Image: iStock
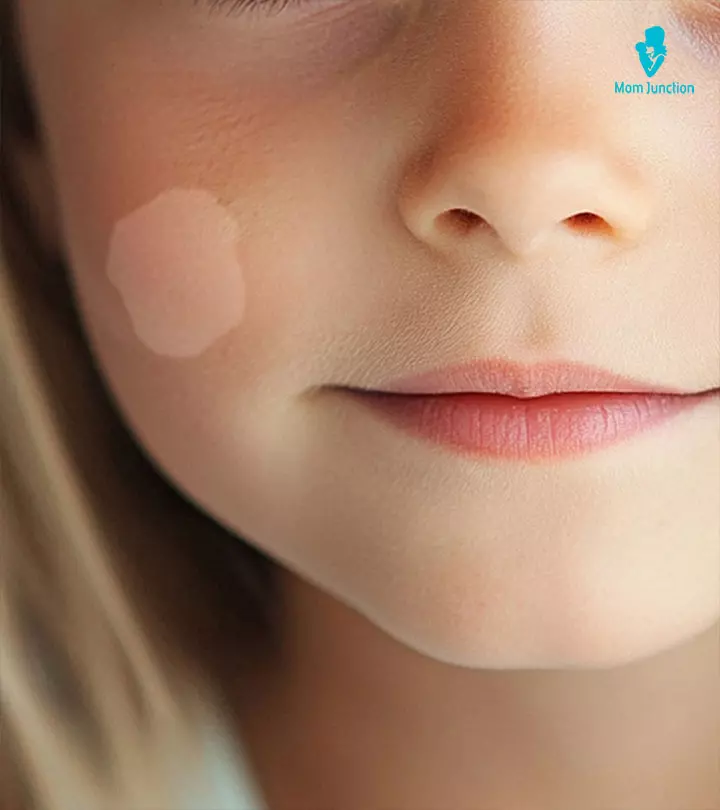
Molluscum contagiosum in children is a common viral skin infection that causes tiny skin-colored or pink bumps to appear on the child’s skin. It is a poxvirus infection that affects about 3% of the pediatric population. The CDC suggests that molluscum contagiosum is most common among children aged one to ten years (1) (2). The infecting virus stays inside these bumps and is mildly contagious. The bumps are painless, but they may be itchy and bothersome. Usually, these bumps clear over time, but you can use medications to clear the bumps faster. Keep reading to learn more about the symptoms, causes, diagnosis, and treatment of molluscum contagiosum in children.
The infecting virus stays inside these bumps and is mildly contagious. The bumps are painless, but they may be itchy and bothersome. Usually, these bumps clear over time, but you can use medications to clear the bumps faster. Keep reading to learn more about the symptoms, causes, diagnosis, and treatment of molluscum contagiosum in children.
Key Pointers
- Molluscum contagiosum is a mildly contagious viral skin infection.
- It causes painless pink bumps on the skin, sometimes accompanied by eczema.
- The virus spreads by touching infected lesions or surfaces, or sharing items with an infected person.
- The condition usually clears up on its own in 6-12 weeks, but treatment can speed up the healing process.
- Treatment options include oral therapy, topical therapy, or physical removal.
What Is Molluscum Contagiosum?

Molluscum contagiosum is a skin disease that spreads through person-to-person transmission via direct contact. Unlike chicken pox or measles, there is no pain or fever. However, there is a bit of itchiness, which the child may scratch and then touch other places on the skin, eventually spreading the infection from one part of the body/ skin to another (3) (1).
Symptoms Of Molluscum Contagiosum In Children

The symptoms of molluscum in children can be apparent or otherwise, depending on the infected part of the skin. A child infected with this virus develops tiny pink, flesh-colored round papules. The bumps or pimple-like things are hard to miss and can occur anywhere: the arms, legs, knees, under the armpits, back, tummy, legs, neck, face, and even genitals.
These little bumps are prominent and can appear in places that you cannot cover, making the child feel conscious and uncomfortable to go out in public. The bumps may appear individually or in patches of twenty or so. Usually, these little lumps are (3) (1) (4):
- Pinkish red, flesh-colored.
