Image: Shutterstock
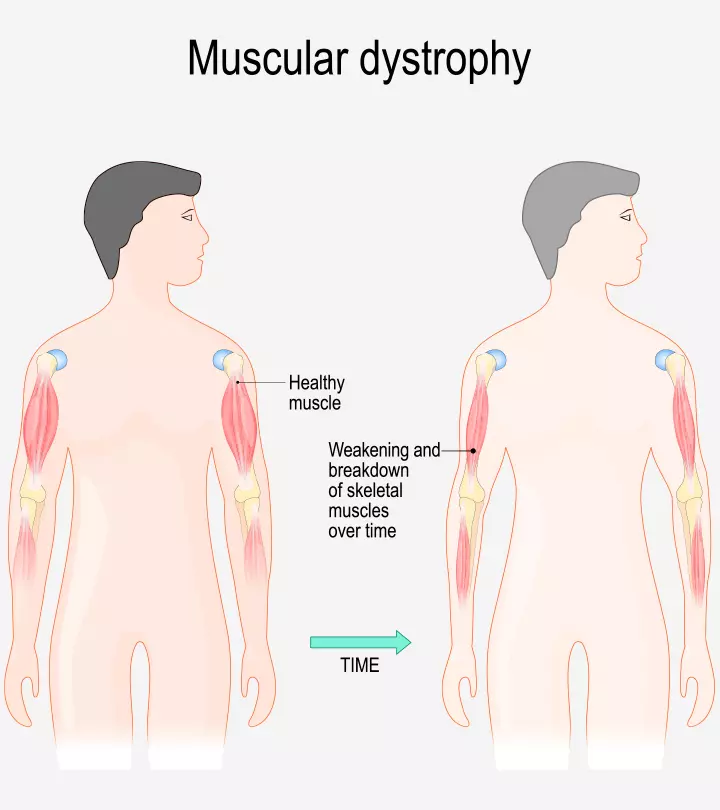
Muscular dystrophy in children is a collective name for over 30 different genetic neuromuscular disorders. Each disorder causes muscle weakness and wasting (atrophy). The progressive muscle weakness leads to difficulty in movement and loss of control (1).
Duchenne muscular dystrophy (DMD) is the most common disorder affecting young boys from three to six years (2). While there is no cure, different therapies can help lessen the severity and prevent complications.
Read about muscular dystrophy in children, including its types, causes, symptoms, and treatment.
Key Pointers
- A child with muscular dystrophy experiences muscle weakness and loss of muscle function.
- Some common types of muscular dystrophy include Duchenne muscular dystrophy (DMD) and Becker muscular dystrophy (BMD).
- It is caused by gene mutations and deletions, which affect the proteins of the muscles.
- Physical and occupational therapies, supportive devices, and medications could help manage the condition.
What Causes Muscular Dystrophy In Children?
Muscular dystrophy could result from a mutated gene that affects proteins in the muscles. It further prevents the proteins from working accurately and efficiently. Different dystrophies occur from various mutations. The mutated genes are inherited from the parents, but in some cases, the mutation can occur spontaneously and pass to future generations (3).
What Are The Types And Symptoms Of Muscular Dystrophy In Children?
Several types of muscular dystrophy can occur during childhood and adulthood. Here we discuss the common childhood muscular dystrophies that progress and affect muscles in various ways (4):
- Duchenne muscular dystrophy (DMD): It occurs due to a faulty gene on the X chromosome. The condition primarily affects boys and is seen in around 50% of people with muscular dystrophy (3) (5). This disability affects children from three to six years.
Symptoms include
- Difficulty in standing up from a sitting or lying position
- Wobbly walk
- Problem in jumping and running
- Falling frequently
- Swollen calf muscles (3)
 Things to know
Things to know- Becker muscular dystrophy: This condition is due to the mutation in the DMD gene responsible for the production of dystrophin proteiniA protein found in muscles connecting the interior of the cells to the outside matrix and strengthening and protecting the muscles. for maintaining the muscle (6). It may occur during early adulthood. Similar to DMD, it is more common in males. According to the final population-based study from the Centres for Disease Control and Prevention (CDC) research network (MD STARnet), it was observed that among 1,164 males with DBMD, the prevalence of the disease throughout a five-year period among males aged 5 to 9 ranged from 1.92 to 2.48 per 10,000.

