Image: ShutterStock
Migraine is a pounding pain felt on either side of the head. Some women experience migraines while breastfeeding too. However, the treatment for migraine may be different for lactating and non-lactating women although the symptoms remain the same.
Migraines can leave you disrupted for the entire day if not taken care of. Thankfully, certain over-the-counter and prescribed medications can help relieve its effects while nursing.
If you are a chronic migraine patient or suffer from migraine while breastfeeding, continue reading to learn how to cope with it. This post will tell you more about migraine in nursing women, including its causes, symptoms, treatments, and preventive measures.
Key Pointers
- Migraine headaches are characterized by a throbbing pain on either side of the head.
- Breastfeeding mothers may experience migraines due to stress, hormonal changes, sleep issues, or phonophobia.
- Lactating mothers with migraines may find relief through painkillers like ibuprofen and acetaminophen, or prescription medication such as sumatriptan.
- To ease migraine symptoms, it is important to get adequate rest, avoid triggers, and practice regular exercise.
What Is A Migraine?

Image: Shutterstock
Mothers who suffer from migraines, feel intense throbbing and pulsating sensation around the head region. The prolonged head pain can even persist for 2-3 days, and you may suffer from a high level of discomfort.
Symptoms Of Migraine In Lactating Mothers
Typically, the major symptom of a migraine is a throbbing headache. Some other symptoms that indicate the onset of a migraine include (1):
- Pain on one side or both sides of your head
- Irritability
- Neck stiffness

Image: Shutterstock
- Aura (Blurred vision)
- Nausea and vomiting
Nana Pieterson, a lactating mother, describes the symptoms she encounters during a migraine episode. She says, “I suffer from migraines; they come at a specific time. I started keeping a diary to monitor when it happens, and it seems to come just when I’m about to be on my period, after my period, or while I’m ovulating—before or after ovulation. I’m noticing a pattern, so I’m guessing it’s got something to do with the lady time. Yeah, I had a migraine earlier; My head was spinning, I felt nauseous, and I had colors in my eyes. The migraine made my arm numb and tingly, and I couldn’t feel my feet (i).”
It’s important to note that not everyone experiences the same set of symptoms. Migraine symptoms may vary significantly from person to person.
Causes Of Migraine In Lactating Mothers
Let’s look at some causes of migraine during breastfeeding.
- Hormonal Changes:
The American College of Obstetricians and Gynecologists states that women are affected more by migraine due to hormonal changes(2)
. Additionally, A CDC National Health Interview Survey revealed that women were about twice as likely as men to experience severe headaches or migraines, with rates (calculated over three months) being 20.1% for women and 10.6% for men. When you are breastfeeding, the body releases the hormone, Oxytocin. Oxytocin in the lactating mother’s body causes contraction of the milk ducts and triggers severe headaches. Oxytocin release triggers the condition of migraine headache in lactating moms.
 Quick fact
Quick fact- Sleep Deprivation:

Image: Shutterstock
A lactating mom often experiences sleep deprivation, during her early stages of post-pregnancy. The condition of sleep deprivation is prevalent and triggers migraine headaches.
- Stress:
Stress can trigger migraine headaches. Hence, it is important to ensure you have enough relaxation time by seeking support and care from your loved ones to help prevent excessive stress and reduce the likelihood of experiencing migraines.
- Phonophobia:
Individuals exposed to loud noises usually suffer from migraine headaches. As a new mom, you should avoid loud noises as they can lead to migraine pains.
- Less Medication Available:
You may use painkillers when breastfeeding or other migraine medications only after consulting your doctor. Painkillers such as acetaminophen or ibuprofen are usually considered safe but doctors may prescribe a daily limit that should not be exceeded by lactating women. With proper medical consultation, you can ask your doctor for a list of migraine medications, which are safe to consume during breastfeeding.
 Point to consider
Point to considerMedications To Cure Migraine In Lactating Mothers

