
Image: ShutterStock
New mothers often get occupied with their babies and overlook their health. However, post-childbirth, a mother’s health is as important as the neonatal health. Ignoring postpartum health could lead to various health conditions like postpartum anemia. In developing nations, women are more likely to develop anemia after delivery, which can have a negative impact on maternal health and in some cases lead to maternal morbidity. Reading this post may help you understand the possible causes, signs, risk factors, and treatment options of postpartum anemia.
Key Pointers
- Postpartum anemia is caused due to severe iron deficiency and is observed in several mothers from developing countries.
- Its onset has three main stages, beginning with depletion of iron in the bone marrow, followed by fatigue and then a drastic drop in hemoglobin levels.
- The condition is usually caused by a poor diet, blood loss, and intestinal diseases.
- The main symptoms are shortness of breath, fatigue, pale skin, and reduced production of breast milk.
- It can be treated with iron supplements, iron-rich foods, foods rich in vitamin C, and adequate hydration.
- Iron supplements, injections, or blood transfusions may be recommended by a doctor in women with severe anemia.
What Is Postpartum Anemia?
Postpartum anemia is chronic iron deficiency post-delivery, when hemoglobin levels are less than 110 g/L at one week postpartum and less than 120 g/L at eight weeks postpartum (1).
Anemia Develops In 3 Stages
- First stage: The iron levels in the bone marrow start to deplete, causing an overall reduction in the iron content in the blood. No specific symptoms of anemia are noticed at this stage.
- Second stage: The side-effects of anemia start to show up. You start feeling more tired and may have headaches. The deficiency can be detected with a blood test. At this stage, the hemoglobin production starts getting affected.
- Third stage: The hemoglobin levels go down further, causing severe anemia. The symptoms include extreme tiredness and exhaustion, making you feel sick (2).
Knowing what brings down the hemoglobin levels is essential to avoid the condition.
What Causes Anemia After Pregnancy?
Postpartum anemia could develop due to (3):
- Poor diet: Insufficient intake of iron before or during pregnancy can lead to postpartum anemia. The iron requirement during pregnancy is 4.4mg per day. Since you do not get enough iron from food alone, it is important to take iron supplements during pregnancy and before conception. Insufficient amounts of vitamin B12 and vitamin B9 (folate) may also result in anemia.

Image: IStock
- Blood loss: Significant blood loss during menstruation can also lead to loss of iron before conception.
- PeripartumiPeriod surrounding childbirth, including the last months of pregnancy and the early postpartum weeks blood loss: Heavy blood loss during delivery (exceeding 300ml) can deplete the body’s iron reserves and lead to anemia after delivery (4). The greater the blood loss, the higher the risk of anemia in the mother.
- Intestinal diseases: In the case of intestinal disorders such as celiac diseaseiAn autoimmune condition where the consumption of gluten causes health issues such as diarrhea, stomach pain, and fatigue , Crohn’s diseaseiA chronic inflammatory and autoimmune condition of the digestive system characterized by pain, diarrhea, and fatigue , and inflammatory bowel diseasei A group of chronic inflammatory digestive disorders, including Crohn's disease and ulcerative colitis , the presence of worms, malabsorption of iron becomes a concern (5).
When the iron levels go down, you will experience certain changes in the body.
Research shows postpartum anemia is frequently linked to maternal morbidity, perinatal morbidity and mortality, small-for-gestational-age (SGA) live birth, and preterm birth. Moreover, anemia is increasingly prevalent and can be a treatable risk factor for preeclampsia. If the hemoglobin levels during pregnancy fall below 7 g/dL, it is associated with higher rates of low birth weight and preterm birth. Therefore, it is crucial to consult with your doctor and take appropriate medications if you experience the symptoms of anemia during pregnancy.
What Are The Symptoms Of Postpartum Anemia?
Here are the signs and symptoms indicating iron deficiency after childbirth (6):
- Feeling overly exhausted and tired
- Pale skin
- Weakness
- Feeling depressed
- Feeling confused
- Reduced quality and quantity of breast milk, which is associated with low weight gain in babies (7)
- Shortness of breath
- Lightheadedness or dizziness
- Rapid heartbeat
- Headaches
- Irritability
- Mood swings

