Image: Shutterstock
Pica is defined as the tendency of children to put non-food substances into their mouths (1). Pica in children is a common occurrence since kids are naturally curious about anything and everything. The most common items that children tend to put in their mouths are dirt, grass, toys, clay, etc. Studies state that the most common causes of pica include anemia and malnutrition (2). Some also link it to certain psychological conditions. Although there are no set rules for preventing pica in kids, keeping an eye out for what babies put inside their mouth and giving attention to their eating habits can help reduce these incidences. Continue reading this post to know more about pica, its causes, treatment, and prevention techniques.
Key Pointers
- Pica is an eating disorder where individuals, mostly children, develop an appetite for non-food items.
- Pica can occur at any age, but it’s more common in people with developmental difficulties.
- Nutritional deficiencies, malnutrition, gastrointestinal distress, oral fixations, and inadequate parental attention are common triggers of pica.
- Children with pica eat non-food items for more than a month, leading to abnormal eating patterns and health problems.
- Pica can cause complications such as lead poisoning, intestinal obstruction, and malnutrition.
What Is Pica?

Pica is an eating disorder in which children develop cravings for non-food items for more than a month. The word ‘pica’ comes from the Latin word magpie, a bird with an indiscriminate appetite. It is also known as compulsive eating disorder.
Pica disorder can surface at any time during childhood, adolescence, or adulthood, especially in individuals with developmental disabilities. Pica could be more prominent among people of lower socio-economic groups with probable attribution to poor child-rearing practices such as child abuse and neglect (1) (3).
Children with pica eat a variety of substances such as:
- Clay
- Cloth
- Sand
- Paint
- Chalk
- Glue
- Soap
- Ice
- Hair
- Coffee grounds
- Cigarette ashes
- Paper
- Metal
- Talcum powder
- Starch
- Pebbles
- Animal feces
- Rubber bands
- Shampoo
 Quick fact
Quick factCauses Of Pica In Children
The exact cause of pica in children is unknown. It is essential to identify the root cause of pica for effective management. Below are some of the most common triggers (3) (4) (5).
- Gastrointestinal distress: Some children with GI distress might find it soothing to eat non-food items, especially earth.

- Nutritional deficiency: Iron deficiency, zinc, calcium, or some other trace element deficiencies may trigger specific cravings. The US Centers for Disease Control and Prevention (US CDC) states, “At least half of children worldwide under 5 years old suffer from vitamin and mineral deficiencies (6).”
- OCD in children: The anxiety arising out of these disorders might make the individual eat non-food items to get some relief. Any attempts to forcefully stop them from eating might increase their anxiety and distress, resulting in chronic stress.
- Malnutrition in children: Deficiency in the intake of nutritious food might trigger cravings for soil or clay. Though soil/ clay does not have the nutrients to meet the deficiencies, it binds to iron in the gastrointestinal tract, thus soothing the cravings.
- Oral fixations: Some children have an oral fixationiA repetitive and detrimental behavior involving the use of the mouth , an obsessive urge to put things in their mouth. This is common in very young kids.
- Mental, growth, and developmental delay: Children, especially those with autism spectrum disorder or other developmental conditions, might eat unhygienic or non-food materials like dirt or paper due to their inability to differentiate (7). Regular consumption of nonfood substances may lead to gastrointestinal problems. Consequently, a collaborative study supported by the US CDC revealed that children diagnosed with autism spectrum disorders (ASD) were over three times more likely to have parent-reported gastrointestinal symptoms compared to children in the general population (8).
Tisha, a mother of three boys, has encountered a challenging situation with Pica. She shares, “My two eldest children have been diagnosed as being on the autism spectrum, and both of them have exhibited pica behavior. However, my four-year-old middle child displays a more consistent pattern of chewing on non-food items, such as crayons, chalk, wood, paint chips, and USB cables (i).”
- Lack of proper appetite stimulation: Selective eating or picky eating may lead some children to suppress their hunger by resorting to eating non-food objects.
- Poor parental attention: Parental neglect is a major cause seen mostly in people living in poverty where they might fail to supervise their child’s diet.
- Celiac diseaseiAn autoimmune and genetic condition characterized by an immune reaction to gluten, the protein found in barley, rye, and wheat : Sometimes, celiac disease in children may develop nutritional deficiencies due to malabsorption. These deficiencies can lead to various issues, including unusual cravings for non-food items. Iron deficiency is common in celiac disease; iron deficiency anemia (IDA) may lead to pica. One type of pica that children with long-standing IDA may develop is lithophagia, a compulsive desire to eat pebbles and stones (9).
- Cognitive impairment: Cognitive impairment in children can raise the risk of developing comorbid psychiatric conditions, and one of them is pica. Some reports show the association between pica and children’s cognitive impairment, which may occur primarily due to iron deficiency (or low ferritin levels) in such individuals (10).
