Image: MomJunction Design Team

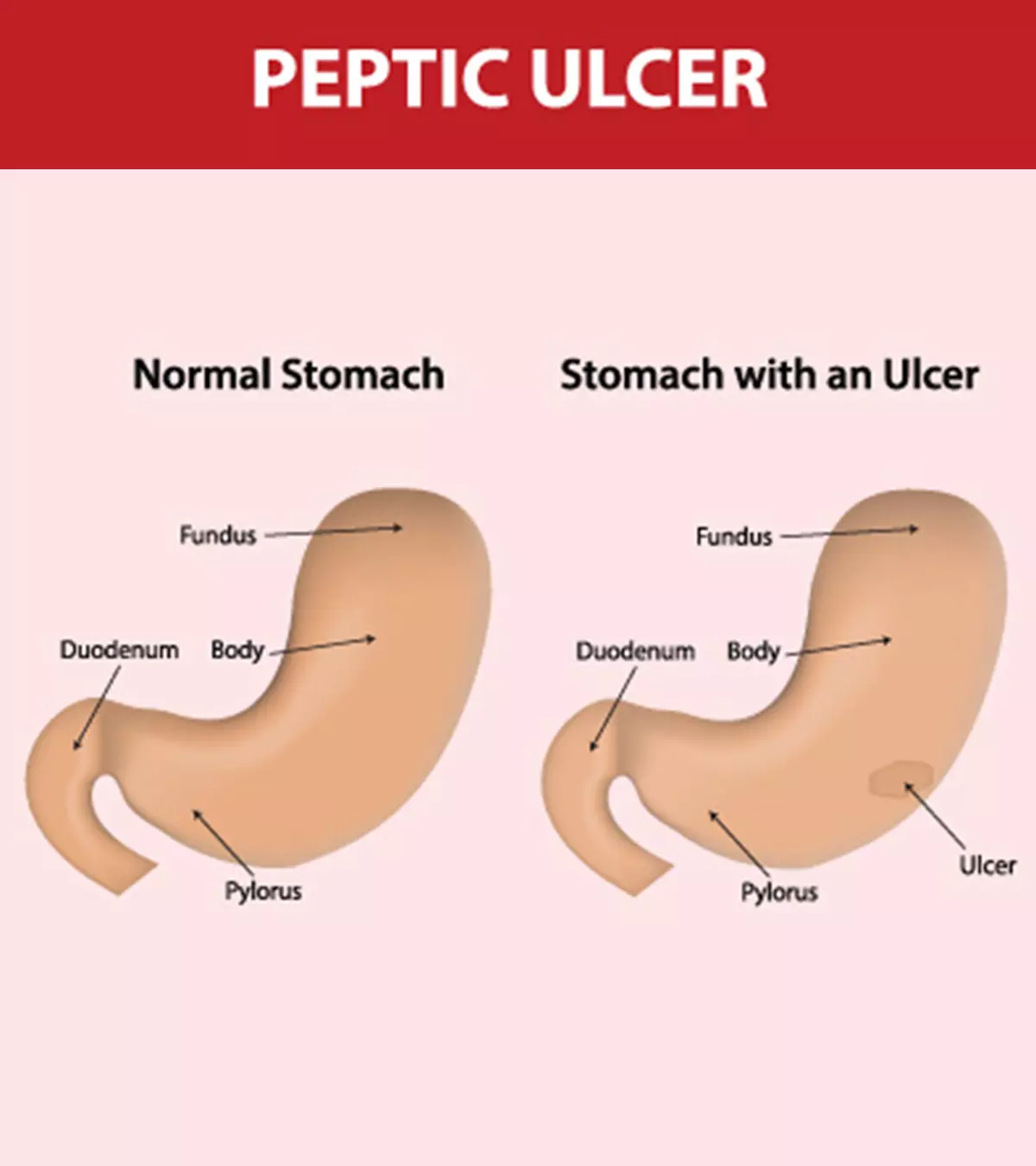
Duodenal and stomach ulcers in children are rare, and the signs and symptoms can be nonspecific. These are also called peptic ulcers that can occur in the mucosa, the inner lining of the stomach and intestines. Ulcer diets and OTC medications may not heal the ulcers since they can be caused by infection of H. pylori (Helicobacter pyloriiA pathogenic bacteria that causes chronic inflammation and ulceration in the stomach and small intestine ) bacteria. Children may require appropriate treatment, and eradicating causes can cure ulcers and avoid complications.
Read on to know the clinical features, causes, risk factors, diagnostic tests and procedures, complications, and treatments of peptic ulcers in children and ways to prevent them.
Key Pointers
- The bacterium H. pylori is the primary cause of duodenal and stomach ulcers in children.