Image: IStock
- Reduced sex drive
- Decreased immunity
You may not be experiencing all these symptoms at a time, but if you find any of the symptoms mentioned above unmanageable, consult your doctor to avoid complications.
Your doctor may do a hematocrit test to identify the percentage of red blood cells in your blood, where the content lesser than 36% indicates anemia. Upon detection, appropriate treatment options will be shared with you.
 Be watchful
Be watchfulRisks Factors For Postpartum Anemia
Women who fall under the following categories are at a greater risk of developing postpartum anemia (8):
- Iron deficiency before or during pregnancy
- Multiple pregnancies
- Pre-pregnancy BMI over 24
- Cesarean section
- Short recovery time between pregnancies
- Bleeding during pregnancy
- Premature or post-term delivery
- High blood loss during pregnancy
- Placenta Previa
- Hypertension
- Multiple births
- Low income (9)
Eritrea Ghebrehiwet, a mother who had just given birth to a beautiful baby, shares her scary experience with a sudden dizzy spell after delivery, “When the nurses were helping me get up to use the bathroom for the first time after delivery, I immediately felt dizzy, heard ringing in my ears, my vision became blurry, and I felt incredibly cold and weak. I was seconds away from passing out. Eventually, the results of my blood work indicated that my hemoglobin count was dangerously low….. I was anemic before pregnancy and didn’t have much iron in my diet. Iron is needed to make hemoglobin…. Thankfully, my anemia didn’t cause any trouble while pregnant.” She incorporated some lifestyle and dietary changes in her day-to-day life to combat the anemia (i).
 Point to consider
Point to considerDoes Anemia Affect Breastfeeding?
Anemia after delivery is associated with insufficient milk syndrome, which brings down the duration of full breastfeeding and leads to weaning at an earlier age. Early weaning also leads to poor weight gain in infants (7). Around 22% of first-time mothers suffer from postpartum anemia, with a hemoglobiniA predominant protein of the red blood cells responsible for transporting oxygen to the body’s tissues level of less than 10 g/L.
Treating anemia soon after diagnosis can prevent breastfeeding problems.
 Point to consider
Point to considerHow Is Postpartum Anemia Treated?

Image: Shutterstock
Treatment of postpartum anemia includes some changes to your diet and lifestyle with recommended iron supplements. If the diagnosis confirms iron deficiency anemia, 100-200mg daily dose of oral ferrous iron is given for women with mild to moderate anemia after childbirth. You may require intravenous ferric iron from 800-1500mg in the case of severe deficiency.
Your doctor will order hemoglobin analysis after two weeks to check if the treatment is successful. Blood transfusion is only given for women who have circulatory problems due to blood loss (4). For more severe forms of anemia, there are various medical treatments that can be implemented under the guidance and supervision of specialists.
Here are a few tips to follow for managing anemia after delivery:
- Iron supplements: Take iron supplements to improve the iron levels in the blood. You can take tablets, capsules, or tonics as recommended by the doctor.
- Eat iron-rich foods including (10):

Image: IStock
- Leafy Greens such as spinach
- Beans
- Lentils
- Apricots
- Pumpkin
- Tofu
- Cereal
- Brown Rice
- Asparagus
- Potato
- Squash
- Peas
- Iron-fortified bread
- Oysters
- Chicken
- Strawberries
- Reduce tea intake: It contains an ingredient called tanniniA group of naturally occurring compounds found in plants, particularly in the leaves, bark, and fruit , which slows down iron absorption in the body. Similarly, a lot of calcium intake can also reduce the absorption of iron in the body (10).
- Eat vitamin C rich foods: Eating foods rich in vitamin C can help increase iron absorption in the body. Fruits like oranges and strawberries are good sources of vitamin C (10).
- Stay hydrated: Drinking more fluids helps you improve your blood flow after childbirth. Fluid intake may also help prevent blood clots and urinary tract infections. If iron supplements cause bloating, then fluids can help tackle it. Have more than three liters of fluids per day during postpartum (11):
- Avoid constipation: Stool softeners can help with constipation, which is a side effect of iron supplements. You can also increase fluid intake to tackle constipation.
- Good rest: Get enough rest and avoid overexertion if you feel very tired and exhausted due to low iron levels.

