Image: ShutterStock
Placental abruption is a rare pregnancy complication that may adversely affect the mother and baby.

Data shows that around one in 100 pregnant women experiences placental abruption, an important factor contributing to perinatal and maternal morbidity globally (1).
Understanding what placental abruption is and what causes it is vital for pregnant women to get immediate medical help and avert its complications. Timely recognition can be life-saving for both the mother and the baby.
Continue reading to learn more about placental abruption, including its causes, risk factors, signs and symptoms, diagnosis, treatment, management, and prevention. This post also discusses some frequently asked questions about placental abruption, such as whether it can be caused by exercise.
Key Pointers
- Placental abruption is an uncommon condition that affects 1 in 100 pregnant women.
- It occurs when the placenta detaches early from the uterus before birth.
- Causes of placental abruption include high blood pressure, problems with the amniotic sac, advanced maternal age, and other risk factors.
- Symptoms of placental abruption include vaginal bleeding, abdominal pain, a tender and hard uterus, frequent contractions, and fetal distress.
- Placental abruption can be diagnosed through a physical exam, blood tests, fetal heart rate monitoring, and vaginal ultrasound.
- Measures to prevent placental abruption include avoiding alcohol, tobacco, and non-prescription medicines, maintaining stable blood pressure, and adhering to a healthy diet and sleep schedule.
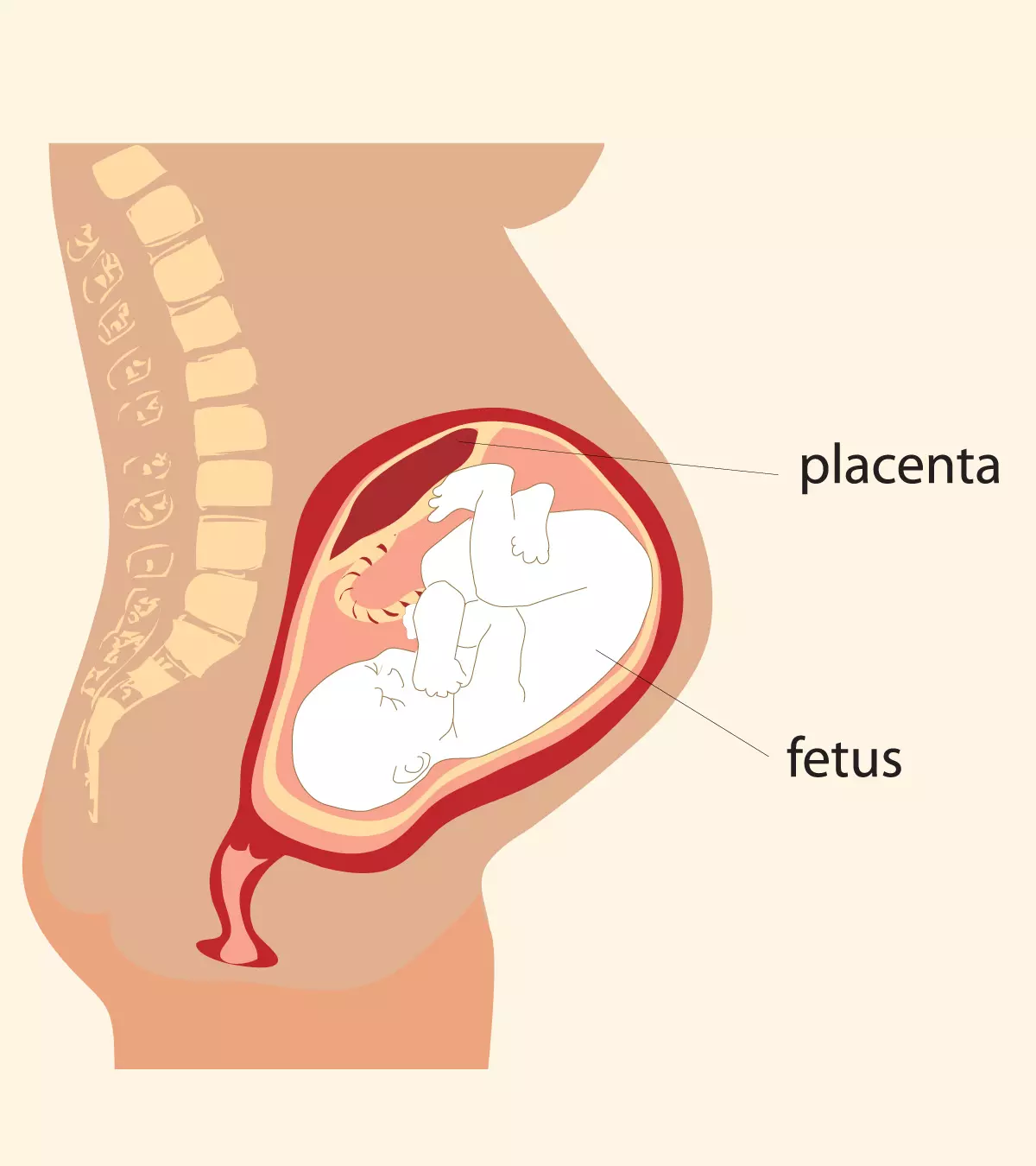
What Is Placental Abruption?
