Image: Shutterstock
Molar pregnancy, also known as the hydatidiform mole, is a pregnancy complication where the trophoblasts (cells in the placenta) grow abnormally. Usually, molar pregnancy may end naturally in miscarriage, or if not, the doctors may recommend procedures to remove the abnormal growth. However, a woman can conceive and have a successful pregnancy after removing the molar pregnancy. You may plan the next pregnancy as per your healthcare provider’s recommendations. Read on to know more about the causes, symptoms, diagnosis, and treatment of molar pregnancy.

Key Pointers
- Severe morning sickness, hypertension, and cyst in ovaries are a few symptoms of molar pregnancy.
- Women aged below 20 and above 40, Asian women, and those with a higher number of births are more at the risk of having a molar pregnancy.
- Ultrasound with doppler and blood test to check hCG levels are a few ways to diagnose it.
- Hysterectomy, dilation and evacuation, and medications can effectively treat molar pregnancy.
What Is A Molar Pregnancy?
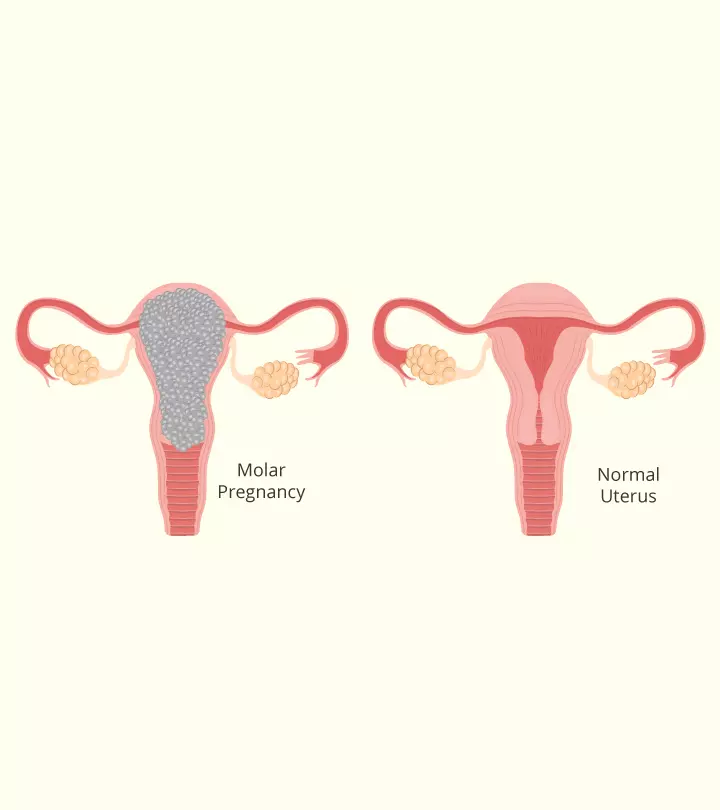
A molar pregnancy occurs when the sperm does not fertilize the egg properly, and the cells that are responsible for the formation of the placenta form a cluster of abnormal cells instead (1). Such a fertilized egg, which cannot survive long, implants in the uterus but does not reach the term.
In such a pregnancy, the abnormally grown cluster of fluid-filled cells takes over space inside the womb. Molar pregnancy is also called hydatidiform mole, where ‘hydatid’ means fluid-filled sacs or cysts and ‘mole’ means a mass of cells. These cells, known as trophoblasts, can develop into abnormal masses, resulting in the formation of a benign trophoblastic tumor. This is why a molar pregnancy is also called a trophoblastic disease (2).
There are two types of molar pregnancies:
- Complete molar pregnancy (Dioploid) : It occurs when an empty ovum without any genetic material gets fertilized by a sperm. In this case, the fetus does not develop. Duplication of haploid sperm or sometimes dispermic fertilization of empty ovum occurs.
- Partial molar pregnancy (Triploid) : It happens when two sperms fertilize the egg. Too much genetic material leads to abnormal development of a fetus that cannot survive; usually evidence of fetal tissue or fetal RBC is present.
The actual cause for molar pregnancy is unknown, although there are certain known risk factors for it. Keep reading to know more about it.
What Are The Risk Factors For Molar Pregnancy?
A molar pregnancy occurs in 1 out of 1000 pregnancies. Molar pregnancy, as estimated by the National Institutes of Health, occurs in approximately 60 to 120 cases per 100,000 pregnancies in North America and Europe. If someone has experienced a molar pregnancy before, their risk for future pregnancies increases by 1% to 2%. Moreover, women aged over 40 years or those with more than two previous pregnancy losses also face higher chances of molar pregnancy (3). The other risk factors include (4):
- Maternal age 40 years

