Milk allergy in infants is fairly common. Breastmilk is the sole source of nutrition and energy for babies for the first six months, and babies seldom show signs of allergies to breastmilk. However, formula milk or cow’s milk may trigger allergic reactions. Further, the signs and symptoms of the allergy are typically evident immediately or within an hour or two of consuming the milk.
Read on to learn more about milk allergy in babies, including its causes, signs, treatment, and substitutes you may use in place of milk to provide the required nutrition.
Key Pointers
- Milk allergy occurs when the body’s immune system treats milk proteins as foreign entities, resulting in an immune attack.
- Approximately two to three percent of babies may experience allergic reactions to animal-based milk.
- A family history of milk allergies and the presence of other conditions, such as asthma and eczema may increase the risk of milk allergies in babies.
- Symptoms of milk allergy may include hives, difficulty breathing, gastrointestinal issues, and swelling of the face.
- Management of milk allergies may involve avoiding milk, except breastmilk, and substituting it with soy milk or hydrolyzed formula.
What Is Milk Allergy?
Milk allergy is the condition when the body’s immune system mistakes the milk protein to be a foreign body or something that harms the body and attacks it
(1). Since the immune system behaves defensively, like it would when fighting a pathogen, the body displays symptoms of an illness.
About 2-3% of babies have a milk allergy.
Do note that we are referring to allergy related to the milk sourced from animals. And that brings us to the next question.
Can A Baby Be Allergic To Breastmilk?

Image: Shutterstock
No, an infant cannot be allergic to breastmilk since it is made specifically for consumption by the human infant (2). The American Academy of Pediatrics states that if the infant is showing signs of allergy to breastmilk, it could be an allergy to a substance that the breastfeeding mother has eaten (3). An infant could exhibit allergy-like symptoms after consuming breast milk.
But that could be an allergy to the animal-milk proteins, which the mother could have consumed earlier and passed to the baby through breastmilk. This happens only when the mother passes on an allergy from the milk she has consumed.
Nina Herrera, a mother and vlogger, recounts the challenge she faced when her son developed an allergic reaction to her breast milk due to the specific foods she was consuming. She reflects, “Around the age of two months, when Jayden turned two months old, we started noticing that his stool was very mucousy and started having little red drops of blood in it… We immediately called our doctor; we were very scared as new parents with our first baby. We were not sure what was going on.
“They figured that it must be some sort of allergy that was causing the GI reaction and that his gastrointestinal system was reacting to something that he was eating. At that time, he was only having breast milk. So it was something I was eating that was triggering him and causing the blood in his stool… They ended up putting me on an elimination diet, so I tried eliminating different foods, and through that, we were able to determine that it was cow’s milk that was triggering Jayden (i).”
Can Milk Allergy Result In Formula Allergy?
Yes, formulas contain proteins derived from cow milk. It means, an infant with milk allergy will also have an allergy to formula milk.
Is Milk Allergy Same As Lactose Intolerance?
No, the two are different.
| Milk allergy | Lactose intolerance |
|---|---|
| The immune system’s reaction to milk protein | The small intestine does not make the lactase enzyme that digests lactose sugar in milk |
| Involves the immune system | Involves the digestive system |
| Cannot consume milk at all | Can consume lactose-free milk |
| Babies can consume and digest breastmilk | Babies may be unable to consume and digest breastmilk |
What Causes Milk Allergy In Babies?
The causes of milk allergy are not known.
The physiology of the condition is that when food passes into the small intestine, the immune system mistakes it to be a foreign body and attacks it, causing an allergic reaction.
Genetics and environmental factors seem to be the fundamental cause of food allergies, while other factors increase an infant’s risk of developing milk allergy (4).
What Are The Risk Factors For Developing Milk Allergy?
A baby can be at a greater risk of developing a milk allergy in the following scenarios:
- A family history of allergies: A baby has 75% chances of developing food allergies if both the parents have a food allergy. The risk comes down to 40% when only one parent has an allergy. A family member with a food allergy can also make the infant susceptible to milk allergy (5).
- Repeated early exposure: A baby who is excessively given cow’s milk at an early age can develop milk allergy.