Placental abruption, premature separation of placenta or detached placenta, is a rare but serious complication of pregnancy.
It is the separation of the placenta from the uterus before the birth of the baby.
This condition occurs after the 20th week of pregnancy, commonly in the third trimester, suddenly during labor, and deprives the baby of oxygen and nutrients and can initiate severe bleeding in the mother and a possibility of kidney failure and a threat to life(2).
Severe abruption of the placenta during pregnancy is life-threatening to the mother and the baby (3).
Based on the separation and location of the placenta, placental abruption is of three types – complete, marginal, and central (3).
- Complete placental abruption: The placenta is completely separated from the lining of the uterus, causing heavy vaginal bleeding.
- Marginal (partial) placental abruption: The placenta is separated only at the edges, resulting in some vaginal bleeding
- Concealed (central or silent) placental abruption: The blood is trapped between the placenta and the uterine wall with no vaginal bleeding.
What Are The Causes And Risk Factors For Placental Abruption?
The cause of placental abruption is usually unknown.
However, one probable causative factor is the irregular supply of blood in the placenta or uterus which can be a result of inadequate placental formation which happens in the very early part of pregnancy at implantation but manifests later. Other factors that could pose a risk of placental abruption are (4).
- History of placental abruption in previous pregnancies; there is a 10% chance of placental abruption in a subsequent pregnancy
- High blood pressure (hypertension) before or after conception (preeclampsia)

- Problems associated with the amniotic saciThe thin-walled fluid-filled sac in the uterus where the embryo grows and eventually forms the fetus.
- Maternal age, pregnancy before 20 or after 35 years
- Short umbilical cord
- Preeclampsia: raised blood pressure
- Gestational Diabetes
- Thrombophilia (abnormal development of blood clots)
- Delivery through c-section in an earlier pregnancy
- Abdominal trauma caused by accidents, falls or infections
- Preterm rupture of membranesiA pregnancy complication where the amniotic sac's membranes break before labor starts, leading to amniotic fluid leakage.
- Intrauterine infectionsiA condition where the vaginal bacteria infect the umbilical cord, amniotic fluid, or membranes enclosing the fetus.
- Multiple gestation (carrying more than one baby)
- Placenta previa
- Carrying more than one baby (twins or multiples)
- Maternal smoking, which is associated with a 90% increased risk (5)
- Maternal cocaine use
- A family history of placental abruption in first-degree relatives
Though you cannot prevent all of these risk factors, there are some things you can avoid, such as alcohol and tobacco and take proper nutrition and regular pregnancy check ups, to lessen your odds.
Being prepared for it and knowing how to identify it can help minimize the risks to the mom and the baby.
 Quick fact
Quick factWhat Are The Signs And Symptoms Of Placental Abruption?
The signs and symptoms vary from moderate to severe. Watch out for (6):
- Vaginal bleeding
- Pain in the abdomen when touched or otherwise
- Lower back pain

- Tender and hard uterus (womb)
- Frequent and painful uterine contractions
- Fetal distress, such as abnormal heart rhythm
Back pain or discomfort, and sometimes spotting, which are quite common during pregnancy, are the usual symptoms of placental abruption. However, they cannot be regarded as signs of placental abruption alone. These symptoms will worsen with time in the case of abruption and need immediate medical intervention.
 Point to consider
Point to considerHow Is Placental Abruption Diagnosed?
The condition is diagnosed based on the symptoms, vaginal bleeding, pain, and discomfort. Your healthcare provider will conduct a few tests to confirm the cause and give the right treatment (7).
- Physical exam: The doctor will perform a physical exam to check the state of your uterus. Any rigidness or tenderness in the uterus indicates a problem that needs medical attention.

- Blood tests: Your doctor may conduct a complete blood count (CBC) to know your platelet count. A low platelet count increases the risk of blood loss. A blood test can also confirm if you have anemia. Anemia can indicate heavy blood loss due to placental abruption.
- Fetal heart rate monitoring: It confirms the state of the baby’s health by measuring the fetal heart rate and rhythm. Abnormal heartbeat could be an indication of placental abruption
- Vaginal ultrasound: It helps your doctor detect vaginal bleeding and placental separation.
