Image: Shutterstock
During pregnancy, the placenta is developed in the uterus as an important organ to provide nourishment and protection to your baby.
In some pregnancies, it can become tethered to the lower section of the uterus, causing a pregnancy-related complication called placenta previa, or low-lying placenta. However, mostly the placenta is attached to the top or side of the uterus by the umbilical cord (1). Read this post to know more about placenta previa, how it affects your pregnancy and your baby, and a few strategies to correct or manage it for safe and healthy childbirth.
Key Pointers
- The placenta lies low in the uterus and covers the cervix in the placenta previa.
- An ultrasound scan can determine the type of placenta previa.
- The cause of placenta previa is unknown, but some risk factors are previous uterine surgeries, advanced maternal age, and multiple fetuses.
- Symptoms of placenta previa include vaginal bleeding and early labor symptoms.
- The delivery method can vary depending upon the condition, with some women delivering vaginally and others through a c-section.
What Is Placenta Previa?
Placenta previa is a pregnancy complication that occurs when the placenta lies low in the uterus and covers a part, or the entire cervix, which is the opening to the birth canal (2).
Placenta previa occurs in one out of 200 pregnancies (3). The condition is not a concern if it happens in the early stages of pregnancy. But if it occurs during labor and delivery, it could lead to complications that can harm both the mom and the baby.
What Are The Types of Placenta Previa?
- Marginal previa, where the placenta borders the cervix
- Partial previa, where the placenta covers only a part of the cervical opening
- Complete previa, where the placenta covers the cervix entirely
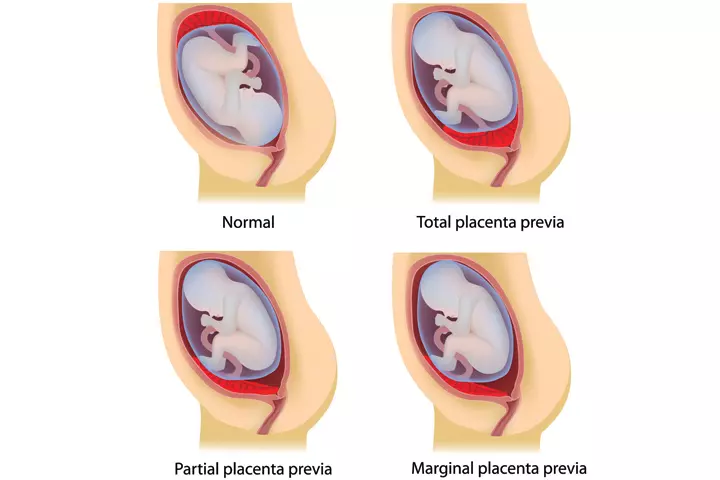
They can be further classified into anterior placenta previa and posterior placenta previa, which refers to the exact placental position within the uterus. It can be defined through an ultrasound scan (4) (5).
What Are The Causes Of Placenta Previa?
The actual cause of placenta previa is unknown.
But some factors can increase the likelihood of this condition (6).
Risk factors that increase the chances of a low-lying placenta include:
- Previous surgeries of the uterus, such as a C-section, D&C (dilation and curettage) or uterine fibroid removal
- Second or subsequent pregnancy
- Advanced maternal age
- Carrying twins, triplets, or more
 Quick fact
Quick factHowever with most cases, sometimes there are no risk factors.
These risks cannot be controlled. Others that can be controlled to prevent placenta previa include:
- Smoking
- Cocaine consumption (2)
Knowing the symptoms of this condition could help in an early diagnosis.
What Are The Symptoms and Signs Of Placenta Previa?
The signs and symptoms of placenta previa differ from one pregnant woman to another. While some do not experience any placenta previa symptoms, others show warning signs such as (7):
- Sudden onset of painless, bright red vaginal bleeding that can range from light to heavy.
- Early labor symptoms such as regular contractions, and pain in the belly, or lower back.
 Point to consider
Point to considerYou must call your obstetrician immediately if you notice vaginal bleeding during your pregnancy, irrespective of the trimester.
If you do not experience any symptoms, your doctor may be able to identify a placenta previa during your regular prenatal ultrasound scans. Early detection helps manage the condition more effectively and allows the mother and healthcare providers to prepare for any needed interventions.
How Is Placenta Previa Diagnosed?