Symptoms include
- Falling frequently
- Walking on tiptoes
- Frequent muscle cramps
- Late appearance of symptoms than DMD (3)
Brad, a blogger who has been dealing with Becker Muscular Dystrophy since childhood, recollects how he learned its symptoms and diagnosis. “I was just ten years old and was first diagnosed with Becker’s Muscular Dystrophy. You see, in the years before my diagnosis, my parents had me join the local soccer team, and it didn’t take long for them to notice that I was having some issues keeping up with other children my age. I was struggling, having issues running from one end of the field to another; I just could not keep up (i).”
- Congenital muscular dystrophy (CMD): It develops at birth with an incidence of fewer than three cases in 100,000 births. CMD is believed to occur due to genetic mutations (7).
Symptoms include
- Weakness along with weak muscle tone (hypotonia) at birth
- Delay in walking
- Limp or floppy baby
- Poor head and neck control
In addition to hypotonia and delayed milestones, children with CMD may also exhibit joint contractures and skeletal deformities at birth, which can significantly impact their motor development and require early intervention.
- Emery-Dreifuss muscular dystrophy (EDMD): It is rare, with the X-linked defect occurring in around one out of 100,000 people (8). It can occur at any age between childhood to early teenage.
Symptoms include
- Stiffness of the spine
- Weakening of muscles from the upper arms and lower legs
- Loss of movement in the elbows, knees, spine, ankles, and back of the neck
- Locking of elbows in a bending position (3)
- Facioscapulohumeral muscular dystrophy: It occurs due to deletion of genetic material from a specific region of the DNA. The deleted gene is passed on in the form of autosomal dominant inheritance, where the missing DNA base pair is enough to cause the disease (9). This muscular dystrophy can affect people in their childhood or early adulthood.
Symptoms include
- Difficulty in hearing, talking, swallowing, and chewing
- Sloped shoulders or winged shoulder blades
- Muscle weakening around the mouth and eyes
- Curved spine (3)
- Limb-girdle muscular dystrophy (LGMD): Resulting from mutations in several genes, LGMD affects around one in 14,500 to one in 123,000 people (10). It mostly occurs in people during their late childhood or middle age.
Symptoms include
- Stiffness of the spine
- Wobbly walk
- Falling frequently
- Muscle weakening around the hips spreading through the neck, shoulders, and legs (3)
What Are The Complications of Muscular Dystrophy?

Muscular dystrophy can impact the muscles, heart, and lungs, leading to complications such as (11):
- Respiratory tract infections, such as pneumonia
- Breathing difficulty or choking
- Heart disorders, including arrhythmiasiA condition of irregular heartbeat that may cause dizziness, shortness of breath, and fatigue. and heart failure
How Is Muscular Dystrophy Diagnosed In Children?
Diagnosis of muscular dystrophy in children involves the following tests (2) (12):
- Genetic test: This is performed to confirm if the cause behind the dystrophy is a genetic mutation.
- Blood test: A blood test can detect the presence of creatine kinase enzyme. High levels of the enzyme will indicate a muscle disorder.

- Muscle biopsy: A confirmatory primary test, where a small portion of the muscle is examined under the microscope to look for changes in the muscle tissue to see if the disease is degenerative.
- Electromyogram (EMG): This test is carried out to determine if the muscle weakness is due to destroyed muscle tissue rather than a nerve disorder.
- Electrocardiogram (ECG or EKG): The test monitors the heart’s electrical activity for detecting any abnormalities in the heart rhythm or heart muscle damage.
Early diagnosis is crucial as it allows for timely intervention and management strategies that can improve quality of life. Parents should be aware of the importance of seeking medical advice if they observe symptoms, especially in families with a history of muscular dystrophy.
How Is Muscular Dystrophy Treated In Children?

Currently, there is no cure for muscular dystrophy. However, the following management therapies, rehabilitation, and treatments are recommended depending on the type of muscular dystrophy, age of the child, and the extent of the condition.
- Physical and occupational therapy: This could help the muscles function and prevent the joints from becoming stiff. Through the therapy, the child will be assisted with orthoticsiAlso known as shoe inserts, or arch support, they are designed to support the feet and help correct certain deformities. to improve their walk and maintain their balance (13).
- Supportive devices: Assistive devices, such as wheelchairs, braces or splints offer protection, support, and prevent deformity (12). Patients with weakened lungs may require assisted ventilation to ease the breathing during the nighttime (13).
- Medications: Oral corticosteroids are administered to help the children with some muscular dystrophies walk for longer durations (14).
- Some other management therapies include nutritional counseling, speech therapy, psychological counseling, respiratory therapy and breathing exercises to improve quality of life.
Surgical interventions
are also recommended to manage some conditions (12) (13):
- Scoliosis surgery for correction of curved backbones and improvement of breathing.
- Muscle-release surgery to treat muscle contractures and increase mobility.