- Hypothyroidism: According to experts, an underactive thyroid can lead to poor iron absorption. Hence, it’s essential to check your iron and ferritin levels (11), which are also caused by pica. Therefore, it might be possible that children with hypothyroidism may also develop pica. However, no direct association between hypothyroidism and pica has been found (12).
All the triggers and causes shared above are etiological theories prevalent since ages but no one theory could be attributed to the cause of pica and its various subtypes. If your child is eating non-food items almost every day, then observe them as this could be the symptom of pica. Consult a pediatrician as you yourself may not identify the symptoms well.
Children below two years of age usually explore many things through their mouth, it is not pica even if they are ingesting non-food items. It is important for you to ensure they consume appropriate foods and receive the optimum pediatric nutrition.
Pica Signs In Kids
Recognizing the signs of pica can help identify this condition early. It’s vital to observe the child’s eating habits and behaviors closely. If certain signs persist, it may indicate that pica is present, and professional intervention could be necessary. These are some signs which could help you identify pica in children (13):
- The child has been eating non-food substances for more than a month despite efforts to stop it.
- Their eating patterns and cravings are not on par with their age or behavior.
- Your child’s eating habits are not a part of some ethnic or cultural food traditions. For example, in parts of Africa and some rural areas of the US, eating clay is believed to cure gastrointestinal issues or problems (14).
- If your child is recurrently consuming high amounts of soil that can be a soil-pica syndrome or geophagia. This could be due to serious iron-deficiency.
Depending on the substances the child is eating, they may have a few other symptoms such as (15):
- Stomach pain, nausea and bloating due to intestinal or stomach blockage.
- Poor nutrition and fatigue.
- Behavior problems
- Lead poisoning
Pica is not a standalone condition as certain deficiencies lead to this problem, and this problem leads to a few more mild or severe complications. In total, identifying pica is a challenge and calls for an expert’s intervention for proper diagnosis.
Possible Complications Of Pica
Indiscriminate eating of non-foods may lead to complications. These complications can range from mild to severe, and prompt attention is necessary to prevent lasting damage. Here are some potential complications associated with pica (16) (17) (18) (19):
- Lead poisoning, if the child consumes paint or sand contaminated with lead.
- Gastrointestinal complications such as constipation, ulcerations, perforations, diarrhea, parasites, nutrient malabsorption and bowel obstruction
- Intestinal obstruction from eating something that can injure or block the intestines.
- Mouth injury when the child swallows or eats some sharp or hard substance.
- Dental erosion as coarse substances harm the teeth while chewing.

- Infections from eating feces or dirt.
- A Bezoar, referring to a mass of indigestible material such as cloth, hair, etc. trapped inside the body, most often in the stomach.
- Mercury poisoning due to the ingestion of tissue boxes and cigarette packages.
You can avoid these complications with timely diagnosis and treatment of pica. Under these circumstances, you can’t delay taking the child to a doctor.
When To See A Doctor?
You need to see a doctor when you find the aforementioned signs of pica in the child or they have any of the above complications. Consider it as an emergency and seek medical help immediately if:
- Your child has consumed something harmful or poisonous such as lead or mercury.
- Your child is regularly eating paint flakes.
- The substance consumed is infectious, such as feces, that might lead to serious health implications.
- The child is bloating from an intestinal blockage, such as a case of Bezoar.
Diagnosis Of Pica

There are no laboratory tests or a single approach diagnosis for pica. Hence, a pediatrician might use the below methods (20):
- The doctor will primarily look at the child’s physical symptoms such as an upset stomach or any other bowel problems like bloating.
- If a child falls in the risk group, such as a child with developmental concerns, the doctor may ask the parents if they have seen their child eating nonfood items. If yes, then for how long.
- They will try to know about the child’s medical history, psychological development, and behavioral issues.
- The doctor may specifically want to know about the child’s food habits and the ambiance at home and school to understand the possible triggering factor. They may also assess your child’s social behavior and emotional health to see if pica is linked to a broader behavioral issue.
- If any suspected behavior has occurred for one month or more than that, the doctor may order tests, such as blood tests or X-rays to confirm pica. Blood tests check anemia, toxins in the blood, blockages in the intestines, and for iron and zinc deficiency. Insufficiency of these vitamins or vitamin deficiency might be a cause for eating dirt (or clay) in certain cases. The doctor may also conduct a stool test to check for parasitic infections.
- Sometimes, imaging or an X-ray may be required to identify what was consumed or to closely observe conditions such as obstructions in the intestines or bowels if any is suspected.
These steps will enable the doctor to diagnose pica and its complications and try to ascertain the cause behind it to the maximum probability.