- Smooth and shiny.
- Firm like a pimple, but with a tiny dent or dimple in the center.
- Have a diameter of two to five millimeters and are usually painless, but can be itchy at times.
- Not seen on the palms of your hand or the soles of your feet.
- Temporary as they fall off after a period, but do not leave a scar, unless affected by bacteria.
According to Dr. Cheryl Bayart, MD, a pediatric dermatologist at the Cleveland Clinic, “What happens is the molluscum virus just hangs out in your skin. It evades your immune system’s recognition since it’s only in your skin’s top layer, or epidermis. At some point, your immune system catches on that it’s there and gets rid of the bumps. When that happens, you’re immune. You never get them again.” She further explains, “If you look at the bumps, they’re usually pink, domed-shaped. And sometimes if you look up close, they’re what you call umbilicated (meaning they look like they have a little belly button in the middle). That’s the core of viral particles or the contagious part of the molluscum. Once the body’s immune system kicks in and there’s crusting or a little scabby spot, that particular molluscum isn’t contagious anymore (5).”
In some cases, eczema develops around the molluscum contagiosum bumps. This can happen before or during the treatment (4). Also, a study revealed that the presence of pruritus and surrounding eczema was higher in children with molluscum contagiosum (6).
When you see the bumps on your child’s skin, it is time to go to a dermatologist.
 Point to consider
Point to considerWhat Causes Molluscum Contagiosum In A Child?
Most healthy children are immune to the virus. However, molluscum contagiosum is contagious and spreads through contact. Your child can acquire the virus if he or she (4) (7):
- Touches an infected kid’s lesions during play or activities.
- Touches one lesion, scratches and touches another part of the body.
- Contacts surfaces that have been infected by the virus.
- Shares towels or bed linen used by other kids or adults who are infected with the virus.
- Touches or plays with toys, books, and other contaminated items.
- Shares sports equipment such as shoes, gloves, helmets or mats.
Teenagers and young adults can get this through sexual contact as well. The infection can spread from one part of the body to another if the child scrapes or touches the lump and then touches another part of his body (5).
Amy, a blogger and a mother of two boys, shares how her older son Oscar got molluscum contagiosum. She says, “I had been taking Oscar to a few play groups a week ever since he was little. I had heard about how babies would have high chances of catching something, but I will never forget how much I freaked out when I first saw babies sucking on toys, throwing them back into the pile ready for another baby to come by and slobber on. One day when Oscar was around 7 months old I was changing his clothes when I noticed a couple of weird bumps on his arms. They didn’t look threatening at all though- normal skin colour, but quite raised looking almost like a white head (like it had something inside, but not hard and not quite pus-like). I kept check on it and to my dismay these spots just kept increasing in number in clusters until it spread to all around his arms and torso, chest and back. I took him to see a GP to discuss that along with his eczema (Oscar had been getting eczema since around 4 months old, coming and going along with the weather changes) as soon as I could. When the GP told me this thing was a virus with a horrible sounding name – Molluscum Contagiosum, I was horrified and upset.” She further shares some ways she managed her baby’s condition as well as eczema flare-ups, including long-sleeve tops, baby wash and cream, oat flour, and calamine lotion (i).
 Quick fact
Quick factDiagnosis Of Molluscum Contagiosum
Molluscum in children is diagnosed by clinical examination of the bumps on the skin. The doctor may investigate the lumps by having a close look at them or by scraping the skin surface and sending it for a biopsy. Once the doctor confirms it is molluscum contagiosum, they may recommend a treatment procedure (9).
Complications of Molluscum Contagiosum
Molluscum lesions are usually harmless and resolve spontaneously without scarring. However, scarring may occur if the lesions are scratched, or attempted to be removed by scraping or scooping, but they are not permanent. Dr. Cheryl Bayart says, “It does leave little pock-like scars in kids. But since they’re not seen in adults, it’s likely that they go away with time as the skin stretches and grows. It’s typically not permanent (5).”
