
Image: Shutterstock
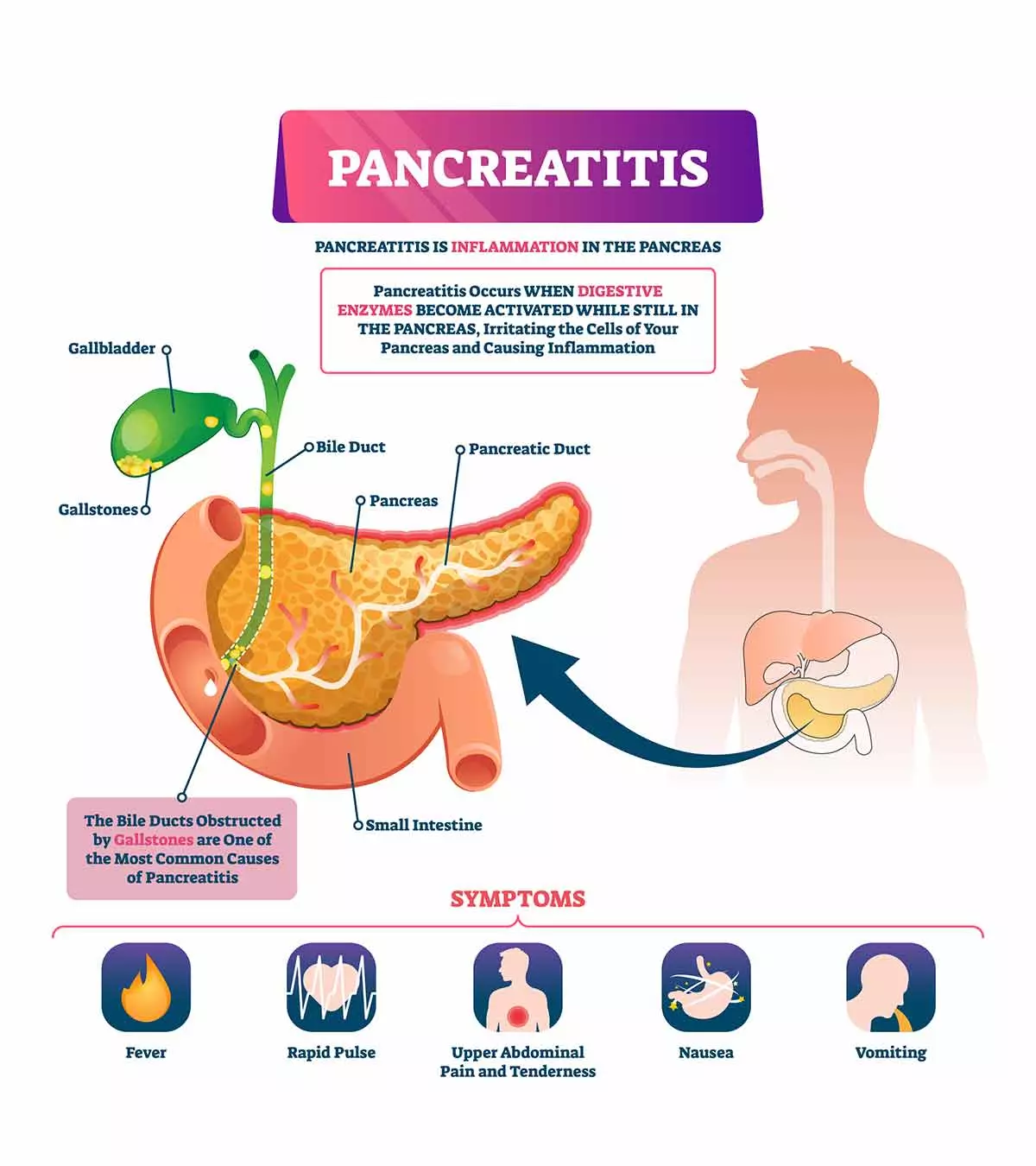
Pancreatitis in children is caused by an inflammation in the pancreas, a leaf-shaped gland located behind the stomach. The pancreas contains exocrine cells that secrete digestive enzymes and endocrine cells producing hormones, such as insulin and glucagon, which participate in glucose metabolism.