Treatment Of Pica In Children
There is no one-way or direct treatment approach for pica, as it all depends on the underlying causes. The pica literature reports various treatments for pathological pica, such as nutritional, psychological, pharmacological, behavioral, ecological, and sensory approaches (21).
- Nutritional intervention: In most cases, addressing the mineral or nutrient deficiency through dietary changes and nutritional therapy may resolve the pica problem in the child. If dietary intervention is not sufficient, supplements could also be considered under the guidance of a pediatrician.

- Psychological intervention: Counseling, behavioral therapy, and psychotherapy may be recommended for individuals in whom pica is believed to be attributable to emotional or psychological disturbances.
 Point to consider
Point to consider- Pharmacological intervention: Medicines may be prescribed to reduce abnormal eating patterns if pica is linked with an intellectual or developmental disability in a child.
- Behavioral intervention: Several behavioral approaches have been reported in the literature. If pica is found to be associated with the behavioral issues, the doctor may recommend consultation from a psychologist. This approach though, is considered more useful for children with developmental disabilities.
- Sensory intervention: Sensory characteristics of a non-food item when identified can help in finding the edible replacements for it, which then will help in treating the condition.
Frequently Asked Questions
1. At what age can pica be diagnosed?
Pica can be diagnosed in children older than two years since it is natural for babies and infants to want to taste or put different things in their mouths (22). Studies show that pica is most frequently observed in 36-month-old children, with 2.29% of caregivers noting this behavior. As children age, the prevalence of pica gradually decreases (23).
2. Do kids with ADHD have pica?
Although some studies show that pica and ADHD may occur together, both the conditions are not believed to be related. However, similarity may be drawn between the two based on impulsivity and ADHD-associated bulimia nervosa (24). The symptoms of bulimia nervosa include strange eating habits (25).
3. Is pica in children a serious condition?
While it is generally considered harmless, pica can potentially lead to the consumption of toxic or non-edible substances, resulting in adverse effects. Therefore, parents must be watchful for new symptoms in their children and seek professional help when necessary, as the condition is usually treatable with therapy and lifestyle changes (26).
Pica in children is an unusual albeit normal occurrence. Most children outgrow it as they get older. However, those with neurological or developmental problems may continue having pica even during adolescence and adulthood. Though the exact cause of pica is unknown, nutritional deficiencies, malnutrition, and oral fixation are some common triggers. Since pica can cause complications that could affect a child’s long-term health, its timely diagnosis and treatment initiation are preeminent. Keeping the house clean and safe and monitoring your child’s eating habits are additional ways to ensure their safety.
Infographic: Tips For Parents To Help Their Children With Pica
Children craving non-edible things is unhygienic and can lead to infections. So if you have noticed signs of pica in your child, you must intervene and take some steps at home to stop their unusual cravings and prevent complications. Learn the effective ways to deal with pica in children through this infographic. Illustration: Momjunction Design Team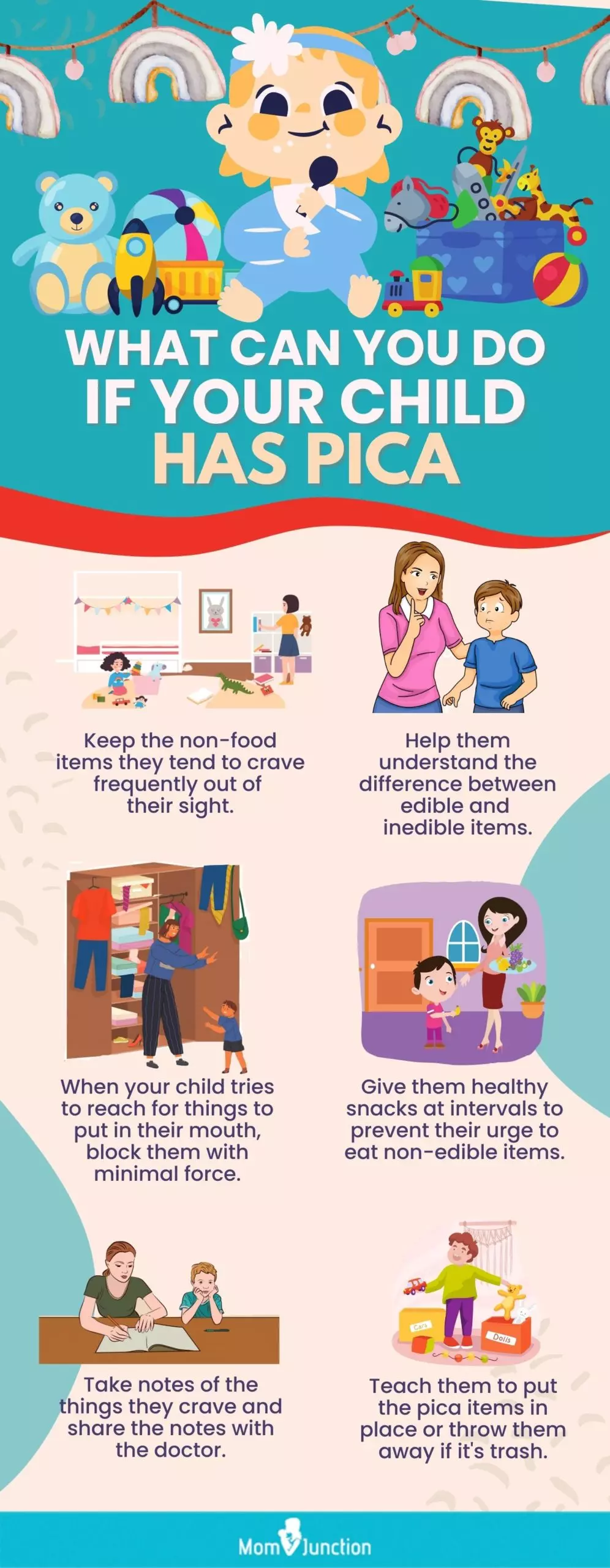