Image: IStock
- Being firstborn: Scientists observe that firstborns are more prone to food allergies than the subsequent babies (6). It is believed that firstborns do not have exposure to germs like the younger siblings do, which makes their immune system delicate and susceptible to allergies.
- Asthma and eczema: Children suffering from asthma and eczemaiA skin condition that causes itchy, red, and scaly patches on the skin due to various factors such as allergies, genetics, or stress. have a higher risk of food allergies such as milk allergy (7). However, it is not known what links the two health conditions to milk allergies. Since asthma and eczema are a result of a faulty immune system, they could make the infant prone to food allergies as well.

Image: IStock
- Presence of other food allergies: If the baby has other food allergies, they may be allergic to milk as well, so be extra careful before using cow milk for babies.
If your baby has any of these risk factors, then be alert and check for any symptoms of allergy.
What Are The Symptoms Of Milk Allergy In Babies?
The symptoms appear a few minutes to several hours after the consumption of milk or milk products. A baby with milk allergy will display the following signs (8):
- Skin hives/ rashes: These are tiny, red or dark pink rashes that appear all over the body. They look like bumps, often appear in clusters and tend to be itchy.
- Swelling of the face: Parts of the face like the eyelids, cheeks, mouth, tongue, and lips get swollen.
- Shortness of breath and coughing: Muscles of the neck swell, making it difficult to swallow, and resulting in fits of coughing and shortness of breath.
- Stuffiness and runny nose: The baby may show cold-like symptoms such as a runny nose and wheezing while breathing.

Image: IStock
- Abdominal discomfort: Stomach cramps and severe pain across the entire abdominal region.
- Nausea and vomiting: Constant feeling of nausea, sometimes followed by vomiting.
- Diarrhea: The infant may have diarrhea, and sometimes the poop may even contain blood.
- Colic and fussiness: Constant crying accompanied by severe, uncontrollable fussiness.
The above symptoms occur at a higher intensity in the cases of severe allergic reaction to milk. Such a situation is called anaphylaxisiAn extreme reaction to an allergen causing breathing difficulties and loss of consciousness. or anaphylactic shock. Take your baby to a pediatrician or allergist as soon as you spot any symptoms of milk allergy.
How Is Milk Allergy In Infants Diagnosed?
Milk allergy is diagnosed using the following two methods:
- Suspected food elimination: After learning about the symptoms, the doctor will ask you to eliminate milk from the baby’s diet. If the existing symptoms improve and the baby does not display the symptoms again, then it can be concluded that the baby has a milk allergy.
- Skin prick test: It is also called a percutaneous test. Here a small quantity of diluted allergen, milk protein in this case, is injected into the upper layers of the skin. If the infant is allergic to the substance, then they will display an itchy bump that would develop at the site of injection, thus indicating an allergy. The test is safe, but usually never performed on infants below the age of six months (9). Since the babies start having cow milk after the age of 12 months, this test can be performed on a baby older than a year.
- Blood test: A blood test will check for the presence of immunoglobulin E (IgE) antibodies, which are present in the case of food allergies in babies.
Treatment of milk allergy is often the biggest concern for the parents.
How Is Milk Allergy In Babies Treated?
Milk allergies can only be managed but not treated (10). Here is how it can be managed (11):
- Antihistamines: These medicines curtail milk allergy symptoms such as swelling, hives, runny nose, and abdominal pain. It does not cure milk allergy but just helps keep the symptoms under control.
- Epinephrine: Also called adrenaline, epinephrine is a hormone that controls an anaphylactic shock. It is administered through an auto-injector when a baby sustains anaphylaxis.
- Avoidance of milk by mother: In the case of breastfed infants, a mother can consider avoiding milk as long as her infant is reliant on breastmilk.
Parents need to work closely with healthcare providers to develop a management plan tailored to their child’s specific needs. This plan may involve dietary adjustments and monitoring for potential cross-reactive allergies. There is no doubt that the baby has to avoid milk entirely. But doesn’t that deprive the baby of nutrients?
What To Feed A Baby With Milk Allergy?
