Image: Shutterstock
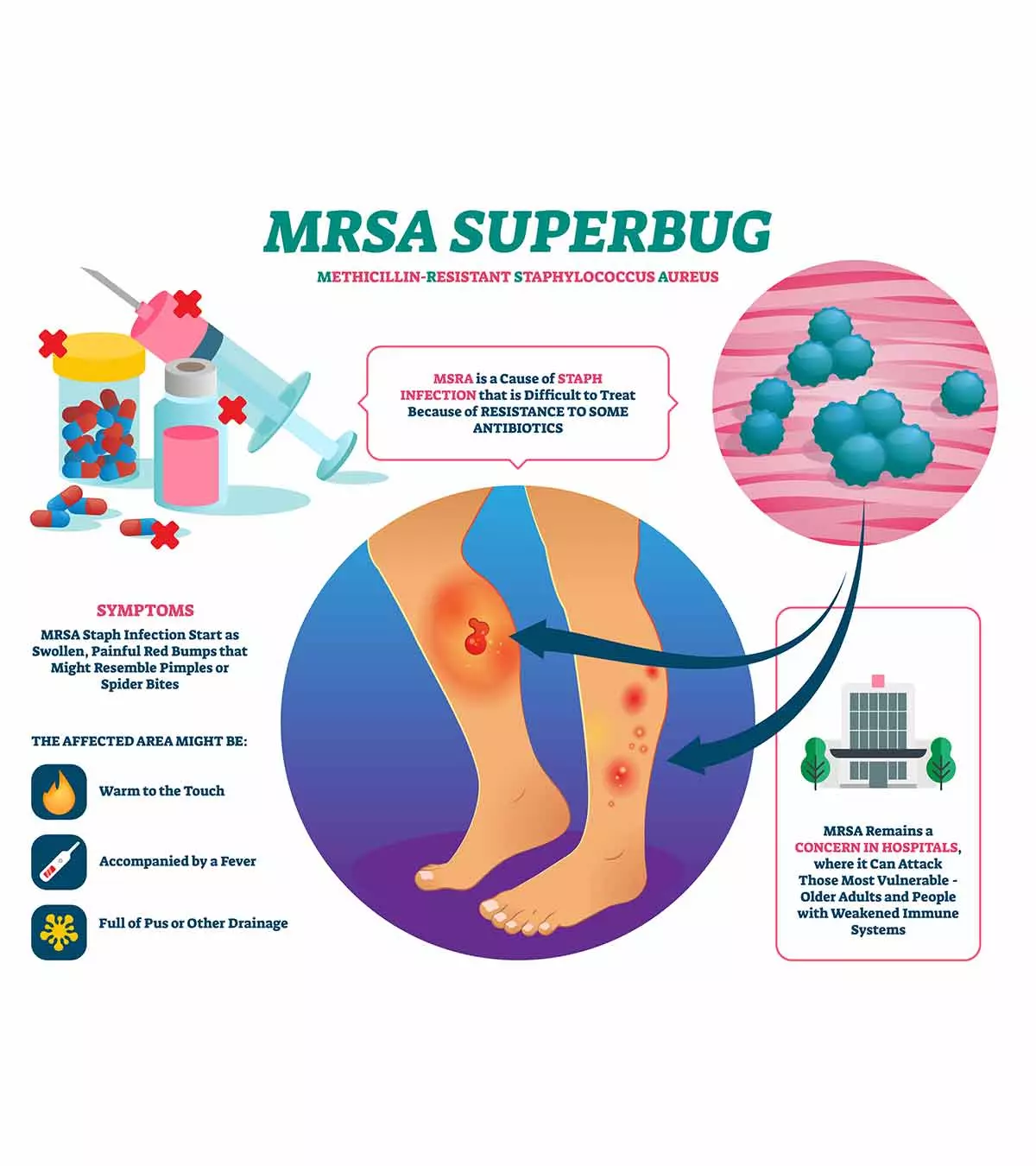
Methicillin-resistant MRSA (methicillin-resistant Staphylococcus aureus) is a genetic form of Staphylococcus aureusiCommonly found bacteria responsible for acute skin and food-borne infections. bacteria that causes significant skin infections in children due to antibiotic resistance (1). MRSA infection in children is typically hard to treat and can have life-threatening consequences since this staph bacteria is resistant to many antibiotics. Therefore, seek medical care if you suspect your child has an MRSA skin infection. Read on to know more about MRSA skin infection in children, including its causes, risk factors, symptoms, complications, diagnosis, treatment, and prevention strategies.