- Higher number of births
- Asian women
- Nutritional deficiencies, such as folate, beta-carotene, or protein deficiency
- History of gestational trophoblastic disease (the recurrence rate being one in 100)
Are there any signs that can indicate molar pregnancy? The section below explains it.
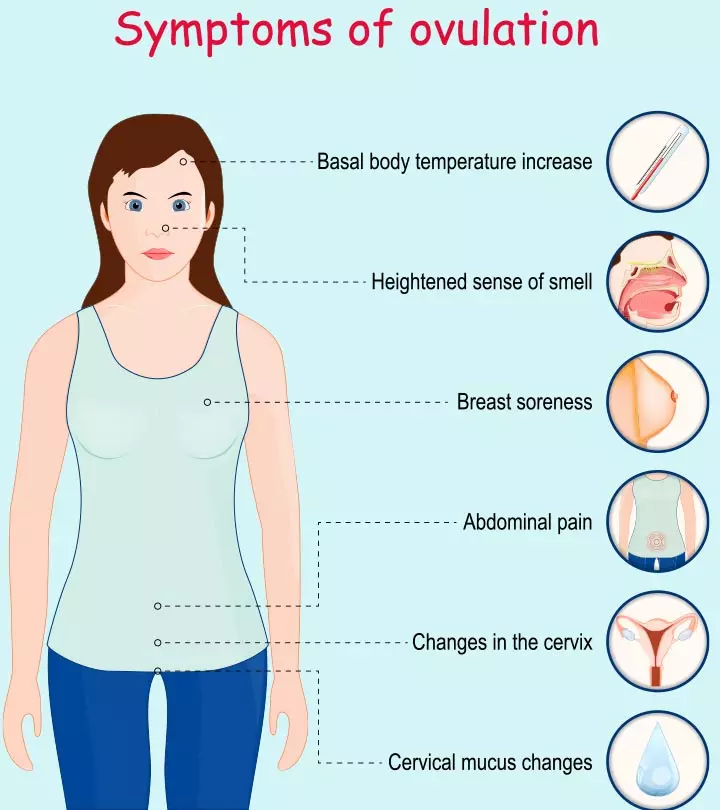
What Are The Symptoms Of A Molar Pregnancy?
In the case of a molar pregnancy, you might experience symptoms that are similar to those of a normal pregnancy, such as missed periods (5). Also, there are specific symptoms that could indicate a molar pregnancy (6):
- Unusual vaginal bleeding that contains blood clots; passing grape-like vesicles or a discharge that is watery and brown.
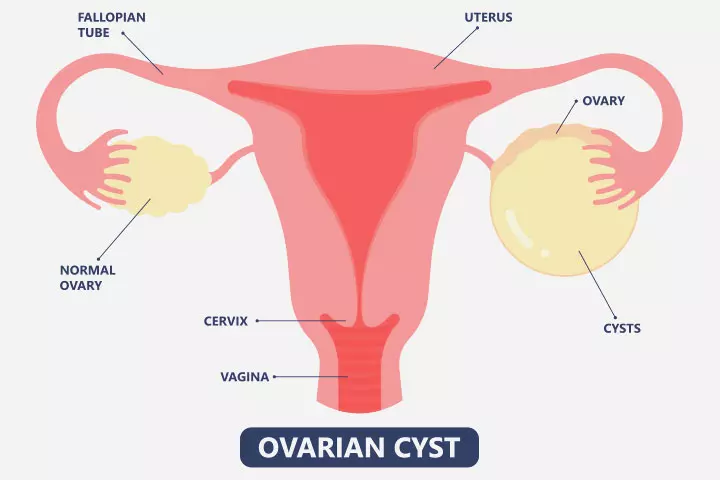
- Cyst in ovaries (7), theca lutein cystiFunctional ovarian cysts believed to be caused by excess circulating gonadotropins. > 6cm, ovarian stimulation by hCG
- Pelvic pressure or pain