The following foods are excellent, nutritionally equivalent, substitutes for cow milk:
- Soy-milk or almond milk formula: Soy-milk formula is manufactured from soy protein that is derived from soybean. Similarly, almond milk is made from almonds. It is naturally free from milk proteins and thus an ideal alternative for babies with milk allergy. Soy formula is recommended for infants with a clinically-proven milk allergy (11).
 Did you know?
Did you know?- Hydrolyzed formula: In this hypoallergeniciA product that contains fewer allergy-inducing components. formula, the milk protein is broken down into smaller amino acid chains that do not elicit an immune system response (12). The formula can be either partially-hydrolyzed or extensively-hydrolyzed. Consult your baby’s pediatrician before choosing a hypoallergenic formula.
- Calcium-rich vegetables: Milk is a good source of calcium for growing babies. However, you can get adequate quantities of calcium from vegetables too. If your baby is a solid food eater, then you can introduce calcium-rich vegetables such as spinach, broccoli, kale, and even carrots into their diet. All green leafy vegetables and beans contain significant quantities of calcium (13). Most vegetables can be safely introduced to babies at the age of six months.
- Meat and eggs: Meat contains several micronutrients while eggs are an excellent source of vitamins, such as vitamin B and vitamin D. Meat, except fish, is safe to introduce at the age of six months. Eggs and fish can be introduced once the infant is a year old (5).

Image: IStock
- Breastmilk: Breastmilk also makes an excellent substitute to cow’s milk for as long as you can feed your baby. The World Health Organization states that you can feed your baby even beyond the age of two years (14).
Your baby won’t miss the nutrition provided by milk when you substitute it with equally nutritious solid foods. But did you know that milk protein could be hiding in foods where you least expect it?
 Nutrition fact
Nutrition factCan Milk Allergy Also Cause Dairy Allergy?
Yes. Milk allergy is not just allergy to liquid milk, but also to other milk or dairy products. Milk proteins are found in some non-dairy, packaged products. The following is the list of products to avoid when the baby has a milk allergy (15):
- All dairy products including cheese, cottage cheese, butter, yogurt, ice cream, and milk desserts like custard
- Foods containing casein, whey, and lactose
- Creams and sour creams
- Chocolates and candies
- Baked products, especially milk bread
- Canned fish; it often contains added milk proteins for better taste
Always check the labeling of the food you purchase to prevent accidental exposure to milk proteins.
Do Babies Outgrow Milk Allergy?
Yes. Experts state that infants can outgrow milk allergy by the time they are three to four years old. However, some continue to be allergic to milk until they are in their teenage.
About 80% of children outgrow milk allergy by the time they are 16 years old (16). The chances of that, however, depending on the severity of the allergy.
How To Prevent Milk Allergy In Infants?
There is no single and specific method to prevent the onset of milk allergy. However, you can take precautions to minimize the risk of a baby developing a milk allergy:
- Introduce milk only after 12 months. While this does not guarantee the prevention of milk allergy, it reduces the chances of it.
- Introduce milk gradually. Do not start with a bottle full of it. Instead, start with small quantities so that the body gets adequate time to get used to the new food. Also, if the baby turns out to be allergic, a small quantity of milk may elicit a weaker allergic reaction.
This tip is also applicable for infants on a formula containing milk proteins. For more on milk allergies in babies, read our FAQ section next.
Frequently Asked Questions
1. Is food protein-induced enterocolitis syndrome the same as milk allergy?
No, food protein-induced enterocolitis syndrome (FPIES) and milk allergy are different although milk can trigger FPIES. The following are the differences (17) (18):
| FPIES | Milk Allergy |
|---|---|
| Non-IgE mediated, i.e., no antibodies in the blood | IgE-mediated, i.e., antibodies are present in the blood |
| Triggered by milk, soy, rice, among many foods | Only triggered by milk |
| Vomiting and diarrhea are the primary symptoms | Symptoms are seen on the skin and abdominal region |
| Usually resolves by four years | May persist till teenage |
FPIES can be hard to detect during blood tests since it does not cause the formation of antibodies like those seen in milk allergy. Observation of symptoms and their pattern can help a pediatrician diagnose FPIES.