Placenta previa is diagnosed by ultrasound. Most cases are detected during the second-trimester checkup when you have a routine ultrasound test. The diagnostic tests include (8):
- Ultrasound scan
- A combination of abdominal and transvaginal ultrasounds, in some cases
To ensure proper fetal and maternal health, activity limitations will be imposed by your doctor upon detection of placenta previa.
Here are some questions your doctor may ask to confirm the diagnosis:
- When did you first notice vaginal bleeding?
- Was the bleeding only once, or was it recurring?
- Do you have any pain or contractions?
- Is the bleeding heavy?
- Did you undergo any surgeries such as fibroid removal, cesarean, D&C, or abortion?
- Is this your first pregnancy?
- How long does it take to reach the hospital in case of an emergency?
- Do you smoke?
- Is there anyone who can accompany you when required?
If the diagnosis is confirmed, you can ask your doctor these questions:
- Is there a chance of the condition resolving on its own?
- How do I take care of myself?
- How can I manage the bleeding?
- What symptoms should prompt me to go to the hospital?
- When should I revisit the hospital?
- Will a placenta previa increase the chances of complications in future pregnancies?
- Can I deliver vaginally?
In addition to this, your doctor may also give you care instructions and precautions to take when you have a placenta previa.
How Is Placenta Previa Treated?
There are no medical or surgical treatments for curing placenta previa (8). However, the condition can be managed by alleviating the bleeding and discomfort (2).
Management and treatment depend on some factors:
- The health of the mother and the baby
- The position of the baby
- The location of the placenta
- The amount of blood loss
- The gestational age of the baby
- The type of placenta previa
If you are diagnosed with placenta previa before the 20th week of pregnancy, it is likely to resolve. The placental position can change with the growing uterus and can move away from the cervix.
If it does not resolve or placenta previa is diagnosed in the later stages of pregnancy, it may be considered a high-risk pregnancy and your doctor may most likely suggest a C-section. If a previa is detected on your 18-20 week ultrasound, a follow-up ultrasound is usually recommended around 28 weeks, and if still present, around 32-34 weeks.
Tina, a mother, recounts her experience of requiring a cesarean section due to placenta previa during her pregnancy. She recalls, “I did have a birth plan of doing a natural birth, in the natural birthing center, at the hospital but due to placenta previa, I had to have a c-section at 37 weeks (i).”
What To Do When You Are Not Bleeding Or Bleeding Lightly
- Be prepared to go to the hospital if bleeding turns heavy or resumes.
- If the placenta is placed low but is not covering the cervix, your doctor may suggest a vaginal delivery.
You are bleeding heavily
- Go to the doctor immediately as a blood transfusion may be necessary in the case of severe bleeding (9).
- The doctor prescribes steroids if you are not nearing the due date, or haven’t reached the 37th week, to prepare the baby by speeding up the development of his or her lungs.
- The OB/GYN will plan a cesarean if you are past the 36th week (10).
Your bleeding does not stop
- Emergency cesarean, even if you are not nearing the due date.
These are situations when you need to visit the doctor immediately, to prevent any harm to you or your baby.
Precautions For Low-Lying Placenta

These precautions help you avoid further complications caused by a low-lying placenta (2).
- Avoid strenuous activities, such as intense cardio exercise or lifting weights
- Avoid sexual intercourse
- Take bed rest
 Quick tip
Quick tipPrecautions are important because placenta previa can lead to some serious complications.
Tina reflects on her challenging journey, “The most difficult part was the light-duty/bed rest part of placenta previa and honestly the pelvic rest! I’m also such a busy body, that resting made me stir crazy! Tough stuff! … When I couldn’t exercise anymore, due to the placenta previa, I turned to meditation and counseling. I’m a firm believer in mental health!”
What Are The Complications Of Placenta Previa?

Some possible complications of placenta previa include (5):
- Hemorrhage (heavy bleeding)
- Fetal distress from lack of sufficient oxygen
- Premature birth that is before the 37th week of pregnancy
- Birth defects
- Delayed fetal growth
- Health risks to the baby
- Emergency C-section
- Hysterectomy, when the placenta fails to deliver from the uterine lining
- Increased risks of placental abruption
- Placenta accreta, where the placenta attaches deep into the uterine wall and mandates a hysterectomy at the time of delivery
- Premature birth before the 37th week of pregnancy A meta-analytical study by researchers from the University of Amsterdam and the Amsterdam Reproduction and Development Research Institute found that women with placenta previa had a 46% incidence rate of premature birth before 37 weeks.
While you cannot correct a low-lying placenta, you can manage the condition. Next, we’ll tell you how.
How To Cope With Placenta Previa?
Here is how you can do it:
- Learn everything about the condition: Having clarity about the condition eliminates unwanted doubts, fears, and anxiety. Talk to your doctor or connect with others (you can find in support groups) who have the same condition. Sharing experiences may offer emotional comfort and useful advice.
- Prepare for cesarean section: Placenta previa makes vaginal delivery impossible and dangerous. Therefore, a cesarean delivery will become necessary for your baby’s and your well-being.
- Rest: You may not like the idea of bed rest, but you need it at this time. Use the free time to pursue a hobby or read about baby care and shop online.
Tina candidly discusses her experience dealing with a diagnosis of placenta previa, “The coming to peace part was hard. It was really hard because I felt like I was being punished in some weird way, having trouble conceiving, having placenta previa, and then a NICU baby. I honestly think the peace came at the very end when we were home, and I was holding my son in my arms and realized what warriors’ women are and things were going to be okay.”
How To Prevent Placenta Previa?