Image: Shutterstock
- Protect yourself from infections: Infection risk may increase as anemia brings down the immunity level of your body. In case you notice any signs of infection, contact the doctor and take antibiotics if necessary.
- Follow up with the doctor: If you are diagnosed with postpartum anemia. Get blood tests to help the doctor determine your condition and take the necessary steps. If the iron level continues to drop, then the doctor may advise iron injections, IV drip, or a blood transfusion.
Frequently Asked Questions
1. Is postpartum anemia common?
Postpartum anemia is a common problem globally, and its prevalence may often be higher in regions where poor maternal nutrition is commonly observed (12).
2. Can breastfeeding make you anemic?
Breastfeeding is not among the major causes of postpartum anemia. However, studies have shown that iron levels of breast milk are unaffected by maternal iron levels. This may indicate that iron levels of breast milk are met at the expense of the iron stores of the mother (13).
3. How much iron do I need postpartum?
The recommended dietary allowance (RDA) for iron in lactating mothers is 9 mg/day (14).
Postpartum anemia is when the hemoglobin levels are lower than normal in the initial postpartum week. Headaches and tiredness are initial signs of anemia in most women after childbirth. Usually, blood loss related to delivery and poor nutrition or lack of iron in the diet can be the causes of anemia. Women who had placental abnormalities and bleeding during pregnancy may have a higher risk for postpartum anemia. This may also cause breast milk insufficiency in some women. Changes in diet and iron supplements help most mothers to recover from postpartum anemia.
Infographic: Consuming Iron-Rich Foods To Manage Postpartum Anemia
As a new mother, it is vital to prevent postpartum anemia to protect your health and provide sufficient nutrition to your baby. One way to do this is by including iron-rich foods in your diet. Check out this list of foods high in iron to help fight anemia after delivery. Illustration: Momjunction Design Team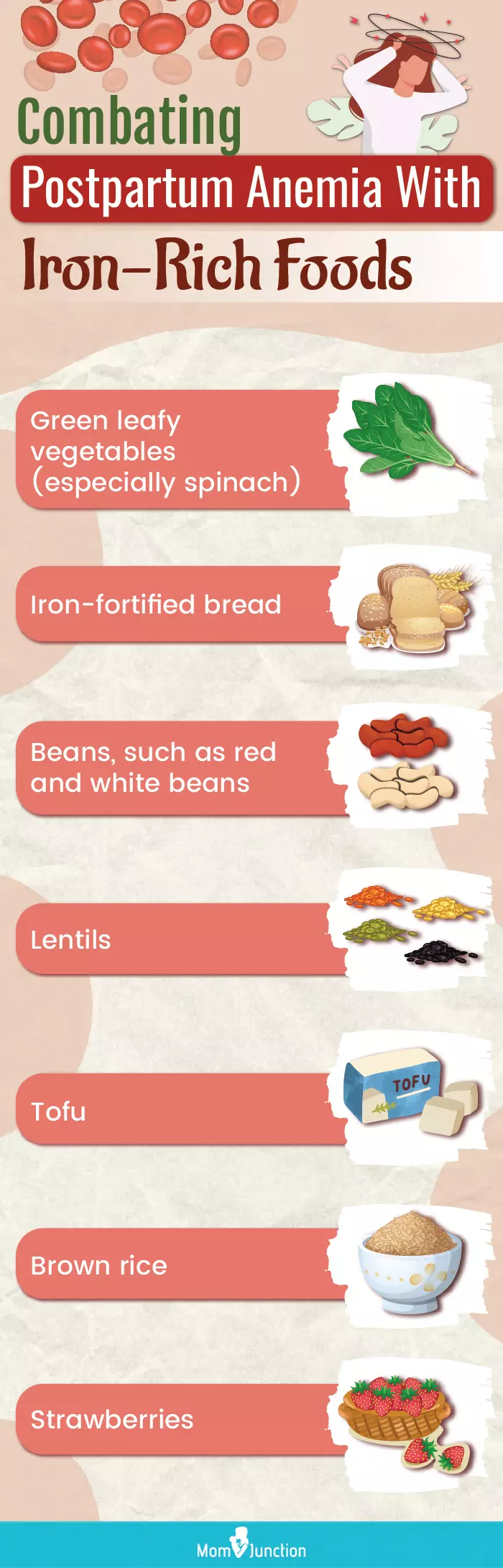
Illustration: Postpartum Anemia: Causes Symptoms And Treatment

Image: Stable Diffusion/MomJunction Design Team
Personal Experience: Source
MomJunction articles include first-hand experiences to provide you with better insights through real-life narratives. Here are the sources of personal accounts referenced in this article.
i.My postpartum experience with low Iron Anemia;https://www.almazandco.com/blog/postpartum-experience-low-iron-anemia
References
1. Milman N; Postpartum anemia I: definition, prevalence, causes, and consequences.
2. Mei Chung, et al.; Biomarkers for Assessing and Managing Iron Deficiency Anemia in Late-Stage Chronic Kidney Disease: Future Research Needs
3. Guideline: Iron Supplementation in Postpartum Women.; Geneva: World Health Organization; 2016
4. Milman N; Postpartum anemia II: prevention and treatment
5. Muhammad Saboor, et al.; Disorders associated with malabsorption of iron: A critical review
6. Markova V, et al.; Treatment for women with iron deficiency anaemia after childbirth; Cochrane
7. Henly SJ, et al.; Anemia and insufficient milk in first-time mothers.
8. Renate L. Bergmann, et al.; Prevalence and risk factors for early postpartum
9. Bodnar LM, et al.; Low income postpartum women are at risk of iron deficiency. anemia; The European Journal of Obstetrics & Gynecology
10. Foods high in iron; Healthdirect
11. Saptawati Bardosono, et al.; Fluid Intake of Pregnant and Breastfeeding Women in Indonesia: A Cross-Sectional Survey with a Seven-Day Fluid Specific Record
12. Alex Mremi et al.; Prevalence of post-partum anemia and associated factors among women attending public primary health care facilities: An institutional based cross-sectional study
13. Yihunie Lakew et al.; Anaemia prevalence and associated factors among lactating mothers in Ethiopia : evidence from the 2005 and 2011 demographic and health surveys
14. Josh M. Jorgensen et al.; Effect of iron supplementation during lactation on maternal iron status and oxidative stress : A randomized controlled trial
15. Nils Milman; Postpartum anemia I: definition, prevalence, causes, and consequences; 2011; NCBI
16. Postpartum Anemia – Still a Major Problem on a Global Scale; Postpartum Anemia – Still a Major Problem on a Global Scale
Community Experiences
Join the conversation and become a part of our nurturing community! Share your stories, experiences, and insights to connect with fellow parents.
Read full bio of Dr. Sangeeta Agrawal
Read full bio of shreeja pillai
Read full bio of Rebecca Malachi
Read full bio of Dr. Joyani Das





