Key Pointers
- MRSA is a contagious bacterial skin infection that causes sores, pus-filled boils, and red bumps.
- It is diagnosed by performing swab tests, blood tests, and blood culture.
- MRSA could lead to serious complications if not treated on time.
- The treatment for MRSA includes the administration of antibiotics.
Causes Of MRSA Infections In Children
MRSA bacteria can be present on the skin and in the nasal passages of many people but may not cause diseases. The bacteria may cause infection if there is a cut or wound on the skin or the child’s immune system weakens (2).
Previously, MRSA was a nosocomial (hospital-acquired infection) bacterial infection. However, these days, it is generally considered a community-acquired infection–One in three people (33%) carries S. aureus bacteria, and two in 100 people carry MRSA on the skin without knowing it (3). The risk of an MRSA infection, a type of staph infection, is higher outside healthcare settings (4).
MRSA is contagious through skin-to-skin contact. Touching, sneezing, and coughing are significant sources of how children get MRSA infection (5). Poor hand hygiene and not following cough etiquette increase the risk of transmission of the bacteria.
Sara Lee South, a mother of three, shares the story of how her son Axel contracted MRSA. She says, “Axel, trying to help her (their dog), grabbed her, and she nipped at his finger because she was hurt. Her little sharp puppy teeth went right down into his finger joint, shoving the bacteria. That day, it didn’t seem too bad. We rinsed it, squeezed the blood, and mostly forgot about it. The next day, he woke up during the night and said, ‘Oh, my finger hurts so bad,’ which started to clue us in that something might be going on.
“Toward the evening, his finger started looking pretty gnarly, swollen, and weird; I noticed a little pink line running up his arm. His symptoms started shifting quickly; he started to say in the car, ‘I’m not feeling good; my brain feels foggy and some different things.’ I thought it was sepsis, so I immediately called the paramedics, and they met us close by. He (the paramedic) said, ‘I don’t think you need to go in an ambulance; go straight to the hospital, and you need to get antibiotics pretty quick because it is infected.’ We got to the emergency room, and they told us, ‘This is bad; we need to get him on IV antibiotics.’ After a few days, his finger was hugely blistered and bubbled. They (the healthcare team) had taken initial cultures, which came back, and the results showed that he had MRSA (i).”
 Quick fact
Quick factRisk Factors And Complications Of MRSA Infection In Children
The following factors may increase the risk of MRSA infection in children (2).
- Skin injuries
- Piercing

- Tattooing
- Previous MRSA infection
The chances of an outbreak of MRSA infection can often be high in certain population groups, such as children in daycare centers and schools (6). Those from a sports team or peer group are also at increased risk since they may share sports equipment or clothing, and skin-to-skin contact is high (7).
The possible complications of MRSA infection in an untreated child may include the following (1).
- Bacteria may damage nearby tissues.
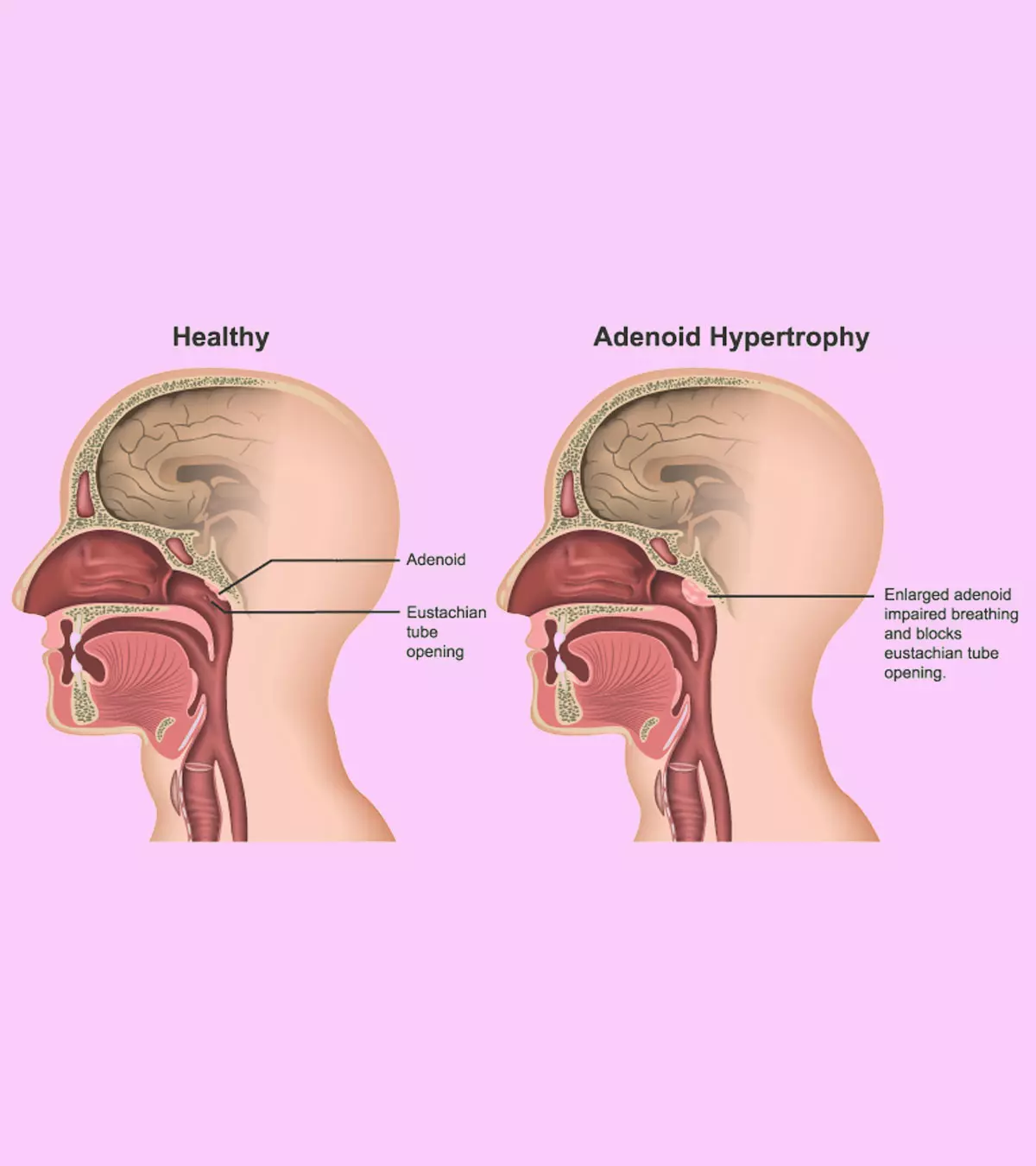
- MRSA may cause fatal complications, such as sepsis (blood infection), septic shockiA severe complication of an infection where a person’s blood pressure drops to dangerously low levels. , pneumonia, necrotizing fasciitisiA potentially life-threatening bacterial infection causing rapid and progressive destruction of the body’s soft tissues. osteomyelitis (bone infection), or endocarditis (heart infection).
- Bacteremia and associated complications. According to the American Academy of Pediatrics (AAP), “ Each additional day of bacteremia was associated with a 50% increased odds of bacteremia-related complications (8).”
Signs And Symptoms Of MRSA Infection In Children
Skin infection is the most common form of MRSA infection in children. Open wounds such as scrapes or simple cuts, primarily on the legs and buttocks, can be infected with MRSA.
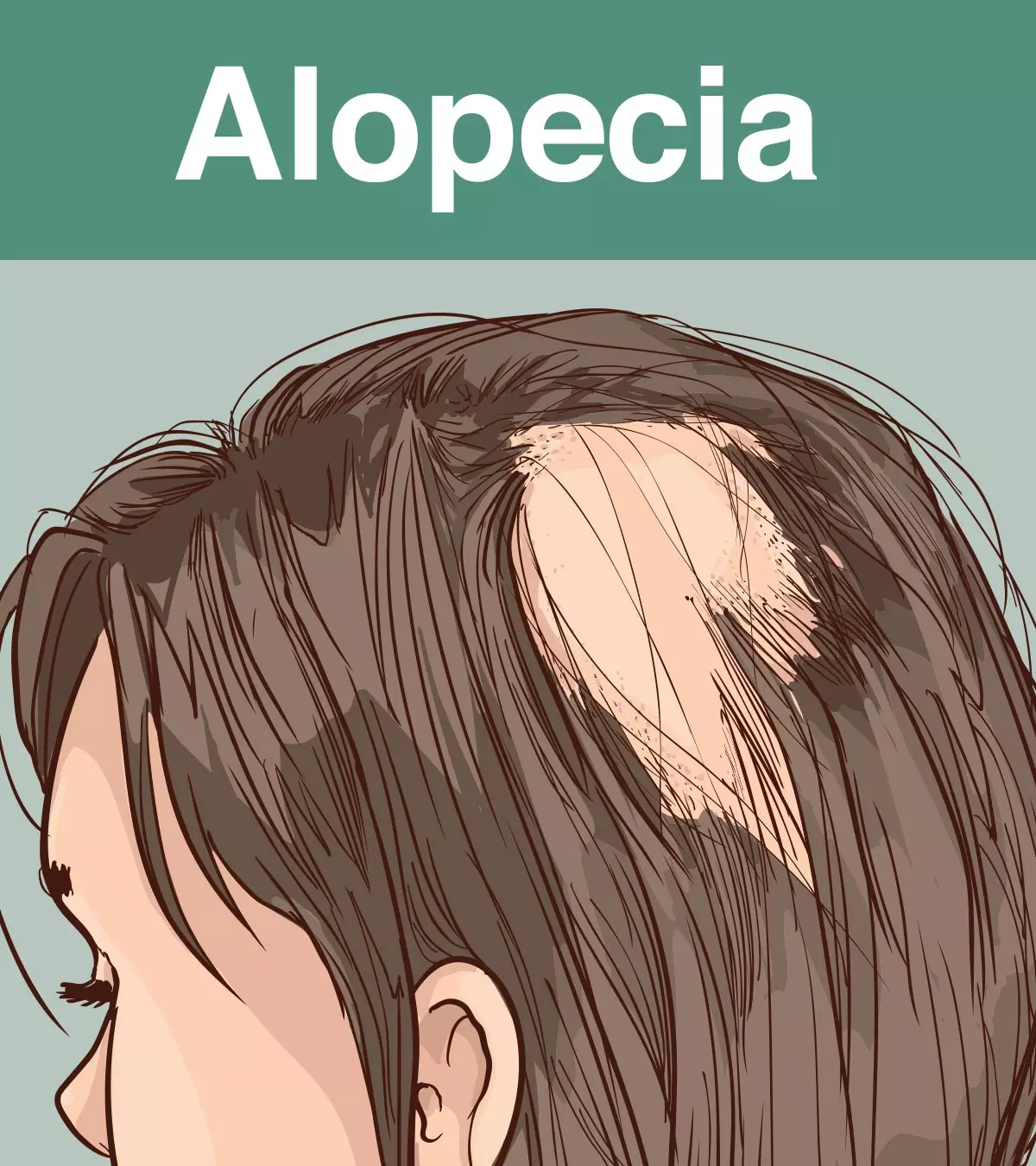
The MRSA skin infection may look like any of the following (9).