In some cases, the condition cannot be diagnosed until delivery. The delivered placenta shows attached blood clots which appear old. The placenta is then sent to the laboratory for further testing.
Placental Abruption: Management and Treatment
Regardless of the condition’s severity, the doctor will monitor you and the fetus closely, depending on how far along you are in pregnancy (8).
- Mild condition and early pregnancy: If the vaginal bleeding stops and your baby is not distressed, you are told to take rest at home.

- Moderate condition and early pregnancy: Your doctor may want you to remain in the hospital until the delivery. Medications are prescribed for maturation of the baby’s lungs.
- Mild to moderate conditions and late pregnancy: Your doctor will recommend delivery and tries for a vaginal birth. If the placenta separates further from the uterine wall, the doctor may suggest a cesarean delivery.
- Severe condition: You may have to go for immediate delivery, followed by supportive care. Heavy bleeding can be either treated by blood transfusion or hysterectomy (surgical removal of the uterus done here as a life-saving procedure). In the case of hysterectomy, you will not be able to get pregnant again.
Even after the treatment for placental abruption or delivery, it is recommended for mothers to attend follow-up appointments with their OB/GYN to monitor their recovery. Also, seek medical care if you experience discomfort or unusual symptoms during your recovery.
What Are The Complications Of Placental Abruption?
There won’t be any complications in the case of partial placental abruption, where only a small part of the placenta separates (retroplacental clot).
But if all of it or a significant part of the placenta separates, it can lead to complications (9).
In the mother, it can lead to:
- Blood loss, causing shock
- Blood clotting problems
- Maternal death from blood loss
- Need for blood transfusion
A mother of two shares her story of having had a placental abruption during the birth of her baby girl. She says, “I suffered a placental abruption just as we were getting ready for bed Sunday night. I had a difficult time in surgery because, besides having a placental abruption, they discovered I had a rare condition called placenta accreta. I apparently lost so much blood I didn’t have protein/plasma in my blood to stop bleeding, and I was hemorrhaging. After having had three blood transfusions and two plasma transfusions, our wonderful and talented doctor was able to save me (i).”
- Failure of kidneys, liver and pituitary gland
- Preterm labor
- Uterine rupture
- Hysterectomy in the case of uncontrollable uterine bleeding
In the baby, it can lead to:
- Low birth weight due to restricted baby growth
- Restricted oxygen supply (leads to brain damage, or even baby’s death)
- Premature birth (before 37 weeks gestation)
- Miscarriage or stillbirth
- Stillbirth or fetal death
- The newborn may have learning disabilities in the later stages of development
Paul Isaacs, a prematurely born boy, shares his story of how placental abruption led him to have a series of problems in later stages. He says, “My mother and I were both in distress during her pregnancy – I was born premature and was born via a cesarean section, and my mother suffered heavy bleeding as a result of what is called placental abruption (ii).
In another blog, Isaac adds, “Brain damage and/or brain injury is a part of the reason why I have autism. The placental abruption and oxygen deprivation that happened, caused the stroke, left-right disorientation, visual perceptual disorders, language processing disorder (aphasia), and issues with internalizing and externalizing language and other developmental aspects (iii).”
According to the National Institutes of Health (NIH), placental abruption accounts for about one to five percent of maternal fatalities annually in the US. The likelihood of fetal mortality, on the other hand, varies from 1% to 40% depending on factors such as fetal age and the extent of detachment.
The only way to avoid these complications is to minimize the chances of placental abruption.
 Did you know?
Did you know?How To Prevent Placental Abruption?
There is no surefire way to prevent placental abruption. But you can take some measures to reduce your risk of the complication (10).
- Avoid smoking, alcohol and drug abuse

- Avoid medications unless prescribed by your doctor
- Keep your blood pressure levels in check, seek doctor’s help regularly
- Avoid the risk of trauma. Walk carefully, and wear a seatbelt while you travel during pregnancy in a car
- Let your doctor know if you had placental abruption in the earlier pregnancy
- Maintain a good diet and include prenatal supplements as prescribed by your doctor
- Maintain a sleep schedule
Next, we address a few frequent queries from our readers.
Frequently Asked Questions
1. Can heavy lifting cause placental abruption?
Yes, there is a possibility of placental abruption since lifting heavy objects puts a strong force on the abdomen.
2. Can exercise cause placental abruption?
Exercises with a high risk of falls and abdominal trauma can lead to placental abruption.
3. Can stretching cause placental abruption?
No, stretching will not cause placental abruption unless it is severe enough to put a lot of pressure on the abdomen and uterus. Normal stretching will not cause any harm during pregnancy.
4. What is the risk of placental abruption in the second pregnancy without a prior occurrence?
The risk of placental abruption in the second pregnancy, without abruption in the first pregnancy, is 4.7 and 6.5 for 1000 women with same and different partners respectively (11).