- Factors such as poor hygiene and consumption of unclean water may increase the prevalence of peptic ulcers in children.
- Physical examination, evaluation of medical history, esophagogastroduodenoscopy (EGD), and biopsy are used to diagnose peptic ulcers in children.
- Antibiotics, antacids, and stress management techniques are used to treat peptic ulcers.
- If left untreated, peptic ulcers in children may cause complications such as intestinal obstruction and bleeding.
- Frequent handwashing, avoiding eating and drinking out, and limiting spicy foods may help prevent stomach ulcers in children.
Signs And Symptoms Of Stomach And Duodenal Ulcers In Children
Sometimes ulcers can be asymptomatic. However, it is common to have a gnawing or burning pain in the stomach that lasts for a few minutes to hours.
The following symptoms may also be seen in the stomach and duodenal ulcers (1).
- Nausea
- Vomiting often with “coffee grounds” appearance or blood
- Lack of appetite
- Weakness
- Bloating
- Weight loss

People with a stomach ulcer may also experience acid reflux, indigestion, a burning sensation in the center of the stomach, and heartburn besides the above.
When To Call A Doctor

Seek medical care or visit a gastroenterology department if your child has signs and symptoms of peptic ulcer. An ulcer may cause burning pain in the stomach in the morning and between meals.
If you notice dark stool and “coffee grounds” vomiting, then make an appointment with the pediatrician immediately. Sudden onset of sharp abdominal pain in a child with a peptic ulcer can be due to perforation that requires emergency care.
What Causes Peptic Ulcers In Children?
The leading cause of gastric (stomach) ulcers and duodenal ulcers is Helicobacter pylori infection although this is less often in children than in adults. Stress, diet, stomach acid and medication can all be causes of ulceration.
Here is the list of the likely causes of peptic ulcer in children (2) (3).
- Helicobacter pylori infection: These bacteria infect the inner lining of the stomach and duodenum. The inner mucous lining protects the stomach and intestine wall from stomach acid and digestive enzymes, such as pepsiniEnzyme produced in the stomach that aids the breakdown of proteins and supports the digestion process . H.pylori may cause inflammation of these mucous membranes, thus resulting in ulcer formation.
- Stress: Physical stress such as injuries, severe burns, major surgeries, etc., may cause stomach ulcers. These stress-induced gastric ulcers are called Curling’s ulcers. However, emotional stress is not the cause of stress ulcer Psychological factors may only increase the perception of ulcer pain.
- Zollinger-Ellison syndrome or gastrinoma: This disease causes increased gastric acid secretion, thus causing ulcers. However, this disease is rare in the pediatric population.
- Nonsteroidal anti-inflammatory medicines (NSAIDs): Medications, such as ibuprofen, aspirin, and naproxen, may cause gastric ulcers. These medicines could be a major cause of non-HP ulceration.
- Obesity: In individuals with excess weight, fat cells produce particles that can lead to inflammation. These particles can travel through blood vessels to various body parts, causing inflammation. Recent discoveries indicate that the cells lining the gut have an inflammatory presence, a crucial finding as persistent inflammation may result in weaker gut cells, making them more susceptible to ulcer formation. Therefore, if your child has excess weight or is obese, there is a significantly higher likelihood of them developing gastric ulcers (4).
Consumption of spicy food does not seem to increase the risk of peptic ulcers (1). Caffeine from coffee may increase the production of stomach acid. However, it is likely to aggravate pain in the existing ulcers (5). A pediatric gastroenterologist can diagnose the cause for the ulcers.
Who Is At Risk Of Peptic Ulcers?
Children who have increased risk of contracting Helicobacter pylori infection are at increased risk of developing stomach and duodenal ulcers.
These bacteria can reach your child through direct contact with saliva, vomit, or fecal matter of an infected person or through contaminated food and water.
The following factors could increase the risk of H.pylori infection in children (6).
- Living in overcrowded conditions

 Point to consider
Point to considerYou may seek medical care if you notice persistent symptoms such as heartburn, abdominal pain, dark stool, dyspepsia (indigestion in children), etc. Early diagnosis and treatment of H.pylori infection could prevent its complications.
How Are Peptic Ulcers Diagnosed In Children?
Pediatricians will listen to the history of symptoms and signs and conduct a physical examination. The following tests are ordered based on the assessment (7).
- Esophagogastroduodenoscopy (EGD) and biopsy is also called gastroscopy, duodenoscopy, or endoscopy. A small, flexible tube (endoscope) with special cameras and light is used to monitor the inner lining of the digestive tract. Ulcers are visualized, and tissue samples are taken with special tools if required. Stomach tissue samples are tested for the presence of pylori. This is the best way of getting a definitive diagnosis.