There is no way to prevent placenta previa since there is no particular cause for it.
However, if the risks for you are high owing to your age, prior surgeries, or previous pregnancies, try to be extra careful and maintain a healthy lifestyle. Most importantly, stay away from cigarette smoking and cocaine consumption as they are associated with the condition.
Next, we answer a few commonly asked questions about placenta previa.
Frequently Asked Questions
1. Is placenta previa genetic (hereditary)?
No, placenta previa is an obstetric complication and not a genetic condition (2).
2. Can I fly with a low-lying placenta?
Avoid flying to avoid bleeding while in flight.
3. Is placenta previa more common when pregnant women carry a boy?
Only a few studies have shown that women carrying a baby boy may be at a greater risk of placenta previa. However, the cause behind this association has not been found (11) (12).
4. Can placenta previa cause a miscarriage?
Placenta previa is generally not an identified cause of miscarriage until around or after the 20th week of pregnancy. Miscarriage refers to the loss of a pregnancy that occurs before reaching 20 weeks of gestation. Given this timeline, it is uncommon for placenta previa to be a direct cause of miscarriage (13).
5. What is the difference between placenta previa and placental abruption?
Placenta previa is about the placenta’s position, while placental abruption is about it coming off the uterus too soon. Placental abruption occurs when the placenta separates from the uterine wall before delivery, which can affect the oxygen and nutrient supply to the baby. Symptoms include vaginal bleeding, abdominal pain, reduced fetal movements, and uterine contractions (14). Although both conditions involve bleeding during pregnancy, they have different causes.
If diagnosed with placenta previa, remain vigilant for any vaginal bleeding. Visit the clinic as instructed by the doctor. Avoid strenuous activities during pregnancy. If you’ve undergone uterus-related surgeries in the past or have an increased risk of placenta previa, keep your doctors informed at an early stage. Placenta previa is a concerning condition that may increase your anxiety until delivery. But proper rest and medical attention could help you deliver a healthy baby. Hence, visit the hospital as directed and rest well.
Infographic: Types Of Placenta Previa And Precautions To Take
Placenta previa can lead to complications at the end of the pregnancy and during childbirth. An ultrasound scan can be used to determine the type of placenta previa a woman has and help tailor her therapy. Learn more about placenta previa types and the precautions you should take to ensure a successful pregnancy by exploring the infographic below.

Illustration: Momjunction Design Team
Dive into the depths of the placenta previa through this comprehensive video. Uncover its causes, signs, diagnosis, treatment, and pathology – all critical knowledge to navigate this pregnancy concern.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Interview with Tina: One mom’s journey surviving placenta previa;https://medium.com/@gloriamond/interview-with-tina-one-moms-journey-surviving-placenta-previa-4ade3a5ac942
References
1. What is the placenta?; Pregnancybirthbaby
2. Placenta previa; The National Library of Medicine;
3. Mabie WC; Placenta previa; Department of Obstetrics and Gynecology, University of Tennessee, Memphis.
4. Shumaila Zia; Placental location and pregnancy outcome; J Turkish-German Gynecol Assoc 2013
5. Frances M. Anderson-Bagga and Angelica Sze.; Placenta Previa
6. Placenta Previa; The University of Rochester Medical Center
7. Robert K. Stoelting, et al.; Placenta Previa; Stoelting’s Anesthesia and Co-existing Disease
8. Bleeding in Pregnancy/Placenta Previa/Placental Abruption; The Children’s Hospital of Philadelphia
9. Placenta Previa; Stanford Children’s Health
10. Heller HT, et al.; Outcomes of pregnancies with a low-lying placenta diagnosed on second-trimester sonography
11. S W Wen et al.; Placenta praevia and male sex at birth: results from a population-based study; NCBI (2000)
12. K Demissie et al.; Placenta previa: preponderance of male sex at birth; NCBI (1999)
13. Placenta Previa; Cleveland Clinic
14. Bleeding in Pregnancy/Placenta Previa/Placental Abruption; The Children’s Hospital of Philadelphia
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Christian Pope
Read full bio of Rebecca Malachi
Read full bio of Swati Patwal
Read full bio of Dr. Joyani Das