- Bump on the skin that may seem like a pimple, spider bite (blackened center), or a boil
- Red bumps with swelling and fluid leak
- Warm or hot skin around the sore
- Painful sores
- Pus-filled spots or boils
- Boils leaking pus
Note:
Always wash your hands with soap and water after touching the infected area of your child’s skin.
MRSA infection’s other signs and symptoms may vary depending on the severity and affected organ or part of the body. The common signs and symptoms seen in MRSA infection may include (2):
- Fever
- Chills

- Headache
- Dizziness
- Drowsiness
- Swollen lymph nodes near the infected area
These symptoms can be seen in other diseases too. Seek medical care if you are unsure about the signs of MRSA infection.
When To See A Doctor
Seek medical care if your child has MRSA infection symptoms since the infection may become severe in a short duration if left untreated.
You may also inform the doctor if the infection does not heal or worsens during the treatment. Self-treatments are not recommended for MRSA infection due to its spread and complications.
Diagnosis Of MRSA Infection In Children
Symptoms, medical history, and physical examinations are helpful in the diagnosis of MRSA infection. Usually, the bacteria are identified from a skin swab. Based on the child’s symptoms, pediatricians may order additional tests to diagnose possible complications. The tests may include blood tests, chest X-rays, echocardiogram, and cultures of samples from blood, sputum, fluid from the sores (9).
Early diagnosis and treatment could help prevent morbidities and life-threatening complications of MRSA infection.
- Skin swab
- Blood tests and blood culture

- Sputum cultureiExamination of sputum (thick liquid comprising mucus and saliva) for any potential microbial infections in the lungs or airways.
- Culture of fluid from the sores
- Chest X-ray
- Echocardiogram
Pediatricians may order diagnostic tests based on the symptoms and signs of your child. Early diagnosis and treatment could help prevent morbidities and life-threatening complications of MRSA infection.