- Upper gastrointestinal (GI) series or an abdominal x-ray or barium enema. Upper GI series helps visualize the upper part of the digestive system for any gastrointestinal issues. The child will have to drink a barium liquidiA white liquid used in an imaging test to evaluate problems in the upper gastrointestinal tract (contrast) before taking an abdominal x-ray for visibility. This test is performed by a radiologist.
- Rapid urease test (CLO test) is a diagnostic test for pylori infection performed using biopsy samples.
- Stool test could help identify the presence of pylori infection. Stool occult blood test may help to determine blood in the stool.
- In a breath test, the doctor may give food or drink with radioactive carboniCarbon isotope with radioactive properties used in tests to detect Helicobacter pylori infection and ask to blow into a bag after some time. pylori breaks down carbon and forms carbon dioxide, and this can be found in the breath sample if your child has an infection.
- Blood tests may help identify anemiaiA condition characterized by reduced levels of red blood cells and hemoglobin in the body and the presence of inflammatory and infectious markers in the blood.
Treatment For Peptic Ulcer In Children

Ulcer treatment may vary depending on the cause. The following medicines are generally considered for the treatment of peptic ulcer in children(8).
- Antibiotics destroy the bacteria in the stomach.
- H2- blockers, such as cimetidine and famotidine (Pepcid), help reduce the acid secretion in the stomach.
- Proton-pump inhibitors (PPIs), such as omeprazole and lansoprazole, reduce stomach acid production.
- Antacids help neutralize stomach acid. They may help relieve symptoms but do not cure the ulcer.
- Cytoprotective agents protect the mucosal layer of the digestive tract from digestive enzymes and stomach acid. Carafate (sucralfate) and Cytotec (misoprostol) are cytoprotective agents. These are also used for ulcer prophylaxis (prevention of ulcers).
- NSAID-induced ulcers are treated with the withdrawal of NSAIDs and the introduction of PPIs.
Treatment protocols for peptic ulcers and gastritis with H. pylori infection are known as Helicobacter pylori eradication protocols. These treatments aim at eradicating the bacteria along with relief from symptoms.
Any of the below-listed combination regimens with antibiotics and proton pump inhibitor with or without bismuth subsalicylate is given for optimal eradication (9).
- Triple therapy: First-line treatment using antibiotics clarithromycin and amoxicillin or metronidazole with oral PPI is given two times a day for 14 days.
- Quadruple therapy: This is second-line treatment with PPI, bismuth subsalicylate, tetracycline, and tinidazole or metronidazole for ten days.
- Sequential therapy: It is a dual therapy involving treatment with PPI and amoxicillin for the first five days. It is followed by standard triple therapy for another five days.
 Point to consider
Point to considerPediatricians may change the antibiotics if your child has an allergy to a specific antibiotic and if there is any antibiotic resistance in your region.
Elective ulcer surgeries are rarely needed for the treatment of peptic ulcer disease since most children get better with medicines (5). However, perforated peptic ulcer requires laparoscopic omental patch repair (laparoscopic omentopexy) in pediatric patients.
Although several medications here are available over-the-counter, you may visit a pediatrician for diagnosis and exact dosage of medicines according to your child’s health status. Alongside medication, lifestyle changes such as avoiding junk foods and eating a balanced diet to maintain an optimal weight, exercising regularly, and practicing stress management and breathing techniques can be beneficial in managing peptic ulcers.
Complications Of Peptic Ulcers
Peptic ulcers may cause severe complications if left untreated or not treated well. The most common ulcer complications are (5):
- Bleeding: If the ulcers or sores are deep and erode into blood vessels, then it could cause severe internal bleeding, including Upper GI Bleeding. It can lead to bleeding ulcers. “Coffee grounds” vomit and black tarry stool are signs of peptic ulcer bleeding. This can lead to anemia and the requirement of blood transfusion if untreated for a long time.
- Perforation: An ulcer may cause a hole in the wall of the stomach or duodenum. Stomach acid, digestive enzymes, and food could spill into the abdominal cavity through this hole and result in peritonitis (inflammation of the abdominal wall). This is an emergency and will need urgent care.
- Obstruction: Ulcers at the end section of the stomach could block or narrow the intestinal opening. This prevents the entry of food to the intestines and results in severe vomiting.
- Gastric cancer: H. pylori infection and untreated stomach ulcers may trigger stomach cancer later in life. According to the US Centers for Disease Control and Prevention (CDC), individuals infected with H.pylori have a two to six-fold increased risk of developing gastric cancer and MALT (mucosal-associated lymphoid type) lymphoma compared to the uninfected population.
Tips To Prevent Peptic Ulcer In Children

Preventing H.pylori infection is one of the best ways to prevent peptic ulcer disease. The following tips may help your child reduce the risk of peptic ulcers (9) (3).