Pancreatitis can either be acute or chronic. Acute pancreatitis is a sudden and short-term inflammation of the pancreatic tissue, while chronic pancreatitis is a persistent and long-term pancreatic inflammation. Both types of pancreatitis can damage the pancreatic tissue and result in complications such as malnutrition and diabetes in children.
Read this post to learn about causes, symptoms, complications, diagnosis, treatment, and prevention of pancreatitis in children.
Signs And Symptoms Of Pancreatitis In Children
Symptoms and signs of pancreatitis may vary depending on the type. Below are the signs and symptoms of acute pancreatitis in children (1).
- Abdominal pain on the upper part of the abdomen, radiating to the backside
- A belt-like pain around the waist
- Abdominal tenderness
- Nausea
- Vomiting
- Fever
- Breathing troubles
- Rapid pulse
The following are signs and symptoms of chronic pancreatitis (1).
- Constant and intermittent abdominal pain radiating to the back for several hours or days
- Increased pain after drinking or eating foods
- Weight loss without changes in eating habits and quantity of food
- Diarrhea
- Steatorrhea (oily stools)
- Smelly stools
- Nausea and vomiting
Pancreatitis signs and symptoms can be confused with diseases such as viral gastroenteritis. You may seek medical care to determine the underlying cause.
Causes Of Pancreatitis
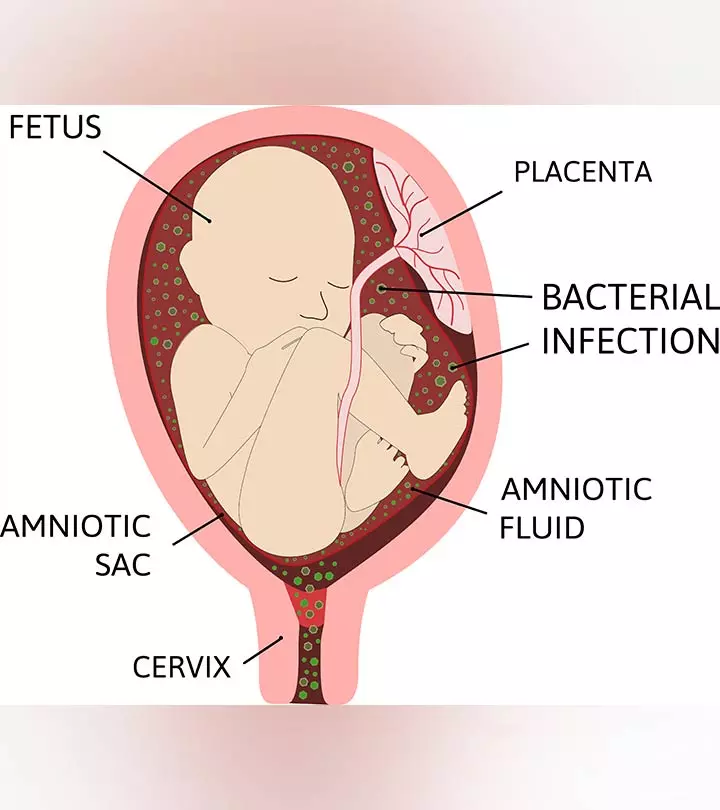
Acute or chronic pancreatitis occurs due to the autoactivation of the pancreatic enzymes as a result of various conditions or factors. These enzymes usually become activated in the intestine. If they are activated in the pancreas, they could cause inflammation and destruction of the pancreatic tissue. Some children may have idiopathic pancreatitis, which is inflammation of the pancreas due to unknown reasons.
The common causes of acute pancreatitis may include the following (2).