Illustration: Pica In Children: Signs Causes Risk Factors And Treatment

Image: Stable Diffusion/MomJunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. My experience with a child with pica and autism/5 tips for managing pica in kids/autism awareness.https://www.youtube.com/watch?v=AHTXiLWeSRw&feature=youtu.be
References
1. Yasir Khan and Glenn Tisman; Pica in iron deficiency: a case series; Journal of Medical Case Reports.
2. What is Pica?; National Eating Disorders Association
3. Sekar Pasupathy and Srujana Swarna;Clinical profile, sociodemographic and biochemical determinants of PICA among 1 to 5 aged children attending a tertiary care hospital;International Journal of Contemporary Pediatrics,Vol. 5 (6) (2018)
4. Annette E. Chalker; The Psychopathology of Pica: Etiology, Assessment, and Treatment;Inquiries Journal (2017)
5. Shweta Advani et al.;Eating everything except food (PICA): A rare case report and review;National Centre for Biotechnology Information (2014)
6. Micronutrient Facts;Centers For Disease Control And Prevention
7. Matson JL1, Hattier MA, Belva B, Matson ML; Pica in persons with developmental disabilities: approaches to treatment; NCBI.
8.Reynolds, Ann M., et al.; Gastrointestinal Symptoms in 2- to 5-Year-Old Children in the Study to Explore Early Development; Journal of Autism and Developmental Disorders (2021)
9. Mosayeb Shahryar et al.; Lithophagia as a clue for celiac disease: a case report and literature review; NCBI (2017)
10. Melody Ashworth;Pica among Persons with Intellectual Disability: Prevalence, Correlates, and Interventions; University of Waterloo (2006)
11. Iron and Ferritin Deficiency; Thyroid UK
12. Mehwish A Mirza, Ricky Ayala, and Jacqueline Savage; SAT-487 Untreated Primary Hypothyroidism Presenting as Pica with Concurrent Hyponatremia and Rhabdomyolysis; Journal of the Endocrine Society (2020).
13. Pica; National Eating Disorders Association.
14. Frances K. Millican et al.;Study of an oral fixation: Pica;Science Direct
15. Pica; MedlinePlus
16. Pica;Kids Health, Nemours (2014)
17. Anderson JE1, Akmal M, Kittur DS; Surgical complications of pica: report of a case of intestinal obstruction and a review of the literature;National Centre for Biotechnology Information (1991)
18. Ramnik Patel, Shiva Jayakumar, Manasvi Upadhyaya, David Drake; Pediatric Gastro-Duodenal Fabric Bezoar; Department of Pediatric Surgery, Evelina London Children’s Hospital St Thomas’ Hospital, London, UK.
19. Bruce E. Johnson; Chapter 148Pica; Clinical Methods: The History, Physical, and Laboratory Examinations. 3rd edition; National Centre for Biotechnology Information (1990)
20. Pica;Family Doctor;American Academy of Family Physicians
21. Lillian N. Stiegler;Understanding Pica Behavior:A Review for Clinical and Education Professionals;Semantic Scholars
22. Pica. Connecticut Children’s
23. Fussy eaters are more likely to experience Pica eating disorder; Cardiff University
24. Soumaya Bourgou et al.; Pica in an Adolescent with Attention Deficit Hyperactivity Disorder responsive to Methylphenidate,; National Library of Medicine (2021)
25. Bulimia Nervosa; Johns Hopkins Medicine
26. Pica; Cleveland Clinic
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Raju C Shah
Read full bio of Swati Patwal
Read full bio of Rohit Garoo
Read full bio of Shinta Liz Sunny