Image: Shutterstock
If you are expecting or nursing and you suffer from migraine, you need to avoid certain medications that may affect your or your infant’s health:
- NSAIDS – non-steroidal anti-inflammatory drugs like Naproxen and Ibuprofen.
- Amitriptyline and Fluoxetine.
- Beta-blockers such as propranolol and nadolol.
- Narcotic drugs such as butorphanol, verapamil, and codeine.
- OTC Medications- Motrin, Tylenol, and other OTC medications are safe for lactating mothers.
The FDA approves the use of Botox (onabotulinumtoxinA) for treating migraine in adults, but you need to consult with your healthcare provider about its safety when you are lactating (4)
.
Medications To Avoid During Migraine In Lactating Mothers
If you are expecting and you suffer from migraine, you need to avoid medications like:
- Painkillers such as Aspirin
- Ergotamine
- Antihistamines
 Caution
CautionPreventing Migraine In Lactating Mothers
Here are some simple tips to prevent migraine during lactation:
- Exercise Regularly:

Image: Shutterstock
Excessive stress and an unbalanced lifestyle can trigger migraines in lactating moms. Light exercises like yoga or walking help release stress hormones from the body and prevent migraine headaches. They also help promote your overall health and wellness.
- Avoid Triggers:
Migraine often occurs due to loud music or food odor. Try to stay in a peaceful environment and avoid consuming spicy or caffeinated food products.
- Rest:
Sleep deprivation or disturbed sleep patterns can elevate the symptoms of migraines while breastfeeding, making it difficult for new mothers to embrace their motherhood journey. Therefore, it is advisable to take adequate rest during lactation. Effective migraine management can include taking short naps throughout the day and keeping your mind relaxed and stress-free.
You can easily deal with migraine by following a well-balanced diet.
Migraine during breastfeeding might disrupt your everyday lifestyle and increase discomfort. You may experience headaches while breastfeeding, accompanied by irritability, neck stiffness, blurred vision, etc. Migraines in nursing mothers may occur due to hormonal changes, sleep deprivation, or stress. The condition may be more discomforting because lactating women have lesser choices in medicines. If you are dealing with a migraine during breastfeeding, talk to your doctor. They may prescribe Ibuprofen, morphine, Tylenol, or other safe options for your baby. However, the best way to deal with migraines is by exercising regularly and resting enough.
Frequently Asked Questions
1. Are postpartum migraines common?