Secondary bacterial infection is the most common complication, especially in people with reduced immune activity (e.g. patients with HIV/AIDs) (1). Pink eye (conjunctivitis) in kids may occur when the eyelids are infected while the viral infection may trigger an autoimmune reaction causing a skin inflammation known as disseminated secondary eczema (7).
Molluscum Contagiosum Treatment
The lumps on the body appear around two to seven weeks after the child is infected with the virus.
Usually, doctors do not recommend treatment as the condition disappears after six to 12 weeks. The condition spreads quickly, so even as lumps on one area of the body disappear, fresh ones may appear on other parts as the virus spreads.
It may take anywhere between three months and three years, or even five, for the infection to go away completely. In the initial stages, your doctor may ask you to let the body heal itself. While molluscum contagiosum is not as serious as other skin infections, it can be uncomfortable and make the patient unsightly (3) (8).
Therefore, it is good to consult a dermatology specialist for the best course of action for eliminating the condition. The dermatologist may suggest a few options to treat Molluscum Contagiosum in kids (8) (9).
- Oral therapy using medications such as oral cimetidine is ideal for young children who do not want the bumps physically removed because of the pain involved in the procedure. This treatment takes time and gradually relieves the child from the bumps.
- Topical therapy involves the use of prescribed creams like Tretinoin and Sinecatechin and over-the-counter creams, such as salicylic acid and potassium hydroxide, to treat molluscum contagiosum. These creams are usually marketed for treating warts and bumps but might also work on molluscum contagiosum bumps. However, the FDA recommends against using any creams that specifically state to cure molluscum contagiosum.
- Cantharidin (beetle juice) is the first FDA-approved drug for molluscum contagiosum (10). The American Academy of Dermatology Association recommends that Cantharidin be applied only in a doctor’s presence and needs to be washed off with soap and water as it may cause serious chemical burns, and scarring.
- In January 2024, the FDA approved Berdazimer topical gel with a concentration of 10.3%. This drug can be topically applied and is safe for both adults and children aged one year and older. It is also the first drug to be approved by the FDA to be applied at home, specifically for the treatment of molluscum contagiosum (11).
- Physical removal of the lumps involves freezing (cryotherapy) them using liquid nitrogen or burning them using laser therapy. Doctors may also try curettage, done through piercing and scraping of the lumps. These procedures should be performed by a trained medical practitioner using local anesthesia. They may result in pain and scarring and are not recommended for children (7).
More often than not, molluscum contagiosum is self-limiting and eventually leaves the body without causing any pain or discomfort. Each child may respond differently to treatments, and factors like age, the severity of the infection, and any underlying skin conditions may affect the treatment choice. If you think your child has had the infection for far too long, their doctor might suggest one of the above-mentioned treatments.
 Quick tip
Quick tipNatural Remedies For Molluscum Contagiosum In Children
There is no 100% effective treatment for molluscum contagiosum infection control because the treatments can only limit the infection to some extent. Complete eradication of the virus is possible only when the patient takes care to prevent the virus from spreading. Therefore, prevention is better than cure.
Here we share some natural remedies for molluscum contagiosum to provide some relief from any itching or tingle that the lumps might cause. However, they do not cure the condition nor can they prevent the spread of the virus.
1. Garlic
Studies have shown that garlic has an immunomodulatory effect (12), meaning it boosts the child’s immunity. Garlic helps the immune system to adjust and modify the immune response to the virus and reduce the time taken for curing molluscum contagiosum. Garlic also has anti-inflammatory properties and is used to treat acne, psoriasis, and other skin conditions.
- After a bath, pat the infected area dry and place finely minced garlic on it.
- Cover it with a bandage to hold the garlic in place.
- Wash the area the next day and repeat the process.
2. Tea tree oil
Tea tree oil has antifungal and antimicrobial properties that can help fight the virus (13). Every day, after a bath, dab the infected lumps with fresh cotton swabs soaked in tea tree oil. Do this twice a day to accelerate the treatment time. Use tea tree oil for kids every day until the bumps start becoming smaller and finally disappear.