- Severe morning sickness
- High blood pressure (hypertension/ preeclampsia)
- An extremely large soft uterine enlargement
- Anemia
- Abnormal appearance of the uterine cavity in the first ultrasound (also called a ‘snowstorm’ pattern)
- HyperthyroidismiA condition where the thyroid gland makes and releases high levels of thyroid hormone. , leading to weight loss and increased appetite (rare symptom)
A molar pregnancy is emotionally disturbing, but it can also pose risks to your physical health, especially your reproductive system.
 Quick fact
Quick factFeatures Of Partial Mole
- Vaginal bleeding in late first or second trimester — missed or incomplete abortion
- Uterine enlargement and hyperemesisiA condition characterized by excessive nausea and vomiting during pregnancy with a possibility of causing dehydration. , pregnancy-induced hypertension, and hyperthyroidism.
What Are The Complications Of A Molar Pregnancy?
Regular pregnancy monitoring is crucial to detect any abnormalities early on. Early diagnosis of molar pregnancy may not be associated with a complication, but a delay in diagnosis can give rise to the following conditions:
- Hemorrhage
- Anemia
- Ovarian cysts torsion/ pain
- Breathlessness (when it spreads to the lungs)
- PreeclampsiaiA pregnancy disorder characterized by high blood pressure, water retention, and protein content in urine. affecting the kidneys and the liver function
- Excess production of thyroid hormone causing heart palpitations and other thyroid hormone effects
If a molar pregnancy is left untreated or does not get appropriately aborted, then it can lead to conditions, also known as gestational trophoblastic neoplasia, such as:
- Persistent GTD (gestational trophoblastic disease), which is associated with continuous and abnormal growth of the placental tissue.
- An invasive mole, wherein the tumor proliferates into the uterine wall. vagina and other pelvic structures.
- Metastatic mole, which is associated with the migration of molar cells to other organs like lungs, causing secondary tumors.
- Gestational choriocarcinoma, a kind of cancer spreading rapidly to any part of the body through the blood vessels or the lymphatic system.
Timely diagnosis, thus, becomes essential in the case of a molar pregnancy to prevent these complications.
 Quick fact
Quick factHow Is Molar Pregnancy Diagnosed?
Molar pregnancy is diagnosed in the following ways (4):
- Blood test to check for hCGiHuman chorionic gonadotropin (hCG) is a hormone produced by the placenta and helps thicken the uterine lining for fetal development. levels (serum beta hCG)
- Ultrasonography or ultrasound with doppler

- Histopathological examinationiA process where tissues of the body are examined under the microscope to detect characteristics of the illness. of molar tissue
- Other scans including x-rays, computed tomography (CT) or magnetic resonance imaging (MRI) to check if cancer has spread to the other areas of the body
Before doing the above tests, you will undergo a physical examination, and the doctor will go through your medical history to know about recent childbirth, miscarriage, or abortion.
The diagnosis of molar pregnancy becomes difficult if:
- The recent pregnancy and birth were healthy, and there are no signs to suspect a molar pregnancy until the symptoms become evident.
- A woman experiencing miscarriage does not know if she has passed a hydatidiform mole until it is tested in the laboratory.
Early diagnosis and treatment make molar pregnancy completely curable. Read the section below to know about the different treatment methods.
How Is Molar Pregnancy Treated?
The treatments for molar pregnancy include (8):
- Medication: If the abnormal cells grow large and cannot be sucked out, then medicines will be given to contract the uterus, thereby helping to evacuate its contents through the vagina in the case of partial mole.
- Dilatation and curettage (D&C): The cervix is dilated, and the uterine contents are removed by scraping and scooping the molar tissue. General anesthesia is given before the procedure.

- Dilation and evacuation (D&E): This is also done under general anesthesia. A thin tube is passed into the uterus through the vagina to suck out the abnormal cells.
- Hysterectomy: It involves surgical removal of the uterus. It is done only if the woman does not want to bear a child in the future.
Sometimes, even after the evacuation of the uterine contents, some abnormal cells remain in the uterine cavity. They usually go away in a few months, but if that doesn’t happen, then further treatment is needed for its removal. It is required in around 10% of the cases (4). In addition to the physical treatment, it is important to look after your mental well-being. Seek support from specialists, family and loved ones, and if necessary, support groups for emotional recovery.
Follow-Up
After the treatment, the blood and urine of the woman are regularly checked, typically every week, for the hCG levels. Around 56 days is required to normalize it and a follow-up is required six months after normalization. These regular checkups help detect any complications or recurrence early on. If there is an increase in the hCG amount, it may indicate the presence of abnormal cells in the uterus. If these cells do not evacuate through discharge, it could result in a condition called PTD (persistent trophoblastic disease).
If PTD spreads to other organs, it is diagnosed as cancer, and the patient needs chemotherapy. The chances of PTD are 1 in 7 among women with complete mole and 1 in 200 among women with partial mole (9).
When Can You Conceive After A Molar Pregnancy Is Treated?
Avoid conception until hCG level has been normal for six months. Use barrier methods as contraception instead of IUCDiAn intrauterine contraceptive device (IUCD) is a form of birth control that is placed inside the uterus to prevent pregnancy. .
Ideally, you should wait until after the treatment and observation period before planning another pregnancy, to make sure the entire molar tissue is flushed out of the body.
Sharing her concerns about conceiving three months after a molar pregnancy, Kara, a mother, reveals, “On the sixth, I had my third zero reading (of the last blood test for hCG levels) in a row from the lab. That caused the doctor to release me from my weekly blood draws and clear me for moving on with my life.
“For the last few months, I have been able to hide from the threat of a repeat molar pregnancy since I was not cleared to try to conceive again. My doctor claims the latest research from the oncologists suggests just three zero tests is fine, even if it means only a few weeks have passed. This news at first seems great, but then I worry that we will run into problems from getting pregnant sooner than we really should (i).”
If you do get pregnant earlier, the high hCG levels during a normal pregnancy can interfere with the blood tests and alter the diagnosis. So to ensure full recovery from the condition and prevent any harm to fetal development, use contraceptives until your treatment for molar pregnancy is complete (9).
What Are The Chances Of Having A Recurring Molar Pregnancy?
If you have had a molar pregnancy earlier, there is a 1% chance of the next one being a molar pregnancy. It means that 99 out of 100 women will have a normal pregnancy. However, if you have had more than one molar pregnancy earlier, then the risk in the next pregnancy increases to about 15-20% (10). If it repeats, it will be of the same histologic type. Therefore, consult your doctor for tailored care and guidance for your future pregnancies.
Frequently Asked Questions
1. Is a partial molar pregnancy considered a miscarriage?
A partial molar pregnancy is often considered a miscarriage or threatened miscarriage because the fetus develops abnormally and can’t survive for more than three months in a partial molar pregnancy (11).
2. How long can a molar pregnancy go undetected?
A molar pregnancy may go undetected until a routine ultrasound is performed at around 8 to 14 weeks or tests are done after a miscarriage (12).
3. When do molar pregnancy symptoms start?
There is no fixed time by which molar pregnancy symptoms start. However, vaginal bleeding, the most common symptom of a molar pregnancy, usually begins between six and 12 weeks of pregnancy (13).
Molar pregnancy occurs when a defective fertilized egg implants to form an abnormal placenta that results in a uterine tumor. The symptoms are similar to pregnancy but may be accompanied by vaginal bleeding, ovarian cysts, and abnormal first ultrasound. If left untreated, it may cause further complications. Factors such as nutritional deficiencies, advanced maternal age, or Asian origin may increase the risk of a molar pregnancy. Your Obstetric/Gynecology specialist may suggest medications or surgical excision of the abnormal growth depending on the condition. They may also tell you about the precautions to take to have a normal subsequent pregnancy and for optimum reproductive health.
Infographic: What Are The Symptoms Of Molar Pregnancy?
A molar pregnancy is a rare condition where the woman experiences fluid-filled cells in the uterus due to conception. It can lead to severe complications if left untreated. The infographic below presents symptoms of molar pregnancy to look for to get early intervention.

Illustration: Momjunction Design Team
Illustration: Molar Pregnancy: Types Symptoms Causes And Treatment

Image: Stable Diffusion/MomJunction Design Team
A molar pregnancy is a rare complication of pregnancy. Learn more about the signs, diagnosis, and treatment in this video.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Kara’s molar pregnancy;https://karasmolarpregnancy.blogspot.com/
References
1. Molar pregnancy; Healthdirect
2. Molar pregnancy; Miscarriage association
3. Partial Molar Pregnancy; Cleveland Clinic
4. Molar pregnancy; Betterhealth
5. Symptoms & diagnosis; Miscarriage Association
6. Signs and Symptoms of Gestational Trophoblastic Disease; American Cancer Society, Inc
7. Molar pregnancy; March of Dimes
8. Types of treatment for molar pregnancy; Cancer Research UK
9. Molar pregnancy; NHS
10. Risks and causes; Cancer Research UK
11. Hydatidiform mole; The Royal Women’s Hospital
12. Molar pregnancy information and support; Tommy’s
13. Symptoms of molar pregnancy; Cancer Research
14. Molar Pregnancy; MSD Manuals
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Subhashis Samajder
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Reshmi Das