Furthermore, recent advancements in research are exploring gene therapy and exon skipping as potential treatments for specific types of muscular dystrophy, particularly Duchenne muscular dystrophy. These innovative approaches aim to correct or compensate for the genetic defects responsible for the condition and represent a hopeful area of ongoing clinical trials.
 ”The
”TheCan Muscular Dystrophy Be Prevented?

Muscular dystrophy is a genetic disease and cannot be prevented. However, in case of a family history of muscular dystrophy, parents can get tested to know if they are carriers and plan accordingly.
What Is The Life Expectancy Of A Child With Muscular Dystrophy?
The life expectancy depends on the type of muscular dystrophy the child develops:
- Duchenne: The child might live beyond 30 years and even marry and have children (15).
- Becker: The child has an average life expectancy of 40 years (16).
- Congenital: This type has a poor prognosis, with most children not surviving up to adolescence (17).
- Emery-Dreifuss: Children may develop heart-related problems anytime between ten and 19 years with EDMD (18).
- Facioscapulohumeral: The prognosis looks good with a life span of several decades of onset (4).
Frequently Asked Questions
1. Is muscular dystrophy fatal in children?
According to the NHS, in some cases, muscular dystrophy may severely affect the heart and lung muscles, making it a serious condition (19). In addition, some types of muscular dystrophy, such as Duchenne muscular dystrophy (DMD), may be fatal, especially in the pediatric male population (14).
2. How does muscular dystrophy affect a child’s learning capabilities?
Reports suggest that around one-third of children with a progressive type of Duchenne muscular dystrophy may experience behavioral and learning difficulties and require additional support to meet their learning needs (20).
3. What are some resources available for families of children with muscular dystrophy, such as support groups and advocacy organizations?
Muscular Dystrophy Association, National Muscular Dystrophy Society, Parent Project Muscular Dystrophy, and The Muscular Dystrophy Family Foundation are some of the renowned non-profit organizations in the US that provide varied assistance to individuals with muscular dystrophy.
4. What are the latest developments in research on muscular dystrophy in children, and what do they suggest for the future of treatment and management?
Research is ongoing to find a treatment for muscular dystrophy. Scientists are hopeful that cell-based therapy, gene therapy, antisense oligonucleotide, growth factor pathways, and stop codon read-through may provide new treatment options for muscular dystrophy in children (22).
Muscular dystrophy is an umbrella term for a group of genetic disorders in children affecting the muscles. Also, there is no effective cure to treat muscular dystrophy rather than managing its symptoms and improving the quality of life. You can support your child by providing the best care they require. Ensure they take medications and follow all the doctor’s instructions. Remember, with the advancing technologies and treatments, children with muscular dystrophy can go to school, college and study.
Infographic: Types Of Muscular Dystrophy In Children