Yes. Postpartum migraines are a common occurrence. Around one in four women are likely to have migraines within two weeks after childbirth, and almost half of them experience migraine attacks in their first month of delivery (5).
2. When should I go to the hospital for a migraine?
If you are experiencing severe symptoms of migraine accompanied by neck stiffness, vision disturbances, and troubled speaking, you should visit the doctor immediately (6).
3. How long do postpartum migraines last?
Postpartum migraines usually go away within five to six weeks post-delivery.
4. Can migraines affect milk supply?
There are no studies that indicate postpartum migraines affect the breast milk supply.
Infographic: Migraine During Breastfeeding
The hormonal changes, irregular sleeping patterns, or stress could put nursing mothers at an increased risk of migraines. Following the doctor’s advice on medication, identifying the triggers, and engaging in relaxative practices could help reduce the frequency of migraines.
The infographic below is a handy list of potential migraine trigger foods. It also includes information on a few concerning signs that need medical attention. Illustration: Momjunction Design Team
Illustration: Causes of Migraine During Breastfeeding And Its Treatment
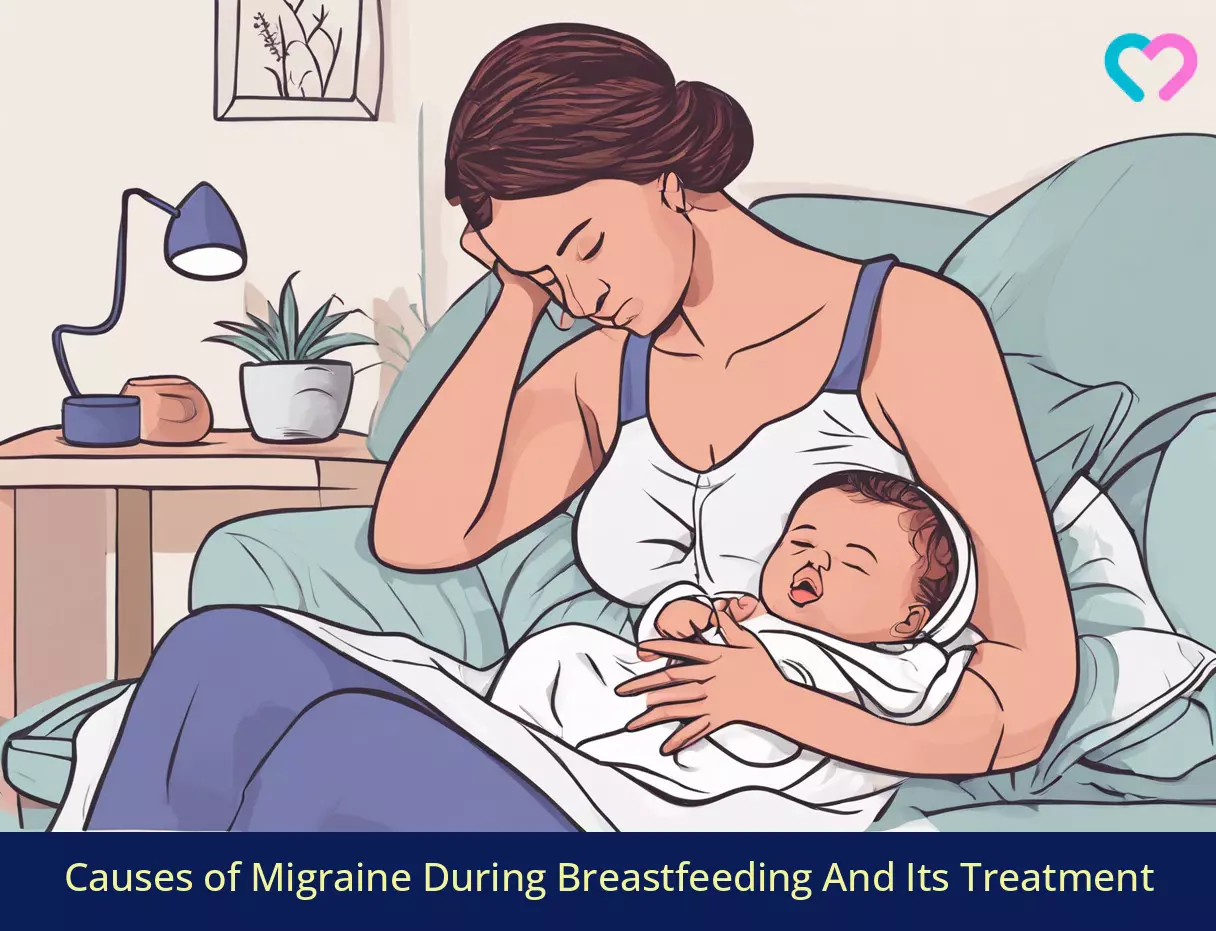
Image: Stable Diffusion/MomJunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Coping with migraines and breastfeeding.https://www.youtube.com/watch?feature=shared&v=U995cZkU3WU
References
- Migraine.
https://medlineplus.gov/migraine.html - Migraine and other headache disorders.
https://www.acog.org/clinical/withdrawn-document?utm_source=redirectcu090&utm_medium=web&utm_campaign=int - Susan Hutchinson et al.; (2013); Use of Common Migraine Treatments in Breast-Feeding Women: A Summary of Recommendations.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3974500/ - BOTOX.
https://www.fda.gov/media/77359/download - New moms with migraine: Understanding postpartum headache.
https://americanmigrainefoundation.org/resource-library/postpartum-headache/#:~:text=This%20phenomenon%20is%20called%20postpartumattacks%20within%20the%20first%20month. - Understanding migraine treatment in the emergency room.
https://americanmigrainefoundation.org/resource-library/understanding-migraine-treatment-in-the-emergency-room/#:~:text=Go%20to%20the%20ER%20ife.g.%20light%20sensitivity%2C%20nausea). - What to Know About Migraine While Breastfeeding.
https://americanmigrainefoundation.org/resource-library/what-to-know-about-migraine-while-breastfeeding/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Morgan Jackson
Read full bio of Jessica Albert
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny