiatric illnesses. According to the US FDA, usage during the first trimester could increase the risk of cleft lip or cleft palate in newborns (22).
The FDA also states that oral clefts happen during the early stages of pregnancy (even before the woman knows she is pregnant) (23), so women of childbearing age should talk to physicians for safer options (when on topiramate) if they are planning to get pregnant. Also, you should not stop taking topiramate without talking to your healthcare professional as it can cause health problems to you and the baby.
13. Trimethoprim (Primsol)
The antibiotic is used to treat bladder infections. The Best Practice Journal’s ‘Managing urinary tract infections in pregnancy’ states that there are no controlled studies to support the use of trimethoprim during pregnancy. So, it is recommended to avoid this medication during the first trimester as it may increase the risk of neural tube defects (24). A study using the Danish fertility database found an association between the use of trimethoprim in the 12 weeks before conception and doubling of the rate of congenital malformations (25). However, further investigation is needed to confirm the chances of adverse effects. So, talk to your doctor if you are on such medications.
While some of these medicines are a clear no during pregnancy, some may be given by the doctor if they think the benefits outweigh the risks.
You need to be extra careful while taking over-the-counter medications as they can be purchased without a prescription. Certain OTC drugs to avoid are Aspirin, bismuth subsalicylate, ibuprofen, and Naproxen.
Medications need not always be the first line of treatment in the case of minor disturbances such as a headache, nausea, joint pains, and constipation during pregnancy.
Things To Consider Before You Consume OTC Medications
Here are a few things to consider before going for a pill, especially when you are pregnant.
- Try natural measures: Most of the physical illnesses you experience during pregnancy may be reduced with natural remedies. For example, you can meditate to get relief from stress or have a massage done for body aches. You may consume a hot soup for cold or take enough rest for a fever.

 Point to consider
Point to consider- Check with your doctor: Before taking any medication, you must seek advice from your doctor to ensure safe antenatal care during pregnancy. They may suggest the lowest possible dose depending on your condition.
- Do not take combination drugs: Do not mix two different medications, and take them together. You can only do that on your doctor’s prescription.
- Read the label: While most of the components of the OTC medicines are not harmful, it is good to know about them by reading the label.
Frequently Asked Questions
1. Are there any alternative treatments that can be used instead of medication during pregnancy?
Pregnant women may try alternative treatments such as relaxation techniques, self-hypnosis, patterned breathing (Lamaze), acupressure/acupuncture, aromatherapy, massage, and visiting a chiropractor specialized in treating pregnancy-related issues. However, ensure that all methods are practiced under expert guidance (29).
Bryony, a mother and vlogger, had severe depression during pregnancy. Sharing how she managed her antenatal depression without medicines, she says, “On the 13th week of my pregnancy, I started my CBT (cognitive behavioral therapy) pregnancy course that was a six-week course and turned out to be good for me… I needed more one-to-one therapy and intervention at this point, and I was fortunate because the therapist who was running this group said that she’d do a one-to-one session with me. During that session, we went through everything I had been experiencing, and she (the therapist) realized that I needed more one-to-one sessions (i).” CBT and one-on-one sessions didn’t entirely treat Bryon’s depressive symptoms, but they helped her manage the condition and feel better without taking any antidepressants.
2. How do changing hormone levels during pregnancy affect the way the body processes medication?
Drug metabolism may be altered due to the increased levels of sex hormones and thyroid hormones during pregnancy. Increased progesterone in pregnant women and the pressure from the expanding uterus slows the movement of the stomach and intestinal contents affecting the absorption of drugs (30).
3. How do healthcare providers determine if a medication is safe to use during pregnancy?
Healthcare providers review the latest safety information on medications provided by government organizations such as CDC before determining if a medication is safe during pregnancy (32). The safety of some medicines also depends on the pregnant woman’s gestational age and medical history.
4. What should pregnant women do if they need to take medication for a condition?
Pregnant women should avoid self-medicating with over-the-counter medications under all circumstances. They should consult a physician if they need medication for a particular condition.
Some medicines can have adverse effects on you or the developing fetus if consumed during pregnancy. There is a lot of misinformation about the safety and risks of these medicines on the internet. You should consult your doctor before consuming any medication during pregnancy. This list of medications to be avoided during pregnancy will help you understand the strict contraindications. However, your doctor may prescribe one of these medicines for specific health conditions. They will weigh risks versus benefits before prescribing a drug. Do not hesitate to ask your doctor if you have any doubts or apprehensions.
Infographic: What Are The Medications To Avoid During Pregnancy?
Pregnancy brings a lot of new discomforts and aches, which could make you think about popping a pill to feel better. But, not all medications are safe for pregnant women, and some may carry the risk of complications and adverse effects for the mother and the fetus. Therefore, note the medicines in the infographic below and avoid consuming them without a prescription.
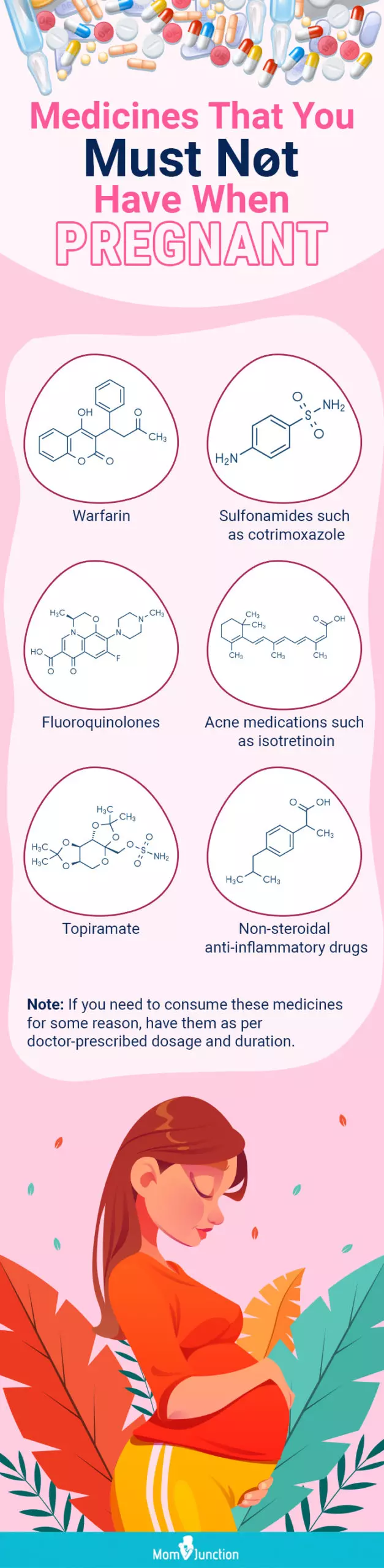
Illustration: Momjunction Design Team
Illustration: Medications To Avoid During Pregnancy

Image: Stable Diffusion/MomJunction Design Team
Alleviate pregnancy-related stress by learning safe medication practices. This educational video equips you with essential information, offering peace of mind during this significant phase of life.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. My (unexpected) mental health struggles in pregnancy | Antenatal depression; and anxietyhttps://www.youtube.com/watch?feature=shared&v=1_WMlnyan34
References
1. Prescribing information – Accutane; US Food and Drug Administration
2. Highlights of prescribing information – Doryx; US Food and Drug Administration
3. Skin conditions during pregnancy; The American College of Obstetricians and Gynecologists (2018)
4. Benoît Pilmis et al.; Antifungal drugs during pregnancy: An updated review;Journal of Antimicrobial Chemotherapy, Volume 70 (2015)
5. Prescribing information – Diflucan; US Food and Drug Administration
6. FDA Drug Safety Communication; FDA; US Food and Drug Administration
7. Sumit Kar et al.; A review of antihistamines used during pregnancy; J Pharmacol Pharmacother (2012)
8. Carrie Armstrong; ACOG guidelines on psychiatric medications use during pregnancy and lactation; American Academy of Family Physicians
9. Andrew E. Czeizel, Magda Rockenbauer, Henrik T. Sorensen, Jorn Olsen; A population-based case–control teratologic study of oral chloramphenicol treatment during pregnancy; Spingerlink
10. Thomseth V et.al.; Exposure to topical chloramphenicol during pregnancy and the risk of congenital malformations: A Danish nationwide cohort study; NCBI (2015)
11. Marvin S. Amstey; Chloramphenicol therapy in pregnancy ; Clinical Infectious Diseases; Oxford Academic
12. Antenatal and postnatal analgesic (Scientific Impact Paper No. 59); Royal College of Obstetricians & Gynecologists
13. Malaika Babb, Pharm D, Gideon Karen, M.D FRCPC FACMT, and Adrienne Einarson, RN; Treating pain during pregnancy; NCBI (2010)
14. Hou JW; Fetal warfarin syndrome; Chang Gung Med J (2004)
15. Asnat Walfish, M.D, Gideon Koren, MD, FRCPC; The “Warfarin Window” in pregnancy: The importance of half-life; Journal of Obstetrics and Gynaecology Canada
16. Flory T. Muanda, Odile Sheehy, and Anick Berard; Use of antibiotics during pregnancy and risk of spontaneous abortion; Canadian Medical Association Journal
17. Ciprofloxacin use by pregnant and lactating women; US Food and Drug Administration
18. RCOG review on pain relief options for women during pregnancy and breastfeeding ; Primary Care Women’s Health Forum
19. K Nezvalova-Henriksen, Ospigset, and H Nordeng; Effects of ibuprofen, diclofenac, naproxen, and piroxicam on the course of pregnancy and pregnancy outcome: a prospective cohort study; NCBI (2013)
20. Primaquine; NIH (2006)
21. Czeizel AE, Rockenbauer M, Sorensen HT, Olsen J; The teratogenic risk of trimethoprim-sulfonamides: a population based case-control study; NCBI (2001)
22. Use of Topiramate in pregnancy and risk of oral clefts; Centers for Disease Control and Prevention
23. FDA drug safety communication: Risk of oral clefts in children born to mothers taking Topamax (topiramate); US Food and Drug Administration
24. Managing urinary tract infections in pregnancy; Best Practice Advocacy Centre New Zealand
25. Jon Traerup Andersen, et. al.; Trimethoprim Use prior to pregnancy and the risk of congenital malformation: A register-based nationwide cohort study; Obstetrics and Gynecology International Volume 2013
26. Is Any Acne Treatment Safe To Use During Pregnancy?; American Academy of Dermatology Association
27. Chloroquine for prevention and treatment of malaria; UK Teratology Information Service
28. Medicines in pregnancy; NHS
29. Pregnancy: Using Alternative Therapies; Cleveland Clinic
30. Maged M. Costantine; Physiologic and pharmacokinetic changes in pregnancy; NCBI (2014)
31. Research on Medicines; CDC
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Shalini MA
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das