Muscular dystrophy can affect a child’s muscular strength and disrupt their daily lives. However, knowing the symptoms of any muscular dystrophy can help the parents look for timely medical intervention. The following infographic states all the types of muscular dystrophy and their specific symptoms.
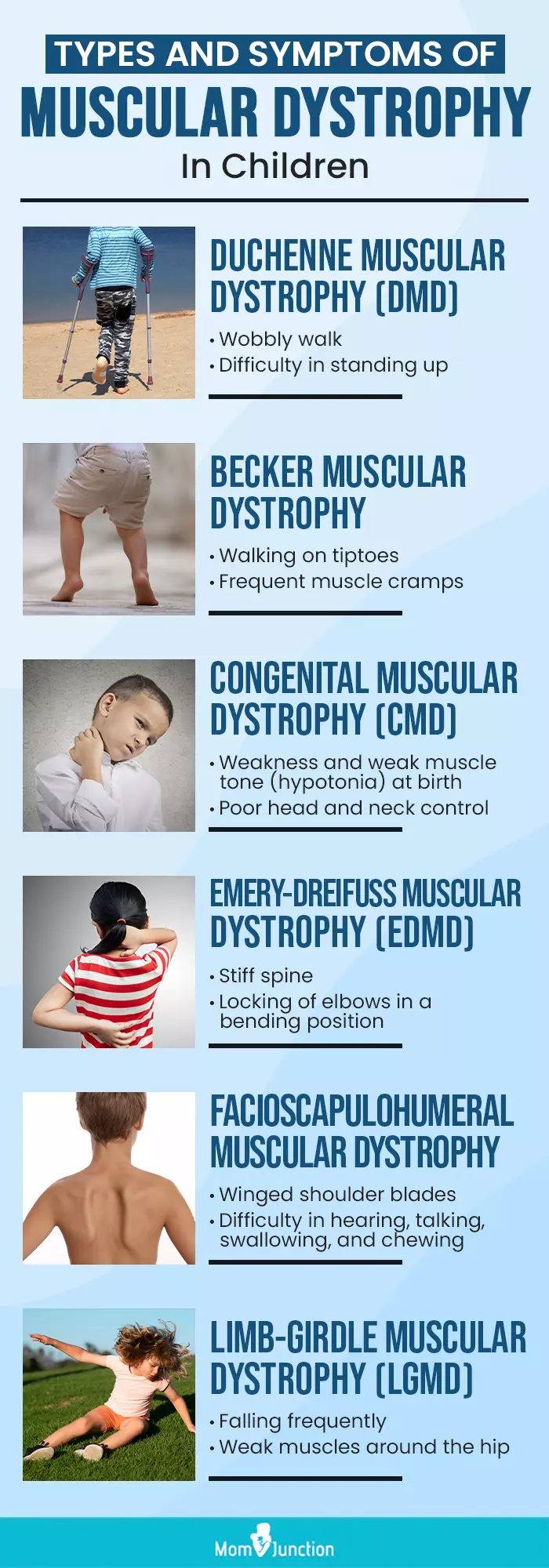
Illustration: Momjunction Design Team
Learn about the tests and outcomes of DMD, a muscle-wasting disease. Understand how to manage the condition and improve quality of life.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Living with Becker Muscular Dystrophy: Brad’s story.https://my-beckers-story.blogspot.com/2010/01/living-with-beckers-my-story.html
References
- Muscular dystrophy.
https://www.nationwidechildrens.org/conditions/muscular-dystrophy - Muscular dystrophy.
https://www.cedars-sinai.org/health-library/diseases-and-conditions/m/muscular-dystrophy.html - Muscular dystrophy.
https://www.childrenshospital.org/conditions-and-treatments/conditions/m/muscular-dystrophy - Types of Muscular Dystrophy and Neuromuscular Diseases.
https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=85&ContentID=P00792 - Muscular dystrophy.
https://www.chop.edu/conditions-diseases/muscular-dystrophy - Muscular dystrophy, becker.
https://rarediseases.org/rare-diseases/muscular-dystrophy-becker/ - Enrico Bertini et al. (2011). Congenital Muscular Dystrophies: A Brief Review.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3332154/ - Emery-Dreifuss muscular dystrophy.
https://medlineplus.gov/genetics/condition/emery-dreifuss-muscular-dystrophy/#frequency - Facioscapulohumeral muscular dystrophy.
https://rarediseases.info.nih.gov/diseases/9941/facioscapulohumeral-muscular-dystrophy/ - Limb-girdle muscular dystrophy.
https://medlineplus.gov/genetics/condition/limb-girdle-muscular-dystrophy/#inheritance - Muscular dystrophy.
https://my.clevelandclinic.org/health/diseases/14128-muscular-dystrophy - Pediatric muscular dystrophies.
https://www.childrensnational.org/get-care/health-library/muscular-dystrophies - Muscular dystrophy in children.
https://www.rush.edu/kids/conditions/muscular-dystrophy-children - Muscular dystrophy.
https://medlineplus.gov/ency/article/001190.htm - Duchenne Muscular Dystrophy (DMD).
https://www.mda.org/disease/duchenne-muscular-dystrophy - Becker Muscular Dystrophy (BMD) in Children.
https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=90&ContentID=P02771 - Congenital muscular dystrophy type 1A.
https://rarediseases.info.nih.gov/diseases/3843/congenital-muscular-dystrophy-type-1a - Emery-Dreifuss muscular dystrophy.
https://medlineplus.gov/genetics/condition/emery-dreifuss-muscular-dystrophy/ - Muscular dystrophy
https://www.nhs.uk/conditions/muscular-dystrophy/ - Muscular dystrophy campaign
https://media.gosh.nhs.uk/documents/Education_MDC_leaflet.pdf - FDA Approves Targeted Treatment for Rare Duchenne Muscular Dystrophy Mutation.
https://www.fda.gov/news-events/press-announcements/fda-approves-targeted-treatment-rare-duchenne-muscular-dystrophy-mutation-0 - Wendy K. M. Liew et al,; (2013); Recent developments in the treatment of Duchenne muscular dystrophy and spinal muscular atrophy
https://pmc.ncbi.nlm.nih.gov/articles/PMC3625012/
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Neema Shrestha
Read full bio of Aneesha Amonz
Read full bio of Dr. Ritika Shah
Read full bio of Vidya Tadapatri