- Wash hands with soap and water
- Avoid sharing utensils and other items with an infected person
- Drink clean water
- Avoid eating or drinking in unhygienic places
- Consume fruits and vegetables after washing them properly
- Avoid giving NSAIDs for a long time without prescription
- Always take the medications such as Pantop (pantoprazole) given for ulcer prophylaxis were indicated
- Ensure regular medical check-ups for children, especially if you have a family history of ulcers or gastrointestinal issues
Avoiding spicy food, oily foods, or acidic food or having ulcer diets, such as bland diet, are not known to offer a cure for gastric or duodenaliRefers to the first part of the small intestine that absorbs water and nutrients from food from the stomach ulcers (10).
Frequently Asked Questions
1. How can I help my child live with peptic ulcers?
Follow the pediatrician’s prescription for the treatment. Although the symptoms disappear, the recommended course of therapy regimen should be followed to avoid the recurrence of H.pylori infection. You may ask your child to avoid intake of any food that may worsen the symptoms.
2. How long does it take for a stomach ulcer to heal?
Gastric ulcers (gastric) may take more time to heal than duodenal ulcers due to stomach acid. Complete cure of uncomplicated stomach ulcers and duodenal ulcers may take up to six weeks in most patients. However, the symptoms may subside much earlier, and often ulcer heals within two weeks (11). Ulcers caused by NSAIDs begin to heal almost immediately after cessation of drug dosage. Proton-pump inhibitors could further accelerate the healing process (12).
3. Can ulcers be caused by not eating in children?
The research did not show any relationship between diet or malnutrition and stomach ulcers (13).
4. What drink is good for ulcers?
Small-scale research showed cranberry juice effectively suppresses H. Pylori load in adults. However, it may also be effective in children, and your pediatrician may be able to guide you better(14).
Stomach ulcers in children may occur due to an H. pylori infection, unhealthy diet, and several other reasons. Children may experience nausea, vomiting, anemia, and weight loss. If your child experiences sharp abdominal pain and dark stool, consult a doctor, who may diagnose the child using an endoscopy, biopsy, and stool test. Further, they may prescribe antibiotics, H2-blockers, PPIs, or antacids, depending on the diagnosis. Since H. pylori infection in the stomach may be recurrent, it is important to follow the complete treatment regimen. Also, the infection may be prevented by maintaining good hygiene, drinking clean water, and washing fruits and vegetables well before eating them.
Infographic: Peptic Ulcer In Children– Risk Factors And Prevention Tips
Peptic ulcers are a common digestive disorder that can affect individuals of all ages. However, certain children may be at an increased risk of developing peptic ulcers due to factors such as lifestyle and hygiene practices. So, explore the different groups of children with a higher risk and how to prevent these painful sores in the digestive tract.
Some thing wrong with infographic shortcode. please verify shortcode syntax
References
1. Stomach ulcer; BetterHealth; Victoria State Government
2. Symptoms & Causes of Peptic Ulcers (Stomach Ulcers); The National Institute of Diabetes and Digestive and Kidney Diseases
3. Stomach and Duodenal Ulcers in Children; The University of Rochester Medical Center
4. Obesity and Gastric Ulcers; Obesity Action Coalition
5. Stomach and Duodenal Ulcers (Peptic Ulcers) in Children; The Children’s Hospital of Philadelphia
6. Rahul S Mhaskar, et al., Assessment of Risk Factors of Helicobacter Pylori Infection and Peptic Ulcer Disease; The United States National Library of Medicine
7. Diagnosis of Peptic Ulcers (Stomach Ulcers); The National Institute of Diabetes and Digestive and Kidney Diseases
8. Peptic ulcer healing drugs; Department of Health; The Government of the Hong Kong Special Administrative Region
9. Treatment for Peptic Ulcers (Stomach Ulcers); The National Institute of Diabetes and Digestive and Kidney Diseases
10. Eating, Diet, & Nutrition for Peptic Ulcers (Stomach Ulcers); The National Institute of Diabetes and Digestive and Kidney Diseases
11. Ulrich Scheurer, et al.; Gastric And Duodenal Ulcer Healing Under Placebo Treatment; The American Gastroenterological Association
12. Peptic Ulcer; Harvard Health; Harvard Medical School
13. Stomach and Duodenal Ulcers in Children; Stanford Medicine
14. Zhang, Lian, et al.; Efficacy of cranberry juice on Helicobacter pylori infection: a double‐blind, randomized placebo‐controlled trial; PubMed
15. Peptic Ulcers; KidsHealth
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Wayne Hough
Read full bio of Dr Bisny T. Joseph
Read full bio of Swati Patwal
Read full bio of Anindita Ghatak