3. Coconut oil

Coconut oil has antibacterial and antifungal properties that make it a natural cure for skin infections (14). Coconut oil is also a good moisturizer for skin and hair, and smells good too! Coconut oil has been used as a remedy to treat molluscum contagiosum for years. Apply pure coconut oil on the affected region at least thrice every day. You can also slightly massage the area but avoid rupturing the bumps to prevent the spread of the infection.
4. Olive oil
Olive oil is one of the most efficient natural remedies for treating skin infections. Ozonated olive oil contains ozone, which can effectively help in fighting infection causing fungi, bacteria, and cancers (15). Apply olive oil directly on the affected areas to relieve any pain and itching on the skin.
5. Bleach
A bleach bath can be an excellent idea to prevent the spread of the infection through the body. Bleach has antibacterial properties and prevents the accumulation of bacteria (16). Add some bleach to your child’s bath and let them soak in it for at least 10 minutes. Then, clean them with fresh water, pat them dry, and apply tea tree oil to the infected areas.
6. Neem
A traditional remedy used in India, neem has properties that fight pox viruses in children (17). Boil the leaves in water and add the water to your child’s bath. If you do not have access to leaves, apply neem oil to the infected area. Neem also boosts immunity to fight the infection-causing virus.
If one of your kids has the infection, use neem water for a bath for the rest of the family to prevent the infection from spreading.
7. Sea salt
Sea salt is an excellent natural remedy to treat molluscum contagiosum. And, there is plenty of it on the planet. Try this solution twice every day to get rid of the bumps caused due to infection.
- Mix a few spoons of sea salt and honey.
- Add a spoonful of olive oil and mix it well.
- Apply this paste to the affected area and massage it gently for at least 10 minutes.
- Wash it off with clean water and let the skin dry naturally.
8. Apple cider vinegar
Apple cider vinegar is acidic and can cause a burning sensation when applied. Nevertheless, it works wonderfully on the skin and can hasten the recovery process. You can add a tablespoon or two of apple cider vinegar to your child’s bath and let them soak in it for 10 minutes. Alternatively, use cotton to dab vinegar on the bumps twice a day.
Cassie, a mom of three from the US, used apple cider vinegar to treat Molluscum Contagiosum bumps on her children’s skin. Sharing her experience, she says, “Two of my children had Molluscum Contagiosum. For the first one, I used apple cider vinegar with tea tree oil and coconut oil, and it worked. Years later, when my third baby got it, we used only diluted ACV to dry them out. We noticed once they are dry, they start healing pretty quickly. So, trying to dry them out is the best (ii).”
9. Australian lemon myrtle
A study has revealed that Australian lemon myrtle can significantly reduce the number of lesions caused due to molluscum contagiosum (18). It also eliminates dead cells and helps in generating new skin cells. To get rid of the lumps, mix a spoonful of lemon myrtle with olive oil and create a fine mix. Apply it on the affected area every day.
10. Baking soda
Baking soda has antimicrobial properties, which makes it a natural remedy to fight molluscum contagiosum. Applying baking soda for a few minutes every day, on the infected area, can help ease the condition.
- Mix some baking soda in a cup of warm water and make a fine paste.
- Apply the paste on the infected part of the skin.
- You can do this 15-20 minutes before bath time and then wash it off.
11. Catechu
Catechu is a wood extract that has been used to treat several conditions, including asthma, cough, and skin lesions (19). It may be used in molluscum contagiosum treatment as well. You can mix catechu powder in water and apply the paste on the lumps. Let the paste dry before washing it off the skin.
12. Elderberry extract
Elderberry contains immunity-boosting compounds (20). You can try the elderberry extracts available in the form of syrups. Elderberry extract can also be applied topically, as you would apple cider vinegar or tea tree oil.
In addition to these natural remedies, you can also try these home remedies for molluscum contagiosum bumps to get relief.
- Use an astringent topically to treat the condition. You can use cotton to apply a chemical astringent (they are safe, unlike popular belief) on the infected area.
- If you do not want to pinch or puncture the lumps, you can use duct tape to remove the bumps. Before your kid goes to bed, put duct tape on the lumps and remove it the next morning. You’ll find the lumps coming off with it. However, this could be painful for your child.
- You can also directly apply iodine on the affected area to prevent bacteria from spreading the infection.
- Giving your child safe vitamin supplements, rich in vitamins A and E, will improve their immunity and enable them to fight the virus better.
- A colloidal oatmeal bath can be a good idea when your child has molluscum contagiosum.
Prevention Of Molluscum Contagiosum In Children
Parents can observe certain practices and teach their children some habits, which could reduce the chances of the child contracting molluscum contagiosum (7).
- If your child has the infection, ensure they do not scratch or pinch the bump and touch other body parts with the same hand.
- Teach your child not to touch any blister on any child or adult. If a family member is infected, the child must avoid contact with the person’s clothing, bedding, and toys, in case of children.
- Encourage regular handwashing. Teach children not to share personal items and keep their nails short.
- If your child is a teenager, you may want to talk to them about how the disease can spread through sexual activity, and abstinence is the best way to prevent it.
Frequently Asked Questions
1. Can I get molluscum contagiosum from my child?
Although it is not common, molluscum contagiosum can also affect adults. Therefore, you are likely to get the infection from your child.
2. Who is at risk of getting molluscum contagiosum?
While anyone can get infected with the molluscum contagiosum virus, children aged between one and ten are more vulnerable. Adolescents with an active sex life, immunocompromised people, and those with illnesses are at a higher risk of getting infected than other, healthy individuals.
3. Can my child get molluscum again?
Once molluscum contagiosum is treated in a child, the virus is gone from the body and the possibility of recurrence may be minimal. However, if your child comes in contact with the infecting virus from another child or a surface, they may develop the condition again (1).
4. What cream is best for molluscum contagiosum?
According to research, podophyllotoxin cream may be effective for the treatment of molluscum contagiosum. Discuss the directions for usage with your doctor (21).
5. Does Vaseline help with molluscum?
Molluscum lumps may leave marks or scars if infected by bacteria, leading to pigmentation. To reduce or control them, petroleum jelly, such as Vaseline, may be used (22).
Molluscum contagiosum in children is a viral skin infection and, like most other viral infections, may be mildly contagious. Your child might be cranky due to the irritation caused by the tiny skin bumps caused by this infection. However, it is not accompanied by pain or fever. Most diagnosis is made based on clinical appearance, and the doctor may at times send a skin sample for biopsy. While the condition usually resolves by itself, a pediatrician may prescribe some medicines for your child. You can also try some home remedies under your healthcare provider’s guidance for molluscum contagiosum treatment in children.
Infographic: What Are The Long-Term Effects Of Molluscum Contagiosum?
Molluscum contagiosum rarely causes complications. Infected people can have the virus until the skin lesions are present. You may treat and remove the skin growths or let it cure naturally over time. Go through this infographic to know the long-term effects of molluscum contagiosum and make the right treatment decisions. Illustration: Momjunction Design Team
Illustration: Molluscum Contagiosum In Children: Signs Causes & Treatment

Image: Stable Diffusion/MomJunction Design Team
Learn about Molluscum Contagiosum, a common skin condition in children. Watch this interesting and informative video to discover more about how it spreads, what are its symptoms, and its treatments.