- Abdominal injuries, such as sports injuries, motor vehicle accidents, or fall
- Abdominal surgeries
- Acute blockage of the pancreatic duct
- Immune system attack (autoimmunity)
- Infections caused by viruses (cytomegalovirus (CMV), HIV, mumps virus, varicella-zoster virus), bacteria (salmonella, mycoplasma, leptospira), parasites (Ascaris, toxoplasma), and fungi (aspergillus)
- Gallstones
- Certain antibiotics
- Anti-seizure medications
- Chemotherapy
- Hypercalcemia (high calcium levels in the blood) due to overactive parathyroid gland (hyperparathyroidism)
- High triglycerides (a type of fat) in the blood
- Celiac disease
- Inflammatory bowel diseases (IBD), such as Crohn’s disease and ulcerative colitis
- Endoscopic retrograde cholangiopancreatography (ERCP)
- Certain types of venom, such as scorpion venom
The causes of chronic pancreatitis could be unknown in some children. Below are some of the factors and conditions that may lead to chronic pancreatitis (3).
- Recurrent or repeated episodes of acute pancreatitis
- Genetic factors
- Family history
- Autoimmunity
- Cystic fibrosis and other chronic disorders
- Blockage of pancreatic ducts or bile ducts
Exacerbation of autoimmunity or chronic diseases may cause acute pancreatitis, while long-term disorders could increase the risk of chronic pancreatitis. Also, obese children may have a higher risk of developing pancreatitis.
Complications Of Pancreatitis In Children
Acute complications
of pancreatitis may include (4):
- Dehydration
- Hyperglycemia
- Shock
- Systemic inflammatory response syndrome
- Pleural effusion
- Kidney failure
- Lung failure
The following long-term complications are often seen in children with pancreatitis (4).
- A pseudocyst, a fluid-filled, cyst-like pocket, may develop near the pancreas
- Rupture of large pseudocysts could result in complications, such as internal bleeding and infections
- Necrosis of the pancreatic tissue due to infection
- Malnutrition due to lack of enzymes to break down the foods
- Diabetes due to damaged beta cells of the pancreas
- Chronic and recurrent pancreatitis may increase the risk of pancreatic cancer
Long-term complications of pancreatitis may require special medical care and treatment. Surgical procedures are needed to drain fluid from cysts and remove any infected tissue.
Diagnosis Of Pancreatitis
The following tests are used to diagnose pancreatitis (5).
- Blood tests may show increased levels of pancreatic enzymes.
- Computerized tomography (CT) helps to visualize the pancreas and to identify gallstones. Inflammatory and destructive changes of the pancreas are seen on CT scans during pancreatitis. This may also help to evaluate the complications in some children.
- Magnetic resonance imaging (MRI) may also be used to examine the pancreas.
- Stool tests may help to identify chronic pancreatitis by measuring the amount of fat in the stool.
- Endoscopic ultrasound may help to identify bile and pancreatic duct
Pediatricians may order additional tests depending on the symptoms, causes, types, and severity of pancreatitis in your child. These tests are required to plan treatment and predict outcomes.
Treatment For Pancreatitis In Children
Treatment strategies may vary depending on the type of pancreatitis, severity, and complications. The initial interventions may include the following (6).
- Hospitalization and parenteral (intravenous) nutrition are recommended for a few days. It helps the pancreas rest and recover from the inflammation. Clear liquids (water) and bland foods are given once the pancreatitis is controlled. Your child can go back to a regular diet if there is no pain for a few days.
- Feeding tubes may be needed for children with severe pain and persistent pancreatitis to meet nutritional requirements.
- Pain medications are prescribed to manage the pain.
The underlying cause of pancreatitis is addressed once the symptoms subside. The treatment could depend on the underlying cause. Some of the common treatments include the following.
- Removal of gallstones and other causes of the pancreatic duct or bile duct obstructions to relieve inflammation.