2. How to differentiate between reflux and milk allergy?
A baby with reflux will not display other allergy symptoms such as skin hives and blood-laden diarrhea. Also, reflux can happen after consuming any food while milk allergy symptoms only emerge after the consumption of milk or milk products.
3. Is rice milk ideal for babies with a milk allergy?
Yes. You can consider giving fortified rice milk specifically made for babies if your child has a milk allergy. However, rice milk contains too many calories and very little protein. It could also be contaminated with arsenic. For this reason, the US Food and Drug Administration recommends avoiding rice products for infants and toddlers. So it is best to stick to hydrolyzed formula or soy formula for your baby with a milk allergy.
4. Can I give probiotics to a baby with a milk allergy?
No, it is best to avoid giving any probiotics to your baby with a milk allergy. There is limited research on the benefits of probiotics for infants with milk allergy. If you still want to consider them, then consult the pediatrician first.
5. Can a milk allergy in infants develop later in life?
Children can develop milk allergy at any age; however, it is more prominent in younger ages (1).
6. Can a milk allergy in infants affect the growth and development in later life?
Studies have indicated growth related problems in children with cow’s milk allergy, but significant improvements in height and weight have been seen in children who were given formula substitutes (20).
Milk allergy in infants occurs when the immune system attacks the milk proteins. These reactions are usually towards cow milk, and there can be an issue if they are fed with cow milk-based formulas. Allergic reactions toward breast milk are not seen since it is a specialty for the conception of infants. However, some content in breastmilk due to maternal diet may trigger allergic reactions. Symptoms including skin hives, swollen lips, breathing issues, colic, and abdominal discomfort are common in babies with milk allergies. Antihistamines are used to treat milk allergies, and it is recommended to avoid milk and milk products that trigger allergies.
Infographic: What Are The Symptoms Of Milk Allergy In Babies
Milk allergy is a common allergy in babies and young children that occurs when the body’s immune system reacts to the milk proteins. So, if you’re planning to introduce milk other than breast milk into your baby’s diet, scour through the infographic below to learn about common symptoms of milk allergy to look out for in babies. Illustration: Momjunction Design Team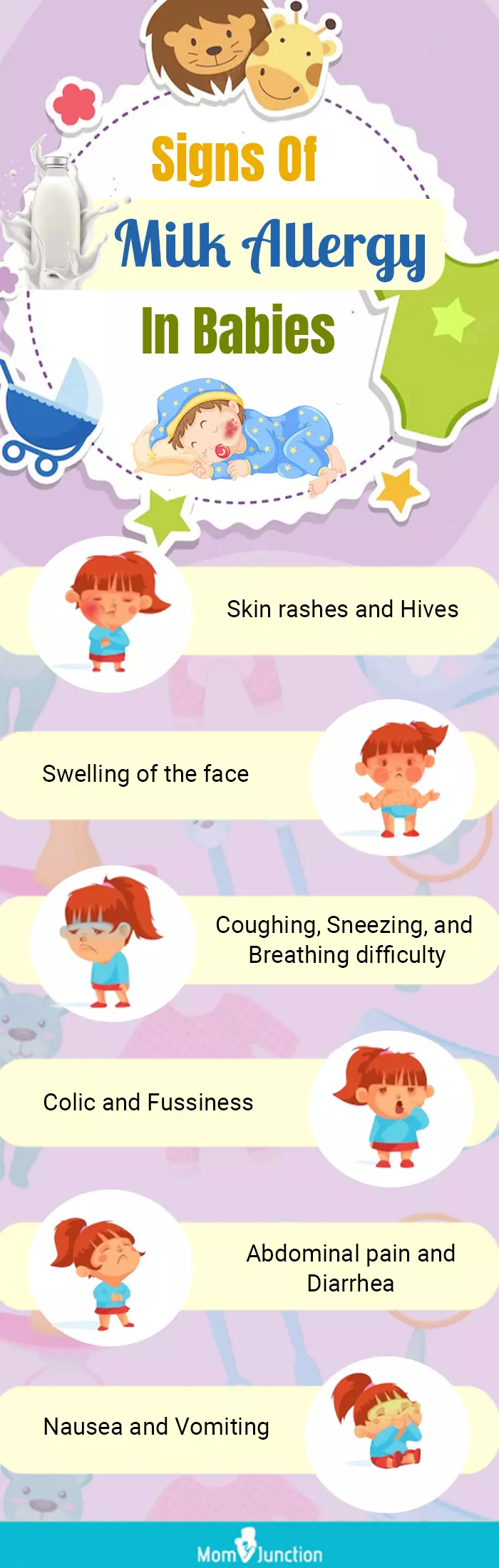
Illustration: Milk Allergy In Infants: Causes Symptoms And Treatment

Image: Dall·E/MomJunction Design Team
Watch a concise video outlining key signs of Cow’s Milk Protein Allergy (CMPA) to quickly recognize symptoms in your child.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Cow’s milk protein allergy in baby | Breastfeeding a baby with allergies.https://www.youtube.com/watch?v=tqdK7oppZUc&feature=youtu.be
References
- Milk Allergy in Infants.