Treatment For MRSA Infection In Children
Treatment for MRSA infection depends on the symptoms, severity of the disease, age, and health status of your child. The following treatments are given for MRSA infection in children (10).
- Mild skin infections or skin abscesses are opened to drain the pus. You may have to keep the wound clean and covered as directed by the doctor. Doctors may prescribe antibiotic oral medication and ointments for more effective treatment.
- Hospitalization and IV antibiotics treatments are needed for MRSA infection that has spread to other parts of the body
- Joint infection may be treated with surgery to drain the infected fluid from the joints.
- Bathing in diluted bleach or antibacterial-treated water is recommended for recurrent MRSA skin infections. You may use half a cup of bleach in a bathtub that is one-fourth full of water.
- Antibiotic soaps, such as those with chlorhexidine, may be needed for recurrent infections
- Antibiotic medicines may be given for application in nasal passages where MRSA usually resides.
It is essential to take antibiotic medications on time and complete the prescribed course, even if the signs and symptoms disappear and your child feels well. In most cases, the infection resolves within a week of antibiotic treatment, and you may make a follow-up visit to evaluate the condition.
Prevention Of MRSA Infection In Children
Teaching the following habits to your child can decrease the risk of MRSA infection and many other infectious diseases (11) (12) (13).
- Wash hands with soap and water or use a sanitizer.
- Keep wounds clean by applying bandages.

- Do not scratch wounds and sores.
- Avoid sharing personal items such as toothbrushes, towels, and soaps.
- Do not touch sores on self or anyone.
- Disinfect toys, mats, and high-contact surfaces regularly.
- Do not participate in contact sports with an open or bleeding wound.
- Shower after sports practice or competitions.
- Disinfect sports equipment.
- Wash sports clothes and uniforms after each use.
- Check your child’s skin regularly for redness, swelling, or pus-filled sores, which may indicate an early MRSA infection.
 Point to consider
Point to considerYou may also ensure hygienic measures in highly crowded areas, such as schools, daycares, and sports facilities. It is also essential to inform teachers or coaches if your child has an MRSA infection to prevent the spread of the disease. Also, educate your child about personal hygiene, such as frequent handwashing and avoiding sharing personal belongings.
Frequently Asked Questions
1. Is it common for kids to get MRSA?
Surveys show that up to 30% of children in US classrooms have MRSA either on their skin or in their noses. However, most children who are carriers of the bacteria do not develop the infection symptoms (5).
2. Is it okay to be around someone with MRSA?
It is usually okay to be around someone with MRSA as it may not affect healthy people, including pregnant women, children, and babies. However, sick people with long-term skin conditions such as eczema or open wounds may be vulnerable to the infection (15).
3. Which antibiotics may be prescribed to children with MRSA?
Children with minor skin infections may be prescribed a 2% topical mupirocin cream. Vancomycin may be prescribed in hospitalized children. Clindamycin or linezolid may be given orally or intravenously, depending on the child’s age. Tetracyclines are not used for children below eight years (10).
4. Can my child with MRSA attend school?
Children with MRSA skin infection symptoms may attend school if (5):
- The infected areas have been properly bandaged and the wound dressing is sufficient to contain all round drainage without needing a change.
- The child can follow hand and personal hygiene.
- The child is not using whirlpools or swimming pools or participating in contact sports or activities that may loosen the bandages.
5. If someone gets MRSA, will it recur?
Most people do not have an active infection after treatment, but there are cases of repeated infections as well. Consult your doctor if you suspect that your child’s infection recurs (5).
6. What other diseases can be mistaken for MRSA?
Spider bites, cellulitis, and impetigo might be mistaken for MRSA due to the similarities in clinical features (16).
7. Can a bug bite turn into MRSA?
MRSA bacteria can enter the body through bites, cuts, burn, or scrapes so yes, a bug bite could turn into an MRSA infection (16).
8. Is MRSA the same as sepsis?
No, but if left untreated, MRSA may cause sepsis which is the body’s response to an infection that can lead to tissue damage, organ failure, and even death (17) (4).
9. What are the chances of surviving an MRSA infection?
In the US, 10 to 30 percent of MRSA patients succumb to the disease. However, as per a study conducted in 2017, only 2 percent of children infected with MRSA died (18).
10. Will MRSA go away on its own?
It is possible that MRSA will go away on its own, however, seek medical advice if you think your child has MRSA symptoms because the infection can become severe in a short span of time if left untreated (19).