- ERCP or endoscopic retrograde cholangiopancreatography is done to diagnose the causes as well as for treatment. However, ERCP also has a risk of causing acute pancreatitis in some individuals.
- Cholecystectomy is a surgery to remove the gallbladder if the gallstones are causing recurrent pancreatitis.
- Pancreas surgery is done to drain fluid and removed any damaged tissue.
Children with chronic pancreatitis may also require the following treatments.
- Medications and surgical or endoscopic procedures are conducted to block nerves for pain management.
- Pancreatic enzyme supplements are often prescribed to improve digestion. These enzymes help to break down the food and should be taken with each meal.
- Dietitians may prescribe dietary modifications, such as low-fat meal plans.
- The child may receive insulin supplements to prevent worsening of diabetes due to chronic pancreatitis.
Prevention Of Pancreatitis
It may not be possible to prevent all causes of pancreatitis. However, early diagnosis and management of some causes of acute pancreatitis in children could prevent the condition. A few examples include timely removal of gallstones and keeping triglycerides and blood calcium levels under check in vulnerable children (7).
Giving vaccinations on schedule may help to prevent some infectious causes. A healthy lifestyle and regular exercise can be helpful since it reduces the risk of obesity. Dietary changes, such as eating a low-fat diet and drinking plenty of water, may help to prevent pancreatic inflammation in some children.
Frequently Asked Questions
No, pancreatitis is not quite common in children. In the US, one out of every 10,000 children gets acute pancreatitis. One out of three cases is severe and has other organs affected by this condition (8). Some children may deal with pancreatitis several times, leading them to chronic pancreatitis. However, chronic conditions are rare (9).
2. Does pancreatitis go away on its own?
Yes, on most occasions, pancreatitis goes away on its own within a week. As the condition starts healing, doctors prescribe medications to treat nausea, vomiting, and pain (10).
3. How well can children recover from pancreatitis?
Most children recover well from acute pancreatitis. Sometimes, fluid may collect in and around their pancreas; however, this resolves on its own. At times, doctors may drain the fluid.
However, children with chronic pancreatitis may experience digestive issues and have to take pancreatic enzyme supplements. Some children may also develop diabetes later in their lives (10).
4. Does pancreatitis cause death in children?
Death because of acute pancreatitis is rare and occurs if multiple organs have been damaged in the child (11).
Pancreatitis in children is a condition where their pancreas gets inflamed for various reasons. As a result, a child could have constant abdominal pain and tenderness, which may also require hospitalization. If left untreated, your child could be at increased risk of hypotension and dehydration. In addition, over-the-counter medications may not relieve pancreatic pain; they could rather worsen the condition. Hence, it is important to contact a doctor immediately if you notice any symptoms of acute or chronic pancreatitis in children. Early detection and appropriate treatment interventions could help prevent the complications.
Key Pointers
- Abdominal pain, abdominal tenderness, nausea, and breathing troubles are some of the signs and symptoms of pancreatitis.
- Treatment varies depending on the type of pancreatitis, severity, and complications.
- Early diagnosis and management of some causes of acute pancreatitis in children could prevent the condition.
References
1. Pancreatitis in Children; Johns Hopkins medicine
2. Acute pancreatitis in children and adolescents; US National Library of Medicine
3. Chronic Pancreatitis; Cedars-Sinai Medical Center
4. Acute Pancreatitis; National Health Service
5. Childhood Pancreatitis; American Academy of Family Physicians
6. Chronic Pancreatitis in Children; Cincinnati Children’s Hospital
7. Acute Pancreatitis In Children; The National Pancreas Foundation
8. Acute Pancreatitis in Children; Cincinnati Children’s Hospital
9. Pancreatitis in Children; Johns Hopkins Medicine
10. Pancreatitis; KidsHealth
11. Acute Pancreatitis in Children; The National Pancreas Foundation
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Richa A Kaushal
Read full bio of Dr Bisny T. Joseph