5. Can sex cause placental abruption?
Yes, there is a possibility of placental abruption due to sexual intercourse. This might also lead to intrauterine fetal demise (12). Domestic violence has been identified as a risk.
6. What is the fetal mortality rate due to placental abruption?
The perinatal mortality rate due to placental abruption is as high as 60% (13).
7. Can a baby survive a placental abruption?
The baby’s survival depends on two factors – the gestational age at birth and the severity of the condition. If the abruption is detected early and the patient is treated quickly, the chances of the baby’s survival increase (14).
8. Can coughing or sneezing cause placental abruption?
Coughing or sneezing are natural activities for your body, and do not cause placental abruption (14). However, if you have had a cough for a long time or experience a deep, hacking cough, consult your doctor for treatment.
9. Can sonography show placental abruption?
It may be possible that sonography does not show placental abruption (15). Therefore, the condition is usually detected by clinical methods rather than diagnostic tests.
Although placental abruption is a rare occurrence during pregnancy, taking adequate preventive measures and leading a healthy lifestyle can help decrease its risks even further. Keep your blood pressure under check, do not take much stress, get proper sleep, eat healthy and nutritious food to have a risk-free pregnancy, and avert the chances of any complications. But if you notice any signs of pain in the abdominal area or vaginal bleeding, it is advised to consult a medical professional or gynecologist immediately to avoid any serious complications.
Infographic: How To Reduce The Risk Of Placental Abruption?
Placental abruption is a rare pregnancy-related complication that can cause maternal and fetal mortality risk. In addition, it can lead to severe consequences, such as preterm birth and fetal distress. The following infographic outlines some tips to help lower the risk of developing this condition.
Some thing wrong with infographic shortcode. please verify shortcode syntaxLearn about placental abruption and its causes, symptoms, diagnosis, treatment, and pathology. Understand how to recognize the signs and when to seek medical care.
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i. Elizabeth Grace Hundley;
https://babyluke.wordpress.com/2010/08/07/elizabeth-grace-hundley/
ii. Placental abruption – Part of my autism profile;
https://theisaacs22.wordpress.com/2014/09/17/placental-abruption-part-of-my-autism-profile/
iii. Being brain damaged – Is apart of my autism profile – A word that just “is”;
https://theisaacs22.wordpress.com/2015/06/09/being-brain-damaged-is-apart-of-my-autism-profile-a-word-that-just-is/
References
1. B. Gelaye, S. J. Sumner et al.; Maternal Early Pregnancy Serum Metabolomics Profile and Abnormal Vaginal Bleeding as Predictors of Placental Abruption: A Prospective Study; PLoS One (2016)
2. Y Singh, A Shankar, & S Rohatgi; Abruptio Placentae Leading to Fetal Death and Adult Respiratory Distress Syndrome; Med J Armed Forces India (2008)
3. P. Schmidt; D. A. Raines. Placental Abruption (Abruptio Placentae); StatPearls Publishing LLC (2018)
4. Oyelese Y, Ananth CV; Placental abruption; Obstet Gynecol. (2006)
5. Ananth CV, Smulian JC, Vintzileos AM; Incidence of placental abruption in relation to cigarette smoking and hypertensive disorders during pregnancy: a meta-analysis of observational studies; Obstet Gynecol. (1999)
6. Hooria Seyedhosseini Ghaheh et al.; Risk factors of placental abruption; J Res Med Sci (2013)
7. Bleeding in Pregnancy/Placenta Previa/Placental Abruption; The Children’s Hospital of Philadelphia (2018)
8. Placental abruption; Better Health Channel (2018)
9. Ananth C V, Lavery J A; Severe placental abruption: clinical definition and associations with maternal complications; Am J Obstet Gynecol (2016)
10. Placenta abruptio; !!br0ken!! National Library of Medicine (2018)
11. Cande V Ananth et al.; Change in paternity, risk of placental abruption and confounding by birth interval: a population-based prospective cohort study in Norway, 1967-2009; BMJ Open; NCBI
12. Aziken ME; Abruptio placenta following sexual intercourse: case report; Niger Postgrad Med J (2003)
13. Yoshio Matsuda et al.; Prognosis of the Babies Born from Placental Abruption – Difference between Intrauterine Fetal Death and Live-Born Infants; Gynecology & Obstetrics (2013)
14. Placental Abruption; Cleveland Clinic
15. Gauri Raghunath Shinde et al.; Diagnostic Performance of Ultrasonography for Detection of Abruption and Its Clinical Correlation and Maternal and Foetal Outcome; National Library of Medicine; (2016)
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Girija Wagh
Read full bio of Rebecca Malachi
Read full bio of Swati Patwal
Read full bio of Reshmi Das