https://kidshealth.org/en/parents/milk-allergy.html - LISTENER QUESTION: CAN MY BABY BE ALLERGIC TO MY MILK?.
https://healthcare.utah.edu/the-scope/health-library/all/2017/05/listener-question-can-my-baby-be-allergic-my-milk - Infant Allergies and Food Sensitivities.
https://www.healthychildren.org/English/ages-stages/baby/breastfeeding/Pages/Infant-Allergies-and-Food-Sensitivities.aspx - Potential Genetic and Environmental Determinants of Food Allergy Risk and Possible Prevention Strategies.
https://nap.nationalacademies.org/read/23658/chapter/7 - CPMC Food Allergy Care.
https://www.sutterhealth.org/cpmc/services/allergy/food-allergy - Was It Something I Ate? Understanding Food Allergies.
https://hms.harvard.edu/sites/default/files/assets/Sites/Longwood_Seminars/2015_Longwood%20Seminar%20Allergy%20Reading%20Pack.pdf - Carlo Caffarelli et al.; (2016); Asthma and Food Allergy in Children: Is There a Connection or Interaction?.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4821099/ - Milk Allergy.
https://www.virtualpediatrichospital.org/patients/cqqa/milkallergy.shtml#4 - Testing & Diagnosis.
https://acaai.org/allergies/testing-diagnosis/ - Milk Allergy.
https://kidswithfoodallergies.org/living-with-food-allergies/top-food-allergens/milk-allergy/ - Choosing an Infant Formula.
https://www.healthychildren.org/English/ages-stages/baby/formula-feeding/Pages/Choosing-an-Infant-Formula.aspx - Hypoallergenic Infant Formulas.
https://publications.aap.org/pediatrics/article-abstract/106/2/346/62820/Hypoallergenic-Infant-Formulas?redirectedFrom=fulltext - Calcium and Strong Bones.
https://www.pcrm.org/good-nutrition/nutrition-information/health-concerns-about-dairy/calcium-and-strong-bones - Breastfeeding.
https://www.who.int/health-topics/breastfeeding - Milk Allergy.
https://www.foodallergy.org/living-food-allergies/food-allergy-essentials/common-allergens/milk - Milk & Dairy.
https://acaai.org/allergies/allergic-conditions/food/milk-dairy/ - Related Medical Conditions.
https://www.foodallergy.org/resources/related-medical-conditions - Food Protein-Induced Enterocolitis Syndrome.
https://rarediseases.org/rare-diseases/food-protein-induced-enterocolitis-syndrome/ - Cow’s Milk Alternatives: Parent FAQs.
https://www.healthychildren.org/English/healthy-living/nutrition/Pages/milk-allergy-foods-and-ingredients-to-avoid.aspx - Growth in infants with cow’s milk allergy.
https://pubmed.ncbi.nlm.nih.gov/16527091/#:~:text=Introduction%3A%20Approximately%202%2D3%20%25,and%20a%20milk%2Dfree%20diet
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Huda Shaikh
Read full bio of Rohit Garoo
Read full bio of Swati Patwal
Read full bio of Vidya Tadapatri