Personal Experience: Sources
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Baby Molluscum Contagiosum;https://abutcherandabaker.wordpress.com/2018/11/30/manage-baby-molluscum-contagiosum/
ii. Molluscum Contagiosum: How to cure it Naturally with Apple Cider Vinegar.
https://www.youtube.com/watch?v=pR8sU9-mC7k
References
- About Molluscum Contagiosum.
https://www.cdc.gov/molluscum-contagiosum/about/index.html - Chia-Ling Yu et al.; (2023); Interventions for molluscum contagiosum: A systematic review and network meta-analysis with normalized entropy assessment.
https://www.jaad.org/article/S0190-9622%2822%2902349-0/fulltext - Molluscum Contagiosum in Children: Symptoms, Treatment & Prevention.
https://www.healthychildren.org/English/health-issues/conditions/skin/Pages/Molluscum-Contagiosum.aspx - Molluscum.
https://www.rch.org.au/kidsinfo/fact_sheets/molluscum/ - What to Do When My Child (or a Kid in Their Class) Has Molluscum Contagiosum.
https://health.clevelandclinic.org/what-to-do-when-a-my-child-or-a-kid-in-their-class-has-molluscum-contagiosum - Maria Bandeira de Melo Paiva Seize et al., (2011); A study of the correlation between molluscum contagiosum and atopic dermatitis in children.
https://pubmed.ncbi.nlm.nih.gov/21987130/ - Molluscum contagiosum.
https://dermnetnz.org/topics/molluscum-contagiosum - Shivani S. Ambardekar et al.; (2024); Evaluating the Role of Topical Immunomodulators for Molluscum Contagiosum: A Review.
https://opendermatologyjournal.com/VOLUME/18/ELOCATOR/e18743722340545/FULLTEXT/ - Molluscum Contagiosum: Diagnosis And Treatment.
https://www.aad.org/public/diseases/a-z/molluscum-contagiosum-treatment - Safely Treating Molluscum, a Common Skin Condition.
https://www.fda.gov/consumers/consumer-updates/safely-treating-molluscum-common-skin-condition - Makoto Kawashima et al.; (2024); The safety and tolerability of berdazimer gel 10.3% in Japanese patients with molluscum contagiosum.
https://pubmed.ncbi.nlm.nih.gov/39553484/ - Peyman Mikaili et al., (2013); Therapeutic Uses and Pharmacological Properties of Garlic, Shallot, and Their Biologically Active Compounds.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3874089/ - Joanna Wallengren; (2011); Tea tree oil attenuates experimental contact dermatitis.
https://pubmed.ncbi.nlm.nih.gov/20865268/ - Lindsey K. Elmore; (2014); Treatment of Dermal Infections With Topical Coconut Oil.
https://www.naturalmedicinejournal.com/journal/treatment-dermal-infections-topical-coconut-oil - Marta Radzimierska-Kaźmierczak et al.; (2021); Olive Oil with Ozone-Modified Properties and Its Application.
https://pubmed.ncbi.nlm.nih.gov/34063952/ - Skin infections – bleach baths.
https://www.rch.org.au/kidsinfo/fact_sheets/skin_infections_bleach_baths/ - Hima Gopinath and Kaliaperumal Karthikeyan; (2021); Neem in Dermatology: Shedding Light on the Traditional Panacea.
https://pmc.ncbi.nlm.nih.gov/articles/PMC8906293/ - Briant E Burke et al., (2004); Essential oil of Australian lemon myrtle (Backhousia citriodora) in the treatment of molluscum contagiosum in children.
https://pubmed.ncbi.nlm.nih.gov/15183850/ - MA Sunil et al.; 2018); Immunomodulatory activities of Acacia catechu, a traditional thirst quencher of South India.
https://pubmed.ncbi.nlm.nih.gov/29502869/ - Mirela Lăcrămioara Mocanu and Sonia Amariei; (2022); Elderberries—A Source of Bioactive Compounds with Antiviral Action.
https://pubmed.ncbi.nlm.nih.gov/35336621/ - Clinical Overview of Molluscum Contagiosum.
https://www.cdc.gov/molluscum-contagiosum/hcp/clinical-overview/?CDC_AAref_Val=https://www.cdc.gov/poxvirus/molluscum-contagiosum/treatment.html - WAYS TO USE PETROLEUM JELLY FOR SKIN CARE.
https://www.aad.org/public/everyday-care/skin-care-secrets/routine/petroleum-jelly
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Mubina Agboatwalla
Read full bio of Dr. Ritika Shah
Read full bio of Swati Patwal
Read full bio of Ghazia Shah