MRSA infection in children can lead to significant skin lesions since the bacteria is resistant to usual antibiotic treatments. It is a type of staph infection in kids that can spread in daycares or peer groups through shared personal items or direct contact. Cultures from skin lesions help to diagnose MRSA infections. Oral and topical antibiotics are also prescribed for mild MRSA skin lesions. Severe MRSA infections require intravenous antibiotics and joint infections require surgical fluid drainage. Maintaining hand hygiene and not sharing personal items may prevent the spread. It is recommended to visit a pediatrician since OTC medications and home remedies may not cure MRSA infections.
Infographic: Impact Of Decolonization In Pediatric MRSA
Some children may be exposed to MRSA during a hospital stay or due to close contact with a person with an active MRSA infection. Decolonization is a process of reducing the bacterial load to lower the intensity of active infection or prevent its further transmission. The infographic below provides some notable points about it.
Some thing wrong with infographic shortcode. please verify shortcode syntax
Watch a pediatric expert explain about how to protect your child from MRSA Staph infections. Get tips on prevention, diagnosis, and treatment.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Axel’s MRSA infection and hospital experience;https://www.youtube.com/watch?v=H3yFqmTvKiY&feature=youtu.be
References
- Methicillin-Resistant Staphylococcus aureus.
https://www.ncbi.nlm.nih.gov/books/NBK482221/ - MRSA Infection in Children.
https://www.stanfordchildrens.org/en/topic/default?id=mrsa-infection-in-children-160-49 - Clinical Overview of Methicillin-resistant Staphylococcus aureus (MRSA) in Healthcare Settings.
https://www.cdc.gov/mrsa/hcp/clinical-overview/index.html - Methicillin-resistant Staphylococcus aureus (MRSA) Basics.
https://www.cdc.gov/mrsa/about/index.html - MRSA and Children: Parent FAQs.
https://www.healthychildren.org/English/health-issues/conditions/infections/Pages/MRSA.aspx - Melissa B Miller et.al; (2011); Prevalence and Risk Factor Analysis for Methicillin-Resistant Staphylococcus aureus Nasal Colonization in Children Attending Child Care Centers.
https://pmc.ncbi.nlm.nih.gov/articles/PMC3067749/ - Methicillin Resistant Staphylococcus aureus (MRSA) in Schools.
https://ldh.la.gov/assets/oph/Center-PHCH/Center-CH/infectious-epi/MRSA/StaphMRSASchool.pdf - Rana F. Hamdy et.al; (2017); Epidemiology of Methicillin-Resistant Staphylococcus aureus Bacteremia in Children.
https://publications.aap.org/pediatrics/article-abstract/139/6/e20170183/38696/Epidemiology-of-Methicillin-Resistant?redirectedFrom=fulltext - Methicillin-Resistant Staphylococcus Aureus (MRSA).
https://www.stlouischildrens.org/conditions-treatments/methicillin-resistant-staphylococcus-aureus-mrsa - IDSA Guidelines on the Treatment of MRSA Infections in Adults and Children.
https://www.aafp.org/pubs/afp/issues/2011/0815/p455.html - Prevention of MRSA.
https://www.nyc.gov/site/doh/health/health-topics/mrsa-prevention.page - Methicillin Resistant Staphylococcus aureus.
https://www.childrens.health.qld.gov.au/health-a-to-z/methicillin-resistant-staphylococcus-aureus - Preventing Methicillin-resistant Staphylococcus aureus (MRSA).
https://www.cdc.gov/mrsa/prevention/index.html - MRSA.
https://kidshealth.org/en/parents/mrsa.html - MRSA.
https://www.nhs.uk/conditions/mrsa/ - What Does MRSA Look Like?
https://www.hopkinsmedicine.org/health/conditions-and-diseases/what-does-mrsa-look-like - Sepsis.
https://medlineplus.gov/sepsis.html - MRSA blood infections are less fatal in kids vs. adults but cause significant complications.
https://www.childrensnational.org/about-us/newsroom/2017/mrsa-blood-infections-are-less-fatal-in-kids-vs-adults-but-cause-significant-complications - Methicillin Resistant Staphylococcus Aureus (MRSA) Fact Sheet.
https://rmh.org/methicillin-resistant-staphylococcus-aureus-mrsa-fact-sheet
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Nikolina Zdraveska
Read full bio of Dr Bisny T. Joseph
Read full bio of Swati Patwal
Read full bio